Fig. 12.2 A gross example of Wolff–Parkinson–White (WPW) syndrome. The PR interval is very short (look at leads V1–6), and the QRS upstroke is very slurred, due to the delta wave. The QRS complex is positive in lead V1, so the pathway is left sided (Fig. 12.1b); the inferior leads show negative QRS complexes inferiorly so this is a left-sided postero-septal pathway.
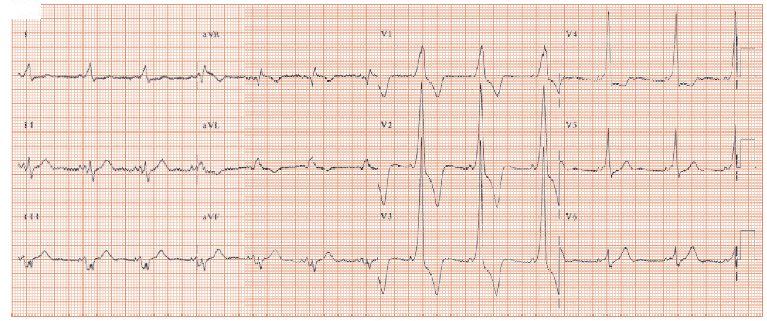
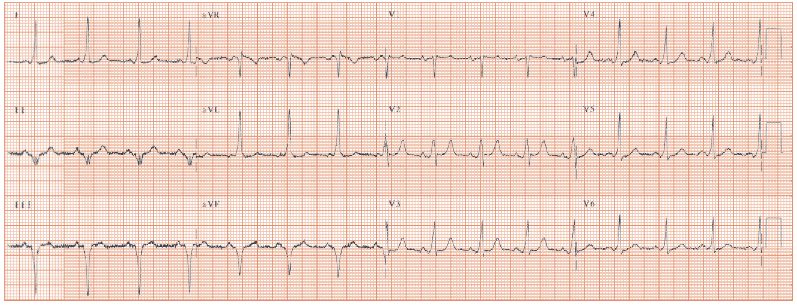
Fig. 12.3 Wolff–Parkinson–White (WPW) syndrome; much more subtle than in Fig. 12.2. At first glance this looks like an old inferior wall Q wave myocardial infarction (MI) (Q waves in leads II, III and aVF), with left ventricle (LV) hypertrophy (aVL = 15 mm, normal < 11 mm). However, further inspection reveals small and rather subtle delta waves, with a short PR interval, especially in the antero-lateral chest leads (V2–6). This is WPW syndrome with a right-sided pathway (lead V1 complex is negative); the inferior wall MI is not real, the ECG pattern is termed ‘pseudo-infarction’ and the Q waves disappear when the pathway is ablated.
Delta waves are pathognomonic of the Wolff–Parkinson–White (WPW) syndrome, and are due to early ventricular activation from an accessory pathway bypassing the atrioventricular (AV) node.
Mechanism of the delta wave
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


