Chapter 89 Diagnostic Aspects of Implantable Devices
Monitoring of Atrial Fibrillation
Atrial tachycardias and atrial fibrillation (AT/AF) are significant components of the global burden of cardiovascular disease and their incidence is increasing rapidly because of the aging of the population; projections indicate that the prevalence of AF could exceed 12 million in the United States by 2050.1 These conditions occur concomitantly with bradycardias, supraventricular tachycardias, and ventricular tachyarrhythmias and are frequently observed in populations with these conditions when an implantable device is prescribed therapeutically.
Atrial tachyarrhythmias result in poor quality of life for patients, as they may cause symptoms of tiredness, palpitations, and dizziness. However, in many patients, AT/AF episodes can be completely asymptomatic.2,3 Whether it is symptomatic or asymptomatic, AT/AF also increases the risk of stroke in the presence of clinical risk factors, and it is estimated that 1 out of every 6 strokes occurs in patients with AT/AF.4 It leads to more hospital admissions than any other arrhythmia and increases mortality rates.5,6 Management of this arrhythmia with pharmacologic agents, ablation, and implantable devices requires accurate assessment of the arrhythmia at baseline and after treatment. Regardless of the AF treatment strategy chosen, diagnostics from implantable devices can provide valuable information to help evaluate treatment efficacy and guide clinical decisions. Other important clinical imperatives for monitoring include the following:
Symptoms Versus External Recorders
Monitoring AT/AF on the basis of patient symptoms is appealing because it is relatively inexpensive and has clinical relevance. However, studies have shown that the vast majority of AT/AF episodes are asymptomatic and that most symptoms attributed to AT/AF are not actually associated with arrhythmia.2,3,8,9 Therefore, even if supplemental event recorders are used to verify the presence of an arrhythmia during symptoms, most atrial arrhythmias will escape detection because of lack of symptoms. Since the risk of stroke is similar among patients with symptomatic and asymptomatic AT/AF, current anticoagulation guidelines do not differentiate on the basis of symptoms,10 which emphasizes the importance of identifying asymptomatic AT/AF.10–12
Because of the highly insensitive and nonspecific nature of patient symptoms, external devices were developed to monitor asymptomatic episodes of AT/AF. External devices such as Holter monitors are commonly used to continuously record cardiac data for 24 or 48 hours. Newer systems, such as mobile cardiac outpatient telemetry, are capable of monitoring patients continuously for up to 30 days and have been shown to increase the yield for arrhythmia detection compared with a single 24-hour Holter monitor.13,14 These systems have the benefits of moderate cost and being a noninvasive procedure. However, these external devices often are bulky and interfere with daily activities such as showering. In addition, the patch electrodes can cause skin irritation with prolonged use. Consequently, patient compliance with such systems often is quite low.8,13 Furthermore, since external monitoring can only be performed intermittently over time and for relatively brief durations, the likelihood of missing paroxysmal episodes of asymptomatic AT/AF episodes is quite high.
Implantable Monitors
Therapy Devices
Devices such as implantable pulse generators, implantable cardioverter-defibrillators (ICDs), and cardiac resynchronization therapy (CRT) devices are capable of monitoring arrhythmias continuously over the lifetime of the device with a high sensitivity as well as a high specificity for AT/AF detection.15,16 Although these devices require an invasive implantation procedure, patient compliance is generally not an issue, and these devices rarely interfere with normal daily activities. Patients can communicate with many modern implantable devices via an external activator to record the occurrence of symptoms in the memory of the device. This symptom information can be retrieved later by the clinician when the device is interrogated via telemetry. However, the monitoring capabilities afforded by these sophisticated devices are available only to those AF patients with comorbid conditions requiring device therapy.
Subcutaneous Monitors
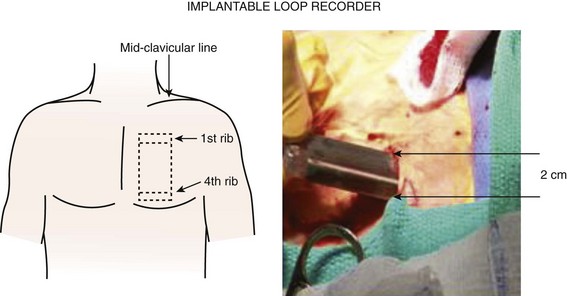
One strategy to address the need for continuous monitoring in a broader population of patients with AF is to use small implantable devices that are capable of monitoring atrial arrhythmias continuously over the lifetime of the device with a high sensitivity and a high specificity for AT/AF detection.17 These devices, about the size of a cigarette lighter, do not have intracardiac leads, as the bipolar recording electrodes are generally located on the surface of the device itself. These monitoring devices are placed subcutaneously, are relatively small in size (3 to 5 cm), and are typically implanted in the left pectoral region in the precordial area, though axillary implants have been described (Figure 89-1, A). Implantation parallel to and in an intercostal space is most desirable for avoidance of local erosion and aesthetics. A local anesthetic agent is infiltrated at the site of entry and in the adjoining subcutaneous tissue where the device pocket will be made. Typically, a small (1 to 2 cm) vertical or horizontal incision is made at one end of the pocket, and the pocket created by blunt dissection (Figure 89-1, B). The device is placed and the electrogram quality assessed using a hand-held wand or wireless connection by the device programmer. If clear electrogram quality and satisfactory amplitude are obtained, the pocket can be closed. If not, device repositioning is needed so that the surface electrodes have an appropriate vector to obtain quality recordings. Although a small skin incision is required to implant these devices, patient compliance is not an issue, as these devices rarely interfere with normal daily activities. Until recently, subcutaneous monitoring devices had only been available for the diagnosis of syncope, but they have now become available for the monitoring of atrial arrhythmias as well. Patients are able to record the occurrence of symptoms in the memory of the device with an external activator, and these data can be retrieved later by the clinician.
Comparison of Monitoring Methods
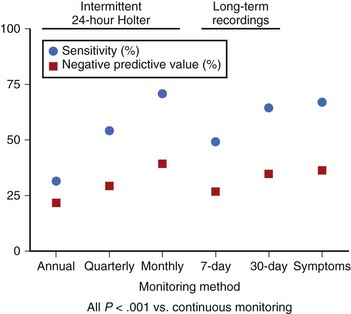
Methods of identifying patients with AT/AF through their symptoms, intermittent external monitoring, and continuous monitoring with implantable devices have been compared in a recent study.18 Symptom-based and intermittent external monitoring methods were shown to have significantly lower sensitivity (range, 31% to 71%) and negative predictive value (range, 21% to 39%) for identification of patients with AT/AF (Figure 89-2) and underestimated AT/AF burden, compared with continuous monitoring. The reported efficacy of clinical procedures such as pulmonary vein ablation for the treatment of AT/AF can vary greatly, depending on how the arrhythmia is monitored. One study reported a success rate of 70% on the basis of symptoms alone and only 50% when intermittent external monitoring was also considered.8 These results were achieved despite the fact that 47% of the patients did not complete the external monitoring protocol and compliance with the monitoring schedule was only 42%. Such results highlight the clinical need for continuous monitoring that does not rely on patient symptoms or patient compliance.
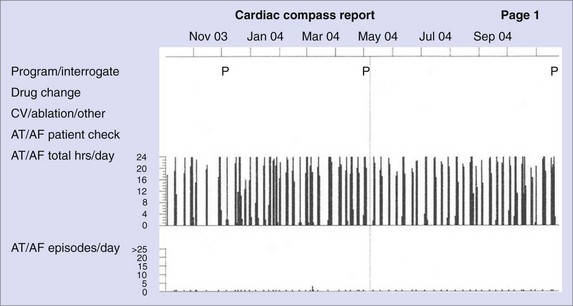
Rhythm Control
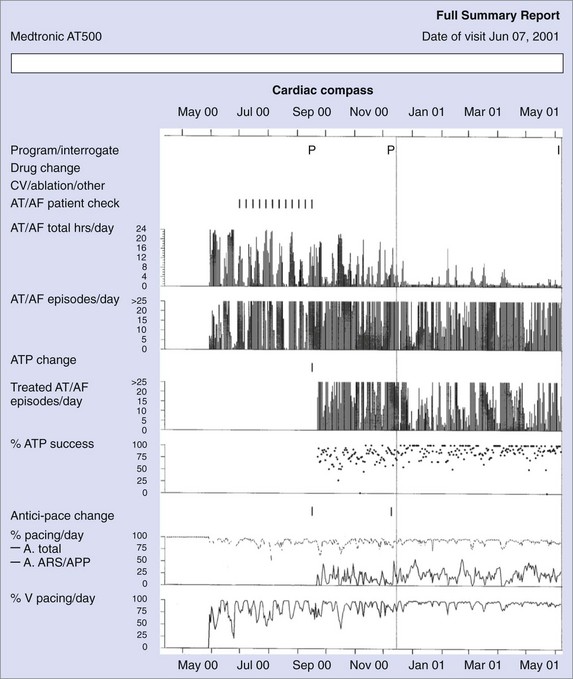
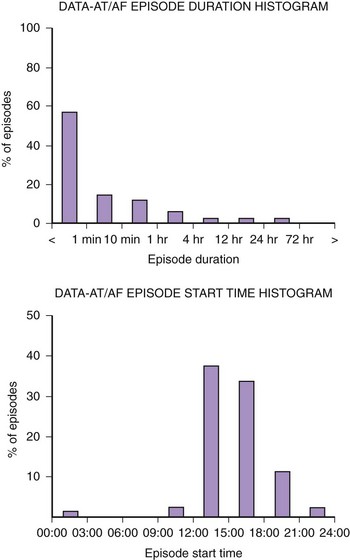
Figure 89-3 shows diagnostic information that can be used to evaluate the efficacy of rhythm control. The total hours of AT/AF per day (AT/AF burden) can be continuously monitored over a period of 14 months before the data get overwritten. Other diagnostics that can provide additional rhythm control clarity are an AT/AF episode duration histogram, episode start time histogram (Figure 89-4), and the duration of the longest episode.
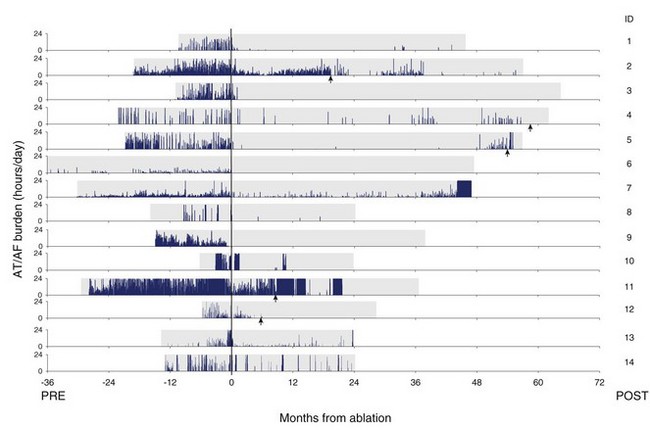
Pulmonary Vein Ablation
Figure 89-5 shows a series of patients who were treated for AT/AF by undergoing a pulmonary vein ablation procedure anywhere from 6 to 36 months after device implantation. These patients had a pacemaker implanted for their bradycardia, and the device was subsequently used to monitor the effectiveness of the ablation procedure. Patient data are aligned such that the date of ablation corresponds with month 0. The amount of AT/AF experienced each day is plotted over the follow-up period and shown in blue. Despite an improvement in symptoms and quality of life in all patients after the ablation, many still experienced significant amounts of AT/AF.19 This example also illustrates that after an ablation procedure, patients can go for many months without an AT/AF episode and subsequently experience recurrences that would be difficult to record with intermittent monitoring methods. This long-term trending information enabled the physicians conducting the study to perform additional ablation procedures (indicated by the red arrows) in select patients who did not respond completely to the initial procedure.
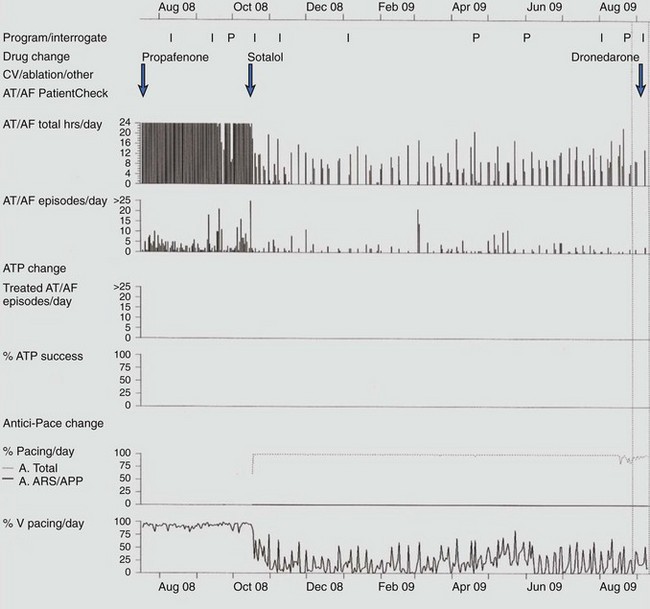
Antiarrhythmic Drugs and Cardiac Pacing
Response to antiarrhythmic drug therapy can be assessed by device-based diagnostic data. Figure 89-6 shows an example of change in AT/AF burden, with conversion of persistent AF to paroxysmal AF, after the initiation of sotalol. The patient continued to have symptomatic paroxysmal AF and was then transitioned to dronedarone, which resulted in the resolution of symptomatic paroxysmal AF.
Recurrence Patterns
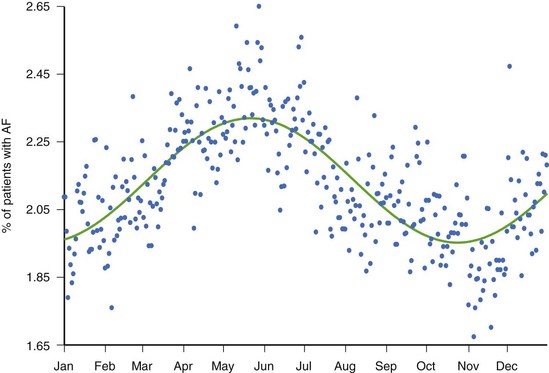
While there is clinical value in knowing whether or not a patient has experienced AT/AF and the percentage of time that has been spent in AT/AF, understanding the pattern of these AT/AF recurrences may be of additional value. The patient data in Figure 89-7 show a very consistent recurrence pattern that persists for the entire 14-month period covered by device diagnostics. On closer examination, it was found that this patient experienced AT/AF predominantly on weekends, with episodes generally initiating on Fridays or Saturdays and typically terminating on Sundays or Mondays. With intermittent arrhythmia monitoring, it might have been erroneously concluded that this patient was either always in AT/AF or always in sinus rhythm, depending on the day(s) selected for monitoring. With continuous monitoring, a more complete picture of the patient’s arrhythmia can be obtained, which may provide additional insight into the patient’s disease and lead to different treatment strategies. In addition to providing more complete information on individual patients, device diagnostics can inform us on the nature of atrial arrhythmias across entire populations. Figure 89-8 shows the percentage of patients with implantable devices (pulse generator, ICD, and CRT) who experienced at least 5 minutes of AT/AF over each day of the year.20 A clear pattern is seen, with a peak incidence in the month of May and a minimum incidence 6 months later in November. While the underlying cause of this cyclic variation is not fully understood, it is interesting to note that the occurrence of stroke has been shown to exhibit a similar recurrence pattern.21
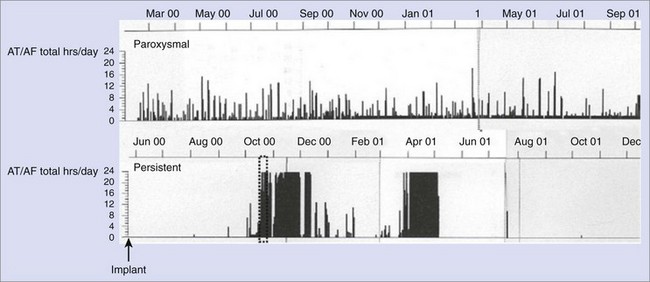
Transition from Paroxysmal Atrial Fibrillation to Persistent Atrial Fibrillation
AT/AF recurrence patterns are not static and may change over time as the disease progresses or as new treatments are applied. Device diagnostics have shown that the transition from paroxysmal AT/AF to more persistent forms of AT/AF can occur relatively abruptly (Figure 89-9).22,23 This finding is consistent with changes in the substrate as opposed to an increase in atrial premature beat triggers or paroxysmal AT/AF episodes. This monitoring approach shows the progression of persistent AF events as well as promotes understanding of the disease state.23 Device diagnostics can heighten the awareness of this sudden change in the arrhythmic state so that a change in treatment strategy can be implemented in a timely manner.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree