Congenital Heart Disease
Why are some children born with abnormal hearts? Sometimes we can answer this agonizing question; sometimes we can’t.
Certain infections during early fetal life can produce various types of birth deformities, including abnormalities of the heart structure. German measles is a familiar example. To some extent, these diseases and the abnormalities that go with them are preventable.
Some abnormal genes, like the gene of Down syndrome, carry abnormality of the heart structure encoded right on the DNA that determines everything about us. At our present stage of medical knowledge, there’s no way of preventing these complications.
Many congenital heart abnormalities simply appear for no reason in otherwise healthy individuals.
About 1 out of every 1,000 babies born will have a congenital heart defect. Because of the early death of the more severe cases, about 1 in 3,000 will have an abnormal heart at the end of 1 year of life.
Parents who have one child with congenital heart disease have a slightly increased risk of the same kind of disease in a second child. The word slightly is emphasized here—the difference in risk isn’t very great.
This chapter discusses the major forms of congenital heart disease in their order of occurrence.
Congenital Aortic Stenosis
In the Western world today, most aortic stenosis is congenital; the acquired type associated with rheumatic fever has become rare. The disease starts with an abnormally constructed aortic valve. Instead of the normal three-valve flaps, this valve has only two—hence the term bicuspid aortic valve (Fig. 13-1).
The two-flap valve by itself isn’t a problem, but in some cases the tissue of the valve is thickened and rigid at birth and the aortic opening is very narrow. The usual complications of aortic stenosis will follow: congestive heart failure, dizziness, and fainting. In severe cases, the only treatment is surgery, and the results are good.
The great majority of bicuspid valves don’t present any problem in early life, but in later years 50% of these valves will calcify and narrow, with significant aortic stenosis.
The symptoms are those to be expected when the entire blood supply for the body has to force its way through a narrow slit. Dizziness, fainting, angina pectoris, and congestive heart failure are all common manifestations. The risk of sudden death is very high after symptoms appear, and the only treatment is surgery. Once symptoms have appeared, there is no excuse for delay.
Septal Defects
Remember that there isn’t supposed to be any connection between the two sides of the heart. Sometimes during fetal development, there’s a failure of closure of the septum between the two sides of the heart and the child is born with a gap, or defect, in the septum. The defect—it’s really just a hole—may lie between either the atria or the ventricles. The ventricular type is more common.
Ventricular Septal Defects
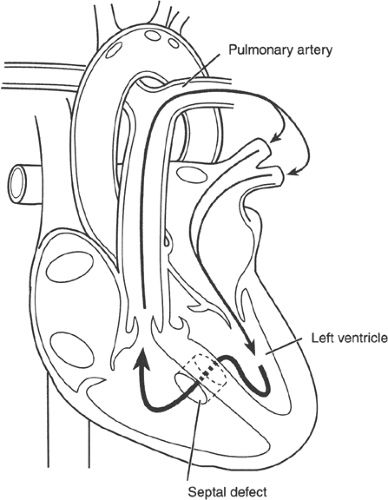
The pressure in the left ventricle is about five times as high as the pressure in the right throughout systole. If there is a hole in the septum between the ventricles, blood will flow from the left ventricle to the right, into the lungs, and back around to the left ventricle (Fig. 13-2).
If the hole is small, this isn’t important. The heart can accommodate a small extra volume of blood going around the circuit and the patient can live a normal life.
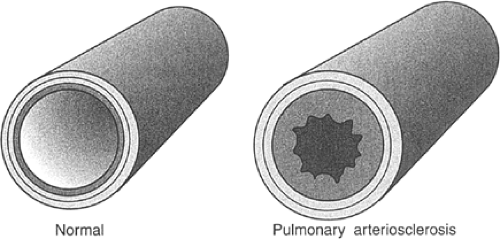
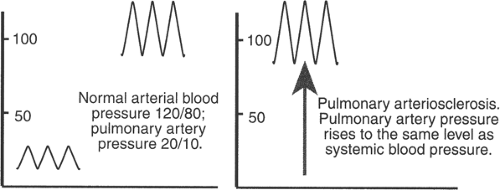
If the hole is large, there is real danger. Now there is a large volume of blood being pumped into the lungs with a rapid, turbulent flow. The blood vessels of the lungs are fragile, not made to stand this kind of pressure and flow. Over the years they harden, with thickening of the coats of the small arteries (Fig. 13-3). This hardening of the pulmonary arteries causes the pressure in the pulmonary vessels to rise. Finally, the pressure in the pulmonary vessels may be as high as the pressure in the aorta.
At this point, the flow of blood will reverse, right to left, because the high pressure in the right ventricle will force some blood through the defect into the left ventricle. The patient will turn cyanotic (blue) because of the appearance in the arteries of unoxygenated blood that didn’t go through the lungs. This is called the
Eisenmenger phenomenon (Fig. 13-4). When this happens, there’s nothing to be done for the disease.
Eisenmenger phenomenon (Fig. 13-4). When this happens, there’s nothing to be done for the disease.
On the other hand, it’s easy to close a ventricular septal defect surgically. If it is closed in time, the reaction in the lungs will not take place and the patient will be able to live a normal life, with no bad effects.
Note: Ventricular septal defects of any size should be closed surgically before this fatal reaction takes place.
Any child with a ventricular septal defect should be studied very carefully to check the size of the defect.
Atrial Septal Defects
There are some interesting differences between atrial septal defects and those in the ventricular septum.
When an atrial septal defect is present, the blood flows through the hole from the left atrium to the right atrium, then to the right ventricle and pulmonary artery. The extra blood never reaches the left ventricle; it flows through the defect from left atrium to right before it gets there. There’s no fluid load on the left side of the heart (Fig. 13-5).
Even though the volume of blood flowing through the defect may be large, it doesn’t affect the small pulmonary arteries the way a ventricular septal defect does. Atrial septal defect is not nearly as dangerous as a ventricular septal defect because the Eisenmenger reaction is very rare with atrial defects. The reason for this difference is probably the low velocity of the blood moving through the atrial shunt and into the lungs, as well as the absence of turbulence in the flow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree