(1)
The Lindner Center for Research and Education The Christ Hospital, The Christ Hospital Physicians Ohio Heart and Vascular Center, Cincinnati, OH, USA
Keywords
RadiationIonizing radiationRadioactivityElectronsAlpha particlesBeta particlesElectromagnetic spectrumGamma raysX raysX ray tubeKiloelectron voltmAmAsMilliamperemAseff Exposure timeEffective milliampereContinuous x raysElectronActivityExposureAbsorbed doseEquivalent doseEffective doseStochastic effectsTissue weighting factorKDose length productCTDICTDIwCTDIvolMilisievertsmSvBecquerelBqMillicuriemCiGrayGyREMRadioactive equivalent in manRadDeterministic effectsLinear No Threshold Dose Response TheoryALARAAs Low as Reasonably AchievableRadiation doseTube voltageProtection I StudyProtection II StudyProtection III StudyProtection IV StudyDose modulationAutomated exposure controlTube voltage reduction ECG dose modulationProspective gatingHigh pitch imagingIterative reconstructionRadiation is defined as energy in transit. Ionizing radiation describes energy in transit that possesses sufficient power to remove electrons from an atom. The term radioactivity refers to the characteristic of a material to emit ionizing radiation. Clinical computed tomography (CT) involves the use of x rays, a form of ionizing radiation. Table 1.1 lists other common types of radiation and their characteristics. Unlike Alpha or Beta radiation, which are radiation particles, x rays are part of the electromagnetic spectrum (Fig. 1.1). Also included in the electromagnetic spectrum are gamma rays which are produced by unstable nuclei and possess slightly more energy (higher frequency) than x rays. Alpha and Beta particles have significantly more energy than either x rays or gamma rays but have very little penetrating ability and thus are not very useful in medical imaging. Alpha particles are shielded by skin or clothing and Beta particles are blocked by glass or plastic. X rays and gamma rays require lead or concrete for shielding. As the energy of a member of the electromagnetic spectrum falls, so does its wave length frequency.
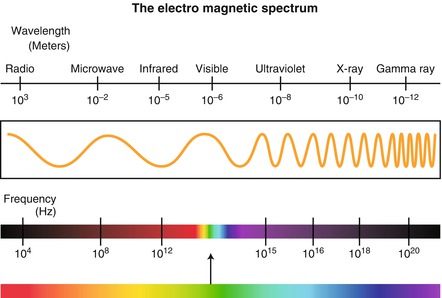
Table 1.1
A table depicting the most common types of radiation and their characteristics
Radiation type | Description | Charge | Shielding material |
|---|---|---|---|
Alpha | Particle | +2 | Skin, clothes |
Beta | Particle | ±1 | Plastic, glass |
Gamma | Electromagnetic wave | 0 | Lead, concrete |
X ray | Electromagnetic wave | 0 | Lead, concrete |
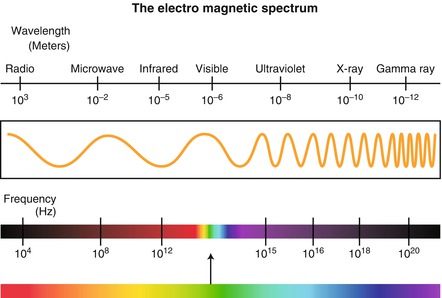
Figure 1.1
A cartoon depicting the electromagnetic spectrum of which x rays are a part
X rays are formed from the electron shells of an atom and are produced in an x ray tube which consists of a negatively charged cathode and a positively rotating anode (Fig. 1.2). The anode rotates to avoid excessive heat production when one location on the anode is bombarded by electrons. This rotating mechanism serves to vary the location on the anode where the electrons interact. The cathode and anode consist of Tungsten. Heating of the cathode causes the electrons within it to separate. Positive charge applied to the anode then forces the separated electrons from the cathode to move toward the anode. The speed with which these electrons travel depends on the charge difference which is applied between the cathode and the anode. The cathode generated electrons strike the anode and interact with its outer electron shells producing characteristic x ray photons (Fig. 1.3), which occur when the incident electron strikes an inner shell with enough energy to displace its electron. An electron from an outer shell moves inward to replace the vacated electron. The remaining energy is emitted as a characteristic x ray photon. Because the charge difference between the anode and the cathode determines the force with which the incident photons bombard the anode, it is this charge difference that defines the energy (kilo-electron volt, KeV) of the x ray photons produced. The number of x ray photons per unit time leaving the x ray tube is known as the photon flux or tube current and is measured in amperage. The unit for tube current in CT is the milliampere (mA). While mA is the term and unit applied to the tube current of a CT scanner, it does not take into account the scan time. Thus, the unit mAs (mili-amperes-second) was created. mAs = mA × gantry rotation time for a pitch of 1. Pitch is discussed in later chapters but simply put, is the term applied to the speed of the CT table movement. However, since a pitch of less than 1 is needed for cardiac CT (to provide image overlap, discussed in a later chapter) another term must be introduced, the effective milliampere-second, mAseff. The term mAseff accounts for a pitch of less than 1. mAs eff = mAs × exposure time, where exposure time = gantry rotation time/pitch. Thus, mAs eff = mAs × gantry rotation time/pitch.
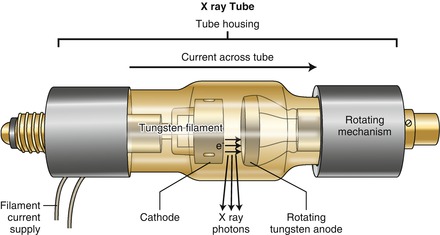
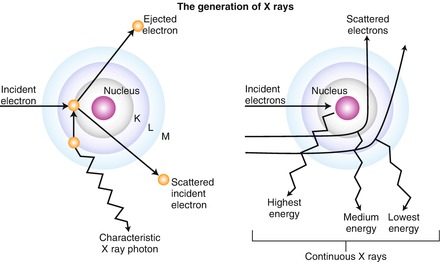
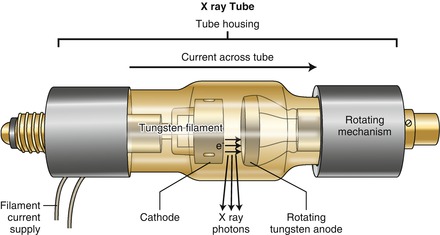
Figure 1.2
A cartoon depicting a basic x ray tube. See text for functional details
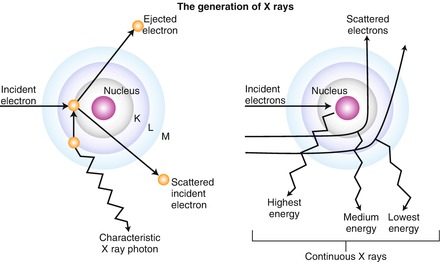
Figure 1.3
A cartoon depicting the mechanism by which characteristic x rays and continuous x rays are generated. See text for details
Continuous x rays are not applicable to medicine. These occur when the incident electron interacts with but does not displace an inner shell electron. The resulting energy difference is emitted as a continuous x ray, the energy of which depends on the type of electron to electron interaction that occurs which is in turn based on the speed with which the incident electron strikes the anode (Fig. 1.3).
Radiation may be quantified in biological terms (relating to the human body) or mechanical terms (relating to the CT scanner). Important biological terms include activity, exposure, absorbed dose, equivalent dose and effective dose. Activity is the number of times per second a radioactive material decays and releases radiation. Exposure is the measure of the ionization produced in air by x rays or gamma rays. Absorbed dose is the amount of radiation energy absorbed into a given mass of tissue. Table 1.2 depicts the units of radiation applied to these biological terms. Equivalent dose is the energy per unit mass multiplied by an adjustment factor for the type or quality of the radiation and represents a dose estimate. Its units are Seiverts (Sv). X rays and gamma rays have a radiation adjustment factor of 1 so that for x rays and gamma rays, absorbed dose and equivalent dose are equal. Alpha particles on the other hand have an adjustment factor of 20.
Table 1.2
A table illustrating various common biological radiation terms and their units
Old unit | SI unit | Conversions | |
|---|---|---|---|
Exposure | Roentgen (R) | Coulomb/Kg (C/Kg) | 1 R = 258 μC/Kg |
Absorbed dose | Rad (rad) | Gray (Gy) | 1 Gy = 100 rad |
Equivalent dose | Rem (rem) | Sievert (Sv) | 1 Sv = 100 rem |
Activity | Curie (Ci) | Becquerel (Bq) | 1 mCi = 37 mBq |
Effective dose is the sum of all weighted equivalent doses in all the organs and tissues of the body and is also measured in Sv. Effective dose compares the cancer risk of a non-uniform exposure of ionizing radiation with the risks caused by a uniform exposure to the whole body. Effective dose is a misnomer since it is not a measurement of dose but rather a concept that reflects stochastic risk (risk of cancer formation) from an exposure to ionizing radiation. The concept of effective dose has several limitations in that it uses a mathematical model for a standard person’s body and is therefore not appropriate for one given individual. It does, however, allow the comparison of biologic effects between diagnostic exams of different types. By comparing effective dose of a particular imaging examination to the average background radiation exposure and to the expected benefits of the imaging test, patients are better able to put the risks associated with medical imaging into perspective. Effective dose = Equivalent Dose x Tissue Weighting Factor. The tissue weighting factor is tissue specific and is itself a fraction such that the effective dose is a fraction of the equivalent dose. Effective dose is calculated by the equation Effective Dose = DLP × k where DLP is the Dose Length Product, which itself is calculated by the equation DLP = CTDIvol × scan length and has units of mSv-cm. DLP integrates the CTDIvol, which is explained below, over the length of the scan. k is a constant specific to the area of the body being scanned (Table 1.3). It reflects the radiation sensitivity of a particular body part. For the chest, for example, k = 0.017 for most scanners. The units of k are mSV/mSv-cm so that the units of effective dose are mSv.
Table 1.3
Table depicting the k value for various body parts
Body part | K |
|---|---|
Head | 0.0023 |
Neck | 0.0056 |
Chest | 0.017 |
Abdomen | 0.015 |
Pelvis | 0.019 |
Important mechanical (scanner specific) radiation terms are Computed Tomography Dose Index (CTDI), Weighted CTDI (CTDIw) and CTDI Volume (CTDIvol). CTDI is the term used for the estimation of the delivered dose for the given specific scan parameters applied to a specific scan such as KeV, mAs, etc. CTDI is measured in a thermolucent dosimeter. CTDIw is the weighted average of the CTDI in the X and Y planes. CTDIw = 2/3 CTDI surface + 1/3 CTDI center. The units for CTDI and CTDIw are Gray (Gy) which for x rays is equivalent to Sv. CTDI and CTDIw do not account for the scan length (Z axis). Thus, CTDIvol was constructed. CTDIvol is the term used for the estimation of the delivered dose accounting for the scan length. CTDIvol = CTDIw/Pitch. As the pitch decreases, the scan length increases so the CTDIvol also increases. That is, the faster the pitch, the lower the radiation dose delivered since a faster pitch shortens the scan time. The units of CTDIvol are also Gy. DLP is also a scanner specific dose estimation term. It is the very best scanner specific dose estimate available.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


