A stronger association for low-density lipoprotein particle (LDL-P) and high-density lipoprotein particle (HDL-P) versus cholesterol concentrations (LDL-C and HDL-C) in predicting coronary heart disease (CHD) has been noted. We evaluate the role of these factors and extent of particle-cholesterol discordance in those with diabetes mellitus (DM) and metabolic syndrome (MetS) for event prediction. In the Multi-Ethnic Study of Atherosclerosis, we examined discordance of LDL and HDL (defined as a subject’s difference between baseline particle and cholesterol percentiles), LDL-C, LDL-P, HDL-C, and HDL-P in relation to incident CHD and cardiovascular disease (CVD) events in subjects with DM, MetS (without DM), or neither condition using Cox regression. Of the 6,417 subjects with 10-year follow-up, those with MetS (n = 1,596) and DM (n = 838) had significantly greater LDL and HDL discordance compared with those without these conditions. In discordance models, only LDL discordance (per SD) within the MetS group was positively associated with CHD events (adjusted hazard ratio [HR] = 1.22, 95% confidence interval [CI] 1.01 to 1.48, p <0.05). In models with individual particle/cholesterol variables (per SD), within the DM group, HDL-P was inversely (HR 0.71, 95% CI 0.52 to 0.96, p <0.05) and LDL-C positively (HR 1.47, 95% CI 1.07 to 2.03, p <0.05) associated with CHD. In those with MetS, only LDL-P was positively associated with CHD (HR 1.34, 95% CI 1.00 to 1.78, p <0.05). Similar findings were also seen for CVD. LDL discordance and higher LDL-P in MetS, and higher LDL-C and lower HDL-P in DM, predict CHD and CVD, supporting a potential role for examining lipoprotein particles and discordances in those with MetS and DM.
Current guidelines recommend statin therapy in patients with diabetes mellitus (DM) for prevention of cardiovascular disease (CVD). Low-density lipoprotein cholesterol (LDL-C) concentration has been the primary focus of treatment, but many with well-controlled LDL-C levels still have considerable residual CVD risk. Although high-density lipoprotein cholesterol (HDL-C) is inversely associated with coronary heart disease (CHD), it does not fully capture HDL-related CVD risk. Both LDL and HDL particles range in size, densities, and composition. Although HDL particle number and size have been correlated to total HDL-C, the association is complex. HDL particle concentration (HDL-P), but not HDL cholesterol content, is inversely associated with CHD and subclinical disease, and other studies have shown stronger associations of LDL particle concentration (LDL-P) than LDL-C with both subclinical disease and CVD events. Furthermore, studies show that in those with low LDL-C but discordantly high LDL-P or high LDL-C but discordantly low LDL-P, the risk of CVD events is related to LDL-P but not LDL-C. There is, however, a lack of information on the relation of LDL-P and HDL-P on CVD risk prediction in patients with DM and metabolic syndrome (MetS). We hypothesize that the extent of discordance between LDL and HDL particle and cholesterol concentration at the patient level is related to CVD risk in MetS and DM.
Methods
The design of the Multiethnic Study of Atherosclerosis (MESA), a National Institutes of Health–sponsored prospective epidemiologic study of the prevalence, risk factors, and subclinical disease predictors of CVD has been previously published. Briefly, 6,814 multiethnic participants aged 45 to 84 years were recruited from 6 US communities in 2000 to 2002 and were absent of known CVD. Recruitment was based on lists of residents, dwellings, telephone exchanges, lists of Medicare beneficiaries, and referrals by participants. The present study included 6,417 subjects with lipid concentration/particle and required covariates for CVD and CHD event analysis. Institutional review board approval was obtained from all MESA Field Centers.
Age, gender, race/ethnicity, and risk factor information were collected at the baseline MESA examination (2000 to 2002). Smoking was categorized as being either a former smoker (smoked ≥100 cigarettes in lifetime) or current (smoked cigarette in last 30 days). Family history of CHD was defined as a history of “heart attack” in parents, siblings, or child. Blood was drawn after a 12-hour fast and stored at −70°C. Lipids and glucose were measured at a central laboratory. Lipids were assayed on thawed ethylenediaminetetraacetic acid plasma using Centers for Disease Control Prevention/National, Heart, Lung, and Blood Institute standards. HDL-C was measured using the cholesterol oxidase method (Roche Diagnostics, Indianapolis, Indiana) after precipitation of non–HDL-C with magnesium/dextran (coefficient of variation 2.9%). LDL-C was calculated using the Friedewald equation. Plasma lipoprotein particle concentrations were measured at LipoScience, Inc. (Raleigh, North Carolina) by nuclear magnetic resonance spectroscopy. HDL-P and LDL-P (coefficient of variation <4%) are the sums of the particle concentrations of their respective subclasses, quantified from particle size using the amplitudes of their lipid methyl group nuclear magnetic resonance signals, and mean particle sizes are the weighted average of related subclasses.
DM was defined as a fasting glucose ≥7.0 mmol/L (126 mg/dl) or if on insulin or oral DM medications. In those without DM, MetS was defined with ≥3 of the following: (1) waist circumference >88 cm (35 in) for women and >102 cm (40 in) for men, (2) HDL-C <1.0 mmol/L (40 mg/dl) for men or <1.3 mmol/L (50 mg/dl) for women, (3) fasting triglycerides ≥1.7 mmol/L (150 mg/dl), (4) blood pressure (BP) ≥130 mm Hg systolic or ≥85 mm Hg diastolic or on treatment, or (5) fasting glucose of 5.6 to 7.0 mmol/L (100 to 125 mg/dl), based on the American Heart Association/National Heart, Lung, and Blood Institute definition. Those not defined as having DM or MetS were categorized into the neither disease group.
Incident CHD (myocardial infarction, CHD death, resuscitated cardiac arrest, definite angina or probable angina followed by revascularization) and CVD events (CHD, fatal or nonfatal stroke, or other atherosclerotic CVD death) were ascertained and adjudicated for MESA as previously described. Follow-up time for those experiencing events was defined from the baseline examination date to the date of the first qualifying event. Those without an event were followed to death (from non-CVD causes), last follow-up, or the end of the study, after which they were censored.
Analyses were performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina). For patients with DM, MetS without DM (MetS), and neither disease group, we compared baseline laboratory values and cardiovascular risk factors using the chi-square test for categorical variables and the Student’s t test or ANOVA for continuous variables. Percentile distributions of LDL-P, LDL-C, HDL-P, and HDL-C were calculated from the study sample. LDL and HDL discordance was defined as a subject’s difference between respective baseline lipoprotein particle and cholesterol percentiles (e.g., LDL-P% – LDL-C%). The Student’s t test was used to calculate significance among groups (MetS, DM, or neither condition) for mean LDL and HDL discordance. Incident CHD and CVD event rates were calculated by quartile of discordance for both LDL and HDL discordance among the 3 groups.
Cox proportional hazards regression provided hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for CHD and CVD events. HDL-C, HDL-P, LDL-C, and LDL-P were each separately modeled with adjustments for baseline age, gender, race/ethnicity, family history, systolic BP, BP medication, smoking, body mass index, and statin use in each of the 3 groups and among all participants. Three separate models were conducted for all participants together and then for each of the 3 groups using the above covariate adjustments. Model 1 examined the continuous HDL discordance variable, adjusted for LDL-C and LDL-P. Model 2 examined the continuous LDL discordance variable, adjusted for HDL-C and HDL-P. Model 3 examined the variables of HDL-C, HDL-P, LDL-C, and LDL-P separately but in the same model. All 3 models reflect adjustments for both particle and cholesterol concentration variables similar to previous studies. All HRs were reported per SD to allow for direct comparison. Interaction between each LDL or HDL discordance, particle, and cholesterol variable with group variables were evaluated for significance. Interactions with gender and race/ethnicity were also examined. Sensitivity analyses were conducted for models 1 to 3 among all study groups, excluding patients with a history of statin use or hormone therapy at baseline and, separately, with the additional adjustment for excessive alcohol use (>14 drinks/week) and exercise (minutes/week).
Analysis involving dichotomous discordance (compared with continuous discordance analysis) as studied by others involv categorizing individuals as < or ≥ median levels of LDL-C. Discordance was defined as LDL-C greater than or equal to median and LDL-P less than the median level, or vice versa. This was also done for discordance groups between HDL-C and HDL-P. Risk factor–adjusted Cox regression was also used for discordantly high cholesterol/low particle groups versus high cholesterol/high particle groups.
Results
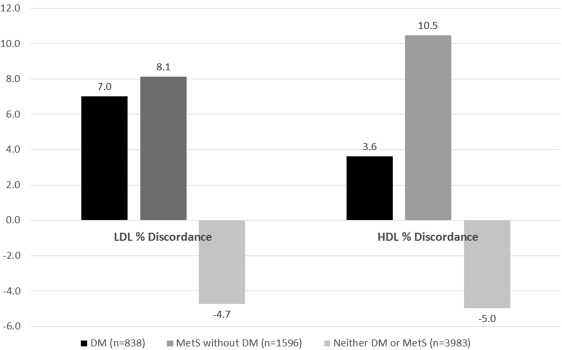
Table 1 lists significant differences in baseline covariates among the 3 study groups. Both HDL-C and HDL-P were higher in participants without MetS or DM compared with neither disease (p <0.001). LDL-P was lower in those with neither disease compared with both disease groups (p <0.001). Mean (SD) LDL discordance (LDL-P percentile − LDL-C percentile) among groups were 7.0 (21.3) for DM, 8.1 (19.3) for MetS alone, and −4.7 (19.4) for those with neither disease. LDL discordance differed across all groups (p <0.001), except comparing DM and MetS (p = 0.20) ( Figure 1 ). Mean HDL discordance (HDL-P percentile − HDL-C percentile) among groups were 3.6 (22.7) for DM, 10.5 (19.4) for MetS alone and −5.0 (19.5) for those with neither disease (p <0.001 between groups).
| Characteristic | MetS without DM (N=1596) | DM (N=838) | Neither DM nor MetS (N=3983) |
|---|---|---|---|
| Mean ± SD or N (%) | |||
| Age (years) ∗ | 63.1 ± 10.0 | 64.7 ± 9.6 | 61.2 ± 10.3 |
| Male | 656 (41.1 %) | 438 (52.3 %) | 1957 (49.1 %) |
| Female | 940 (58.9 %) | 400 (47.7 %) | 2026 (50.1 %) |
| White | 644 (25.9 %) | 157 (6.3 %) | 1683 (67.8 %) |
| Black | 150 (19.4 %) | 102 (13.2 %) | 522 (67.4 %) |
| Hispanic | 407 (23.0 %) | 325 (18.4 %) | 1034 (58.6 %) |
| Chinese American | 395 (28.4 %) | 254 (18.2 %) | 744 (53.4 %) |
| Systolic BP (mm Hg) ∗ | 133.6 ± 20.6 | 133.0 ± 22.2 | 122.2 ± 20.6 |
| BP Medication ∗ | 760 (47.6 %) | 472 (56.3 %) | 862 (21.6 %) |
| BMI (kg/m 2 ) ∗ | 30.8 ± 5.1 | 30.3 ± 5.8 | 26.7 ± 4.9 |
| Cholesterol (mg/dLL) ∗ | 195.8 ± 35.5 | 188.0 ± 37.5 | 193.8 ± 33.6 |
| Triglycerides (mg/dLL) ∗ | 172.5 ± 68.6 | 144.4 ± 73.6 | 102.9 ± 49.0 |
| Smoker | 790 (49.6 %) | 422 (50.4 %) | 1954 (49.2 %) |
| Family History of CHD † | 688 (43.1 %) | 320 (38.2 %) | 1549 (38.9 %) |
| Statin Use ∗ | 259 (16.2 %) | 208 (24.8 %) | 470 (11.8 %) |
| HDL-C (mg/dl) ∗ | 43.2 ± 10.2 | 46.8 ± 13.2 | 55.2 ± 15.1 |
| HDL-P (μmol/l) ∗ | 32.6 ± 6.4 | 32.7 ± 6.3 | 34.8 ± 6.7 |
| LDL-C (mg/dl) ∗ | 118.1± 32.3 | 112.3 ± 33.4 | 118.0 ± 30.5 |
| LDL-P (μmol/l) ∗ | 1354.3 ± 354.9 | 1264.8 ± 344.9 | 1199.2 ± 313.3 |
Of the 6,417 subjects, 462 subjects experienced CHD events and 659 subjects CVD events over an average 10-year follow-up. HDL discordance (model 1) was not predictive among the 3 study groups for either CHD or CVD ( Table 2 ); however, in the entire sample, higher levels of HDL discordance were associated with decreased CHD (HR 0.90, 95% CI 0.81 to 1.00, p <0.05) and CVD (HR 0.90, 95% CI 0.83 to 0.99, p <0.05) events. Similar results were seen in sensitivity analyses in those without previous statin or hormone therapy use for CHD (HR 0.86, 95% CI 0.76 to 0.98, p <0.05) and CVD (HR 0.88, 95% CI 0.79 to 0.98, p <0.05); additionally, HDL discordance was associated with decreased CHD and CVD within the DM group. LDL discordance (model 2) was positively associated with CHD and CVD in the MetS group only but attenuated in sensitivity analyses excluding those with statin or hormone therapy use. When adjusting for the standard baseline covariates, interaction terms of HDL and LDL discordance variables with group, gender, and race/ethnicity variables were found to be insignificant.
| Variable | Hazard ratio (95% confidence interval) per standard deviation | ||
|---|---|---|---|
| MetS (without DM) (N= 1596) | DM (N= 838) | Neither DM nor MetS (N=3983) | |
| CHD Events | 139 | 105 | 218 |
| Model 1 ‡ : HDL Discordance | 0.84 (0.68-1.04) | 0.88 (0.72-1.08) | 0.94 (0.80-1.10) |
| Model 2 § : LDL Discordance | 1.21 (1.01-1.47) ∗ | 0.88 (0.71-1.10) | 0.87 (0.74-1.02) |
| Model 3 ‖ : | |||
| HDL-C | 1.12 (0.73-1.73) | 1.00 (0.70-1.43) | 1.14 (0.90-1.45) |
| HDL-P | 0.86 (0.63-1.17) | 0.71 (0.52-0.96) ∗ | 0.82 (0.66-1.03) |
| LDL-C | 0.80 (0.59-1.08) | 1.47 (1.07-2.03) ∗ | 1.27 (1.01-1.59) ∗ |
| LDL-P | 1.34 (1.01-1.78) ∗ | 0.82 (0.58-1.17) | 0.93 (0.71-1.22) |
| CVD Events | 200 | 152 | 307 |
| Model 1 ‡ : HDL Discordance | 0.95 (0.80-1.13) | 0.90 (0.77-1.06) | 0.88 (0.77-1.01) |
| Model 2 § : LDL Discordance | 1.26 (1.07-1.47) † | 0.88 (0.74-1.06) | 0.91 (0.79-1.04) |
| Model 3 ‖ : | |||
| HDL-C | 1.05 (0.74-1.48) | 0.98 (0.73-1.32) | 1.12 (0.92-1.37) |
| HDL-P | 0.97 (0.76-1.25) | 0.75 (0.58-0.97) ∗ | 0.80 (0.66-0.96) ∗ |
| LDL-C | 0.77 (0.60-1.00) | 1.41 (1.08-1.84) ∗ | 1.17 (0.96-1.42) |
| LDL-P | 1.39 (1.09-1.75) † | 0.76 (0.57-1.02) | 0.99 (0.79-1.24) |
‡ Model 1 additionally adjusted for LDL-C and LDL-P.
§ Model 2 additionally adjusted for HDL-C and HDL-P.
‖ Model 3 include simultaneous adjustment with all four lipid variables.
Figure 2 shows with each increasing quartile of LDL discordance, there is a graded increase CHD and CVD event rates; this association with CHD was strongest in those with MetS ( Figure 3 ) but is less clear within the DM or neither disease groups. In the overall sample, there was no association between HDL discordance quartiles and CHD and CVD events ( Figure 2 ). However, when evaluated by group, those with DM had lower event rates with higher levels of HDL discordance ( Figure 3 ).





