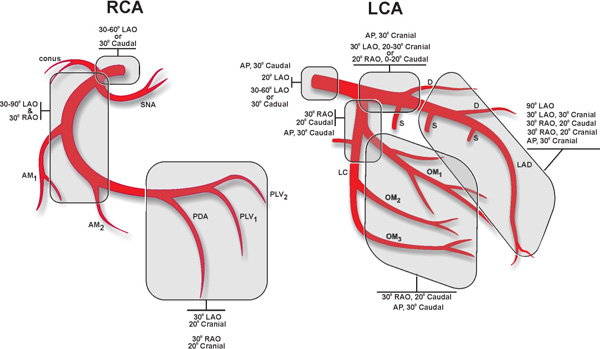
CHAPTER 6 “Follow the rules, but avoid turning those rules into dogmas.” —Anonymous Selective coronary angiography provides two-dimensional (2D) images of the three-dimensional (3D) coronary circulation. In order to better assess the presence and severity of coronary atherosclerosis in any particular segment of the coronary tree, the angiographer should use multiple angiographic views.1-3 In general, there are certain standard views that provide optimal visualization of the particular coronary segment (Figure 6.1). Every angiographer should keep in mind that with each individual patient, he or she may need to slightly modify these standard views in order to obtain the optimal angiographic image. FIGURE 6.1These standard angiographic views are used to visualize different segments of the coronary circulation. The general indications and contraindications for left heart catheterization are listed in Tables 6.1 and 6.2. TABLE 6.1Indications for left heart catheterization and coronary and peripheral angiography.
Coronary, Renal, and Mesenteric Angiography
Angiographic Views and Projections
Indications and Contraindications of the Procedures
Acute myocardial infarction | Particularly in individuals who will undergo PCI, are in cardiogenic shock, or have hemodynamic instability or mechanical complications and will need surgery. Persistent pain or unresolved ECG changes after thrombolytic therapy. 1.In NSTEMI patients, if:
2.Previous PCI in past 6 months |
Unstable angina | Refractory to medical therapy |
Chronic stable angina | Refractory to medical therapy or intolerant of antianginal therapy |
Abnormal stress test | With high-risk criteria, even if asymptomatic
|
Ventricular tachycardia | Sustained |
Left ventricular dysfunction | LVEF ≤ 40% of unknown cause |
Valvular heart disease | Provide confirmatory data to Echo to assess outflow tract obstruction and quantify aortic and mitral regurgitation, and rule out CAD in preoperative work-up. |
Preoperative assessment | Based on ACC/AHA/ESC guidelines. Also, before ascending aortic aneurysm or dissection surgery, as well as in patients with congenital heart disease, to assess shunts or to rule out coronary anomalies. |
Hypertension |
|
TABLE 6.2Relative contraindications for left heart catheterization and coronary and peripheral angiography.*
Coagulopathy | For elective cases, INR < 1.8; heparin stopped 2 hours prior; platelets < 50,000 cells/mL |
Renal failure | In dialysis patients, catheterization is generally scheduled after dialysis |
Contrast allergy | |
Infection | |
Laboratory abnormalities | Anemia, hypokalemia, hyperkalemia |
Decompensated heart failure | |
Severe peripheral vascular disease | Synthetic vascular grafts younger than 6 months warrant special care; older vascular grafts increase risk of embolization of friable atheroma or thrombus |
Severe bleeding can occur if BP > 180/100 mm Hg | |
* All contraindications are relative contraindications. | |
Selective Cannulation of the Native Left Coronary Artery (LCA)
JUDKINS LEFT CORONARY CATHETER FOR FEMORAL, LEFT BRACHIAL, AND RADIAL APPROACHES
The Judkins Left (JL) catheter is a preformed catheter specifically designed to cannulate the ostium of the LCA without major manipulations. Clockwise and counterclockwise torque of the catheter will address an anterior and posterior orientation of the ostium of the left coronary artery (LCA) vessel, respectively. Superior or inferior position of the ostium should be managed through manipulation of the catheter in the vertical plane, or by changing the size of the catheter. In general, in patients with a normal-size aortic root, a JL4 catheter is used. In very tall patients (over 6 feet, 3 inches) or patients whose aortic root is known to be enlarged, JL5 or even JL6 may be tried from the start. Under fluoroscopic guidance, the operator advances the catheter over the J-tip guidewire through the arterial sheath to the aorta, keeping the tip of the wire protruding beyond the tip of the catheter in order to decrease the chance of aortic wall damage (retrograde dissection) and risk of distal embolization. Once the tip of the wire advances around the aortic arch, it is fixed above the sinotubular junction. The catheter slides over the wire until the tip of the wire is covered by the tip of the catheter, at which point the wire is withdrawn gently (to avoid abrupt “jump” of the catheter tip into the LCA ostium). A 5- to 10-mL syringe is attached to the proximal hub of the catheter, and 1–2 mL of blood is aspirated in order to clear the catheter from potential debris accumulation. If the operator has problems aspirating blood, gentle withdrawal of the catheter usually helps. The proximal end of the catheter is then attached to the manifold, and about 2 mL of blood is aspirated into the attached syringe, keeping the syringe at 45- to 60-degree angle elevation and simultaneously tapping gently on the manifold in order to remove potential air bubbles in the system. The catheter is flushed with normal saline, and aortic pressure is recorded.
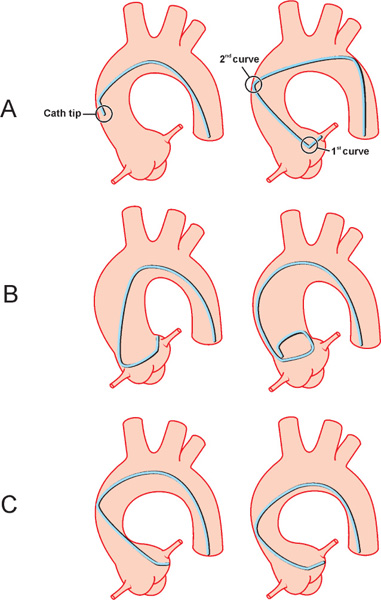
Once pressure waves are recorded, the catheter is advanced under fluoroscopic guidance in a left anterior oblique (LAO) caudal view and with constant monitoring of aortic pressure. In the majority of patients, the tip of the catheter easily cannulates the ostium of the LCA; this can be noted on screen by a sudden “dive” of the catheter tip (Figure 6.2A). Occasionally, when the wire is being removed, the JL4 catheter folds into the aorta due to a very large aortic root and requires straightening and removal over the guidewire (Figure 6.2B). In the presence of normal pressure waveforms, the operator proceeds with 1–2 mL of contrast test injection under fluoroscopic guidance in LAO caudal projection. If the JL4 catheter ends up somewhat proximal to the ostium of the LCA, the operator can try the following approaches: First, a half-turn, clockwise rotation of the catheter with simultaneous slight advancement will work in cases where the tip of the catheter is not far from the ostium. However, if the tip is too far, the operator can either try to rewire the catheter all the way to the left coronary cusp (LCC) and, after removing the wire, attempt cannulating the ostium on slow catheter withdrawal. Alternatively, the catheter can be upsized to a JL5 or JL6. If the JL4 catheter tip ends distal to the ostium, counterclockwise rotation and slight withdrawal of the catheter often cannulates the ostium of the artery (Figure 6.2C). In other instances, the catheter should be downsized to a JL3.5 or even to a JL3.
FIGURE 6.2Schematic drawings show the steps and potential difficulties in engaging the LCA with a JL catheter. Panel A, a sudden “dive” of the catheter tip; Panel B, folding of the catheter into the aorta; Panel C, cannulation of the ostium of the artery after rotation and withdrawal (see text for details).
In some cases, the ostium of the LCA has posterior, superior, or inferior orientation and is not engaged easily with a standard JL4 approach. Alternative catheters such as Amplatz Left (AL), JL3.5, or JL5 catheters may become handy. When the ostium of the LCA is intubated, pressure waves are observed to avoid “damping” (drop of amplitude of systolic pressure) (Figure 6.3A) or “ventricularization” (change in shape of aortic diastolic pressure form) (Figure 6.3B).
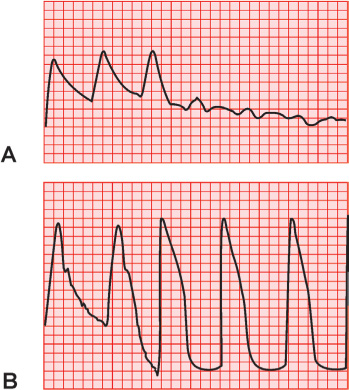
FIGURE 6.3Hemodynamic patterns observed include “damping” (Panel A) and “ventricularization” (Panel B).
This is followed by efforts applied to place the tip of the catheter coaxial to the body of the left main (LM) trunk by advancing or withdrawing the catheter (Figure 6.4 A–B).
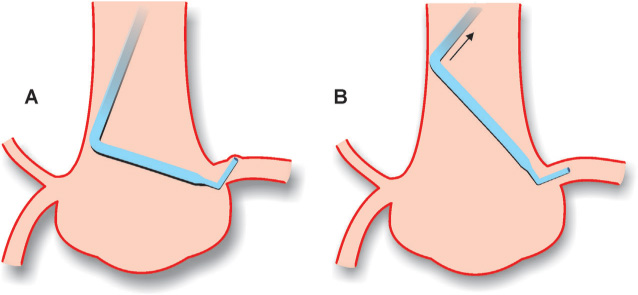
FIGURE 6.4The potential problems illustrating the importance of coaxial positioning of the catheter tip in the LCA ostium are shown. In Panel A, incorrectly placed catheter against the vessel wall. Correct placement is shown in Panel B.
Once the catheter tip is placed coaxially with the LM trunk and the pressure tracing is appropriate, the operator sets the camera in right anterior oblique (RAO), 30-degree view with caudal 30-degree angulation view for the opening shot. The tip of the catheter on the fluoroscopic image screen is placed at a 10- to 11-o’clock position. The opening shot can be obtained using another view, if the operator chooses to do so based on clinical and previous angiographic data. The operator initiates cineangiography, turns off pressure, and injects 5–7 mL of contrast dye into the coronary artery under an initial slow rise, but using steady and constant pressure to opacify the coronary vessel lumen and to avoid streaming. Occasionally, prior to contrast injection a patient may be asked to hold his/her breath on maximal inspiration. This maneuver can reduce proximal vascular tortuosity and straighten the proximal vessel bends. When all of the appropriate images are obtained, the JL catheter is gently withdrawn below the aortic arch, the proximal end of the catheter is disconnected from the manifold, a 5- to 10-mL syringe is attached to the proximal hub of the catheter, and 1–2 mL of blood is aspirated. The operator advances the J-tip guidewire through the catheter under fluoroscopic guidance until the tip of the wire protrudes beyond the tip of the catheter, followed by simultaneous catheter and wire removal from the body through the arterial sheath. The arterial sheath is flushed with heparinized saline in the usual manner.
When utilizing the left brachial or radial approach, the operator may experience occasional difficulties placing the JL catheter due to the inability to navigate the J-tip guidewire into the ascending aorta. Certain maneuvers, such as turning the patient’s head to the right, removing the pillow, extending the neck, abducting the left arm further from the body, performing the Valsalva maneuver, or just asking the patient to take a deep breath may facilitate guidewire placement and advancement of the catheter over the guidewire. If these maneuvers fail, a long, J-tip guidewire and the JR catheter can be used to navigate the wire towards the ascending aorta and subsequently exchange the JR for a JL catheter (Figure 6.5). This is technically accomplished in the following fashion: After the guidewire tip enters the aortic arch, it gets fixed, and the JR catheter runs over until it covers the tip of the guidewire. Then the operator, using the fingers of both hands, turns the catheter a half-turn clockwise until the tip of the catheter points towards the right shoulder of the patient. Next, the guidewire is advanced in the direction of the ascending aorta and down to the sinotubular junction. The JR catheter is removed, and the JL catheter is advanced over the wire towards the coronary cusps. The subsequent steps repeat those that have been described for the femoral approach.
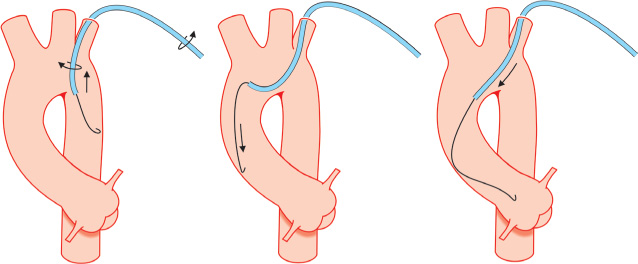
FIGURE 6.5Operators can use the illustrated steps to overcome potential difficulties in engaging the ascending aorta from the left brachial or radial artery approach.
With the right brachial or radial approach, the JL catheter is not routinely used for engagement of the LCA ostium, as other catheters such as Amplatz Left (AL), Schoonmaker-King multipurpose, Jacky (Terumo Medical Corp., Somerset, NJ), or Tiger catheters have higher success rates. In those rare cases when the operator still decides to proceed with a JL catheter, the J-tip guidewire is navigated into the ascending aorta all the way down to the aortic cusp, where the wire is forced to make a loop. The JL catheter is advanced over the guidewire until its tip covers the guidewire tip. Then the wire is removed, the catheter is gently pulled back and clockwise torque is applied in order to cannulate the ostium of the LCA.
Amplatz Coronary Catheter for Femoral, Left Brachial, or Radial Approaches
Amplatz catheters can be used to cannulate the ostia of the left and right coronary arteries, but have a higher chance of causing ostial injury in the hands of inexperienced operators. Although standard coronary angiography can be done with these catheters, they are routinely used in situations where the ostia of the left or right coronary arteries cannot be engaged with Judkins catheters due to unusual take-offs (out of plane, high take-off, separate ostia, and not originating from the appropriate coronary sinus).
LCA CANNULATION WITH AMPLATZ LEFT CATHETER VIA THE FEMORAL APPROACH
The choice of AL catheter size depends on the size of the aortic root, with size 1 corresponding to a small aortic root, size 2 to the regular aortic root, and size 3 to a large one. In order to cannulate the LCA, the operator advances the catheter over the wire under fluoroscopic guidance and positions its tip at the level of the sinotubular junction. Further steps for preparing the catheter are routine and have been described earlier. Once these steps are completed, the catheter (in LAO caudal projection) is advanced into the LCC without rotational manipulation of the tip. The secondary curve of the catheter ends up resting in the noncoronary cusp (NCC), while the primary curve and the tip are in the left cusp. Advancing the catheter with mild, counterclockwise torque forces the catheter to move up towards the LCA ostium (Figure 6.6).
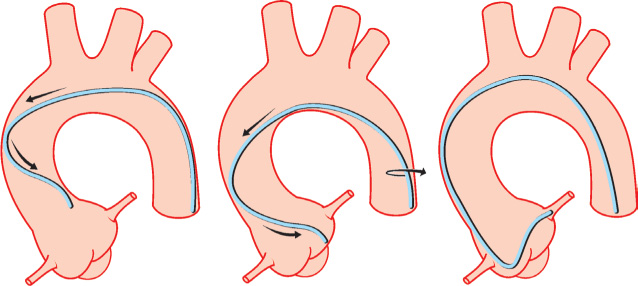
FIGURE 6.6Operators can use the illustrated steps to cannulate the LCA using an AL catheter (see text for details).
Advancing and withdrawing the catheter moves the catheter tip in a vertical plane. It is important to remember that with catheter retraction, its tip has a tendency to damage the coronary ostium, so the operator should be aware of the pressure curve and catheter tip position at all times and, if in doubt, proceed with 1–2 mL of contrast test injection under fluoroscopy. As the tip of the catheter climbs up the wall of the coronary cusp, test injections in LAO and RAO projections can help the operator to establish the position of the left coronary ostium and its relation to the tip of the catheter. Based on this view, the operator makes a decision on the need to further advance or slightly rotate the catheter. When the tip of the catheter enters the LCA ostium, slight withdrawal of its body prevents displacement from the ostium. If the tip points up, the catheter should be pulled slightly back, and if the tip points down, the catheter is slightly advanced. The operator should avoid aggressively retracting or advancing the catheter tip into the LM trunk in order to avoid injury. Once the catheter tip is placed coaxially with the LM trunk and all appropriate angiographic images are obtained, the catheter is gently advanced, then clocked or counterclocked to disengage from the ostium in order to avoid dissection of the LM artery (Figure 6.7).
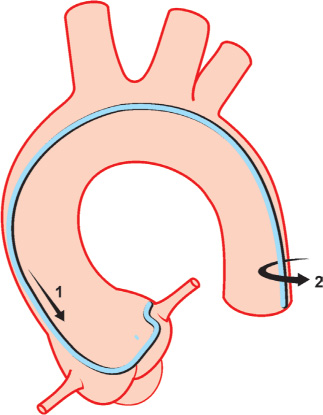
FIGURE 6.7Operators can use the illustrated steps to properly disengage an AL catheter from the LCA ostium (see text for details).
LCA CANNULATION WITH AMPLATZ CATHETER VIA BRACHIAL OR RADIAL APPROACH
When utilizing the left brachial or radial approach, the operator may experience occasional difficulties placing the AL catheter due to the inability to navigate a J-tip guidewire into the ascending aorta. Maneuvers to overcome this problem have been described earlier. The subsequent steps repeat the femoral approach for AL catheter placement.
Selective Cannulation of the Native Right Coronary Artery (RCA)
JUDKINS RIGHT CORONARY CATHETER FOR FEMORAL, LEFT BRACHIAL, AND RADIAL APPROACHES
The cannulation of the ostium of the normally positioned right coronary artery (RCA) with a JR catheter requires manual dexterity. Two approaches will be described. When the ostium of the RCA is approached from above, the clockwise rotation of the catheter drops its tip down into the right coronary cusp (RCC), with frequent cannulation of the ostium of the artery. When the ostium of the RCA is approached from below, gentle pull back after clockwise rotation usually intubates the ostium of the artery. Despite these differences, the general technique for RCA cannulation with the JR catheter is very similar. The operator advances under fluoroscopic guidance the catheter over the J-tip guidewire through the arterial sheath to the aorta. Further steps for preparing the catheter have been described above. The JR catheter is advanced into the ascending aorta towards the RCC under fluoroscopic guidance in LAO 45-degree projection. In the RCC, the tip of the catheter should be facing the left shoulder of the patient. Under fluoroscopic guidance, the catheter is gently withdrawn approximately one intercostal space with simultaneous clockwise torque (Figure 6.8).
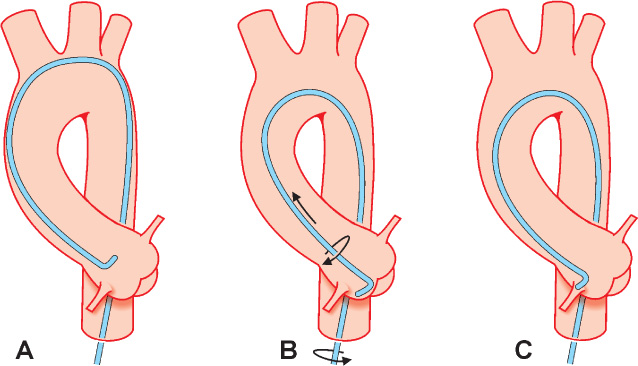
FIGURE 6.8Operators can use the illustrated steps to cannulate the RCA using a JR catheter (see text for details).
This slow, step-by-step, half-turn clockwise rotation should be done by the operator using the fingers of both hands, with the right hand on the catheter hub adaptor and the left hand assisting in turning the catheter near the end of the arterial sheath. After each turn, allow a short interval for transmission of the torque that is applied at the base of the catheter to its tip, just enough to point the catheter tip towards the right side of the patient’s body. To facilitate this process, sometimes minimal in-and-out movement of the catheter is performed. This step-wise rotation allows the operator to avoid over-torqueing the catheter tip. The operator usually observes a small jump of the catheter tip when it cannulates the ostium of the coronary. In other cases, the operator notices a “catch” when the tip of the catheter gets fixed in the ostium of the artery. When RCA ostium cannulation is suspected, the pressure tracing is checked, and a small, half-turn, counterclockwise torque of the catheter is performed in order to neutralize the buildup of tension on the body of the catheter body by clockwise rotation. This movement will prevent the disengagement of the catheter tip from the coronary ostium. If the operator is not sure of the catheter tip position, test injections of 1–2 mL of contrast will assist in locating the ostium of the RCA. Occasionally, a separate origin of the conus branch, which is positioned anteriorly to the ostium of the RCA, complicates the clockwise approach. In such cases, counterclockwise rotation of the catheter with a posterior approach to the RCA ostium avoids cannulation of the conus branch and may help to solve the problem. In some cases, the ostium of the RCA is positioned high and anteriorly, or normally but with superior or inferior orientation and is not engaged easily with a standard JR4 catheter. In such cases, 3D-RCA, IMA, or right coronary bypass (RCB), MP and Amplatz catheters may become handy. When the RCA ostium is cannulated, pressure is checked, and further effort is applied in order to place the tip of the catheter coaxial to the proximal segment of the artery (Figure 6.9).
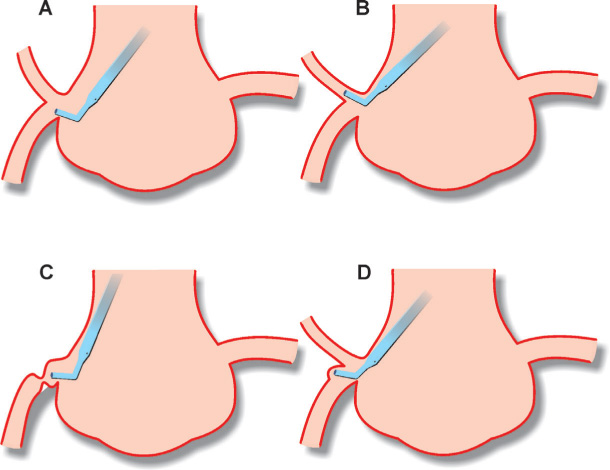
FIGURE 6.9Drawings illustrate the importance of coaxial positioning of the catheter tip into the RCA ostium (see text for details).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree