(1)
The Lindner Center for Research and Education The Christ Hospital, The Christ Hospital Physicians Ohio Heart and Vascular Center, Cincinnati, OH, USA
Keywords
ALARAAs Low as Reasonably AchievableCCTA laboraroryIntersocietal Commission for the Accreditation of Computed Tomography LaboratoriesICACTLAmerican College of RadiologyACRGantry rotation timesScanner detector row numberInjection pumpsAbsolute contraindicationsRelative contraindicationsPatient instructionsMetforminContrast allergyRenal functionBreath holdHounsfield UnitsH.U.Tube currentField of viewProspective triggeringScan protocolsECG editingInterpreting a CCTA examinationIsotropic voxelsVolume rendered imagesVRTMaximum intensity projectionsMIPMultiplanar reformatMPRCurved multiplanar reformatcMPRSystematic reading approachImaging artifactsCoronary artery evaluationCoronary stenosis gradingQualitative stenosis gradingQuantitative stenosis gradingBypass graftsCoronary stentMyocardial perfusionCardiac chamber sizeCCTA reportingIntroduction
The development of cardiac computed tomographic angiography (CCTA) as a mainstream cardiac and coronary artery imaging modality mandates the adherence to and application of standards and reliable practices for its performance, interpretation and reporting. The Society of Cardiovascular Computed Tomography (SCCT) has published guidelines on the performance, interpretation and reporting of CCTA, which should be responsibly and routinely applied [1, 2]. In addition, the SCCT has also published a manuscript detailing the standardized medical terminology which should be adhered to [3].
Performing CCTA
The diagnostic quality and usefulness of CCTA is highly dependent on appropriate patient selection and preparation, adherence to appropriate indications for its use and technical factors, which include proper training for the interpreting physician and technical staff, hardware, software and acquisition protocols. Further, the safety of this imaging modality is highly dependent on the responsible and expert understanding and use of radiation and its safety principles. These factors are in constant evolution and development and thus, it is paramount that the responsible CCTA team maintains its professional continuing medical education in this field. The performance of CCTA should employ a minimum standard for use and interpretation.
All CCTA examinations should be overseen and interpreted by adequately trained physicians and ancillary staff. Knowledge of radiation principles and safety is essential and the ALARA (As Low as Reasonably Achievable) is also important. These principles should always be applied. Additionally, the interpreting physician should possess appropriate knowledge concerning the coronary arteries, cardiac and pericardium, great vessels and extra cardiac structures. The recommended necessary training has been published by the appropriate governing bodies [4–6]. It is desirable that a CCTA imaging center have a director with advanced expertise in CCTA (i.e. diplomat of the Certification Board of Cardiovascular CT (CBCCT) or American College of Radiology (ACR) Certificate of Proficiency in Cardiac CT). All CCTA technical staff should also be appropriately trained and familiar with the ALARA principles.
The CCTA laboratory should be accredited by the appropriate body (Intersocietal Commission for the Accreditation of Computed Tomography Laboratories [ICACTL], or the American College of Radiology [ACR]). Scanners with gantry rotation times of ≤350 milliseconds (ms) are recommended although <400 ms is acceptable. Currently, scanners with at least 64 detector rows are recommended, although the guidelines state a requirement of at least 16 rows. The detector element width should be ≤0.75 millimeters (mm). Dual headed injection pumps that allow biphasic or triphasic injections are optimal with injection rate capabilities of 4–7 milliliters/second (ml/s). A CT data storage system that permits storage and retrieval of the entire diagnostic image set is required.
It is highly recommended that radiation dose estimates in dose length product (DLP) are recorded and stored for retrieval and periodic review. Conversion to an effective dose in milliSeverts (mSv) is also permissible.
Patient selection and clinical indications should adhere to the published appropriateness criteria recommendations which are outlined elsewhere in this text [7]. Patient education and preparation should be performed by qualified staff members, the details of which are discussed earlier. Absolute contraindications (factors that affect patient safety) include a known history of severe anaphylactic iodinated contrast reactions, pregnancy, clinical instability, and moderate to severe renal insufficiency. Relative contraindications (factors where the diagnostic quality of the scan may not be adequate to justify its use) include morbidly obese patients,, inability to cooperate with scan instructions or with the necessary breath hold, contraindications to B-blockade in the presence of an elevated heart rate or to nitroglycerin, and heart rate variability or arrhythmia.
Patients should be instructed not to have food for 3 or 4 h before the scan. They may drink water or clear fluids up to the time of the examination to avoid dehydration and secondary sinus tachycardia. Caffeine should be avoided for 12 h prior. All regular medications should be taken the morning of the exam. Pre-medication for contrast allergies, if applicable, should be taken. Patients should not take metformin for 48 h prior to the scan. Metformin is not nephrotoxic but it is exclusively cleared by the kidneys. If renal failure results from contrast administration, toxic levels of metformin may accumulate, which can result in lactic acidosis. While there is no evidence that withholding metformin before the administration of iodinated contrast is protective, this approach is generally employed. Metformin should definitely be withheld for 48 h after the scan. Since sublingual nitroglycerin is given before a CCTA, Viagra, Cialis or Levitra should be avoided for 48 h before the scan.
Intravenous access must be obtained according to established protocols. While a 20-guage intravenous catheter may be adequate in most, in larger patients in whom rapid infusion rates are needed, an 18-guage catheter is required. The right antecubital vein is most optimal, especially in patients who have a history of bypass grafting with a left internal mammary artery (LIMA) in order to avoid contrast contamination of the origin of the LIMA from the venous injection.
Pretest renal function screening is required. Calculation of glomerular filtration rate (GFR) is preferred over serum creatinine estimates of renal function. The incidence of contrast induced nephropathy (CIN) increases in patients with subnormal GFR and in those with ejection fraction ≤40 % and or diabetes mellitus as well as in the elderly. In addition, CIN increases in those that are dehydrated.
A slow, regular heart rate is required for optimal scanning. Image quality is generally optimized with heart rates ≤60 beats per minute. Oral b-blockade prior to the scan as well as intravenous b-blockade just before the scan is generally employed if necessary. Metoprolol is the standard. Care in using B-blockers should be exercised in those with congestive heart failure and or obstructive lung disease. If not contraindicated, sublingual nitrates are required to dilate the distal coronary arteries for more optimal CCTA visualization. Sublingual nitroglycerin is generally given just before the examination.
To minimize cardiac and chest wall motion, breath holding during the exam is essential. Adequate breath hold instructions are essential and breath hold training may be performed before the scan. Patient positioning on the gantry and electrocardiogram (ECG) lead placement standards are also important. The patient should be positioned so that the heart lies in the focal point of the x rays (center of the gantry). ECG leads should not overly the heart so as to avoid windmill artifact that may result. Patients should be imaged in the supine position with both arms raised above the head. Proper, reliable ECG tracings should be confirmed before the procedure.
Optimal CCTA images require high contrast to noise ratios and optimal intra-arterial opacification with contrast. At least 250 Hounsfield units (HU) within the coronary arteries is necessary but >350 HU is optimal. High iodinated contrast agents are preferred. Typical contrast volumes range from 40 to 120 ml depending on the patient and the indication or question being asked. To assure accurate contrast timing of the scan, test bolus or bolus tracking methods should be employed. The CT laboratory must be equipped and staffed to handle adverse contrast related patient reactions.
Every effort should be made to minimize radiation exposure, while obtaining diagnostic quality images. Tube voltages between 80 and 120 kV are employed using principles discussed earlier in this work. Tube current may also be modified manually or automatically based on protocols discussed in a previous chapter. Automatic exposure control and ECG-based current modulation should be employed. The scanned field of view should be minimized to include only the necessary cardiac and extra cardiac anatomy. Prospective triggering should be employed whenever possible. Appropriate radiation shielding should be utilized when able. Slice thickness, slice overlap, pitch and collimation should be optimized when possible. These practices serve to achieve the minimum necessary radiation exposure. Radiation exposure should be monitored and recorded and periodically reviewed.
Scan protocols should be individualized to the patient and for the question being asked. The first step in a CCTA examination is usually an anterior-posterior scout topogram that allows the technicians to accurately prescribe the scanned field of view (sFOV). The cranial limit of the sFOV depends on the clinical question. For examination of native coronary arteries only, the upper limit of the sFOV will be just above the carina. However, if bypass grafts are being imaged, the upper limit of the sFOV must include the take of the bypass grafts. If a LIMA graft is present, the sFOV extends to the lung apices to include the left subclavian artery and the origin of the LIMA. If only aortic venous grafts are present, the sFOV must include the middle of the ascending aorta. The caudal limit of the sFOV should be slightly below the diaphragm to account for cardiac motion so as not to eliminate the caudal portion of the heart, which may move during the scan due to diaphragmatic drift during the breath hold.
The next step in the CCTA protocol is usually the non-contrasted scan for calcium scoring. Methods for this step have been previously discussed. Whether or not to continue with the contrasted scan based on calcium scoring limits is a controversial topic. It is clear that the amount and location of coronary calcifications may complicate accurate CCTA coronary interpretation. However, it is our experience that the degree and extent of coronary calcification does not consistently preclude accurate and useful coronary artery interpretation. Thus, we do not set an upper calcium score limit for which the contrast scan is cancelled.
Next, the contrasted CCTA examination is performed. Scan settings are individualized to the patient characteristics. The immediate data formed from a CCTA examination is referred to as the DICOM data set or raw data set. These data are not actually viewable. To create interpretable images, the raw data are converted to digital images in which each pixel on the computer screen matrix is assigned a CT number (discussed earlier) and thus an HU value. This reconstruction process is performed by filtered back projection or by iterative reconstruction (discussed in an earlier chapter). While these reconstructions take place with little technologist input, an understanding of these techniques is required. Once the data are reconstructed, the technologist must perform the necessary, appropriate applications such as applying the appropriate filter or selecting the proper phases. Interpretation of the data in multiple cardiac phases is often necessary to differentiate artifact from true coronary lesions. Sharp kernals are often necessary to evaluate stents and highly calcified lesions. ECG editing (discussed previously) should be employed when necessary.
Interpreting a CCTA Examination
The interpretation of a CCTA examination should adhere to the Society of Cardiothoracic Computed Tomography (SCCT) guidelines [2]. Proper, consistently applied interpretation techniques are essential to a successful CCTA program and to foster accurate, clinically useful CCTA examinations. While the following text represents one interpretation style (may vary depending on the reader), guideline mandates and recommendations are discussed.
CCTA studies should be acquired as isotropic (same size in all planes) three-dimensional, ECG-gated data sets that are ≤1 mm in slice thickness [2], which are then reconstructed and displayed on dedicated computer workstations with high powered specialized software that allow appropriate data manipulation and review. Since the coronary and cardiac anatomy are complex and artifacts are frequent and since abnormalities may be subtle, readers review the images using workstations capable of both two- and three-dimensional displays in all of the standard reconstruction formats (volume rendered images, maximum intensity projections, multiplanar reformats, curved multiplanar reformats and curved maximum intensity projections), all of which may be required at one point or another. Additionally, these workstations must allow free manipulation of the data in any conceivable imaging plane. Skilled interpretation requires the reader to be familiar with common artifacts and the acquisition and reconstruction process. It is important to develop a systematic reading and reporting style that avoids omissions. What follows is one such systematic reading approach common in our laboratory.
An initial non-contrasted, so called calcium scoring scan, is performed routinely in our center so long as the patient has not been previously revascularized. In some centers, the calcium scoring scan is used specifically for risk stratification in asymptomatic individuals. When available, we first assess the non-contrasted study. The interpretation of the non-contrasted study requires an independent evaluation and interpretation, which must include the entire scanned field of view, including the valves, pericardium and aorta [2]. An Agatston score and less commonly a volumetric assessment or mass score is performed (see Chap. 6). Calcium reporting may vary depending on the reader’s preference, but should at least include a total Agatson calcium score as well as the age and gender specific percentile based on published nomograms [2]. Additionally, calcium in other portions of the field of view need be described including but not necessarily limited to the aortic valve, mitral annulus and aorta since these findings may have diagnostic and prognostic significance [2]. We also report specific vessel scores as well. Using the MESA vascular age calculator [8], a vascular age may be reported. Figure 7.1 illustrates the required and optional interpretation points for the non-contrasted scan.
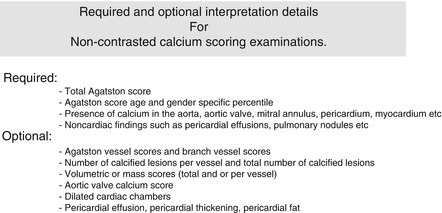
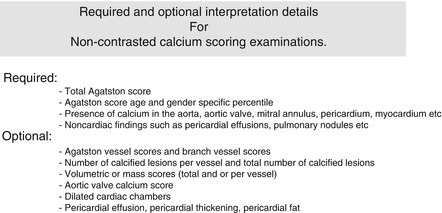
Figure 7.1
A listing of the recommended and optional interpretation points for the non-contrasted calcium scoring scan
Imaging artifacts occur with great enough frequency that mandates evaluation for them and the overall scan quality before proceeding with the CCTA read. We have found that the best way to do this is to review the images in the sagittal and coronal planes in a mutliplanar reformat (MPR). The sagittal images are evaluated for chest wall and sternal motion artifact that may be attributed to breathing during the scan and for cardiac misregistration otherwise known as misalignment artifacts attributable to cardiac motion or arrhythmia. A priori knowledge of these artifacts and whether they interfere with a particular coronary artery segment will help in coronary artery interpretation and in indicating the overall diagnostic reliability of the scan. In the coronal plane, contrast timing and intensity are evaluated and any cardiac misalignment artifacts are also noted. The coronal MPR is adjusted to simultaneously illustrate the left ventricle, left ventricular outflow tract and the aorta to assure adequate contrast intensity and timing. Contrast intensity throughout should measure at least 250 H.U., but more optimally should be above 350 H.U. to assure adequate coronary artery opacification. See Fig. 7.2. The purpose of this exercise is to evaluate for potential low vessel contrast intensity, which may impair evaluation of the coronary arteries.
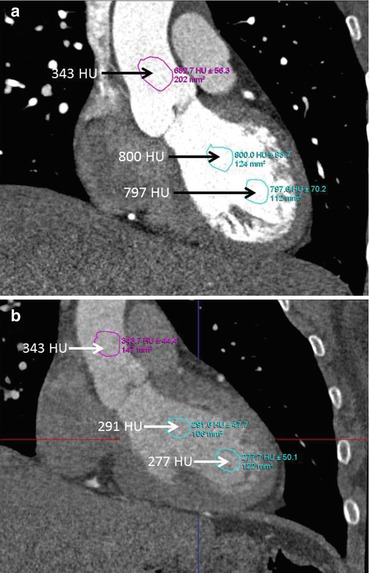
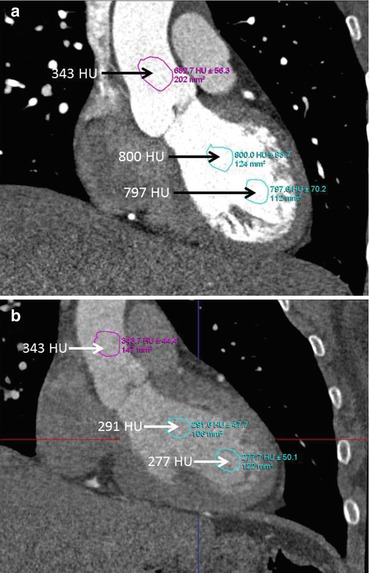
Figure 7.2
Panel (a) demonstrates a coronal multiplanar reformat in a plane that illustrates the left ventricle, left ventricular outflow tract and the aorta. This view is ideal for evaluating contrast timing. Here one sees regions of interest drawn in the apex of the heart, the mid ventricle and in the aorta. The Hounsfield unit (HU) measurement is well above 350 in each region, indicating adequate contrast timing and intensity. Panel (b) demonstrates a scan where contrast timing is late (less intense in the cardiac apex than in the aorta) and slightly inadequate (less than 350 HU in the left ventricle) which might lead to underopacification of the coronary arteries and decreased diagnostic accuracy
Following the quality evaluation, an assessment of the CCTA images is recommended. The critical components of coronary artery evaluation include a systematic evaluation of all coronary segments in multiple planes including the axial transverse plane, an understanding and awareness of important clinically relevant artifacts, a review of the lesion morphology and characterization and an assessment of lesion severity. We recommend first analyzing the axial images to begin the analysis of the coronary tree and the cardiovascular structures. The axial data set is the truest data set since it is the least processed and will give a good overview of the coronary arteries and pertinent cardiovascular structures. In addition, in the axial view, an appropriate initial phase for interpretation is selected by looking at the right coronary artery and choosing a phase where motion artifact is absent (Fig. 7.3). Furthermore, the axial data set at the level of the take off of the coronary arteries is a good place to exclude coronary anomalies by demonstrating normal locations for the origins of the right coronary and left main coronary (Fig. 7.4). Finally, the axial images are reviewed from cranial to caudal by scrolling through them to quickly assess the cardiac and extracardiac anatomy to identify abnormalities which will be reviewed in more detail later.
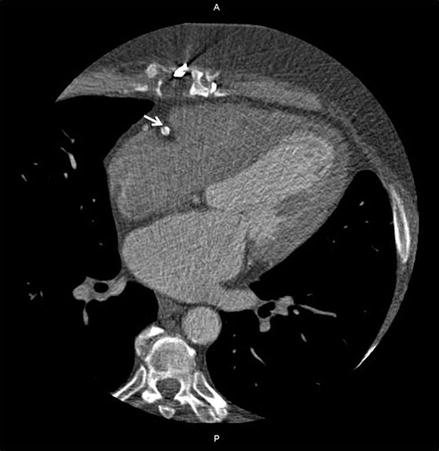
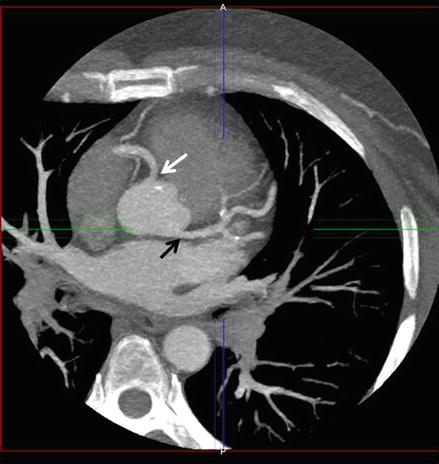




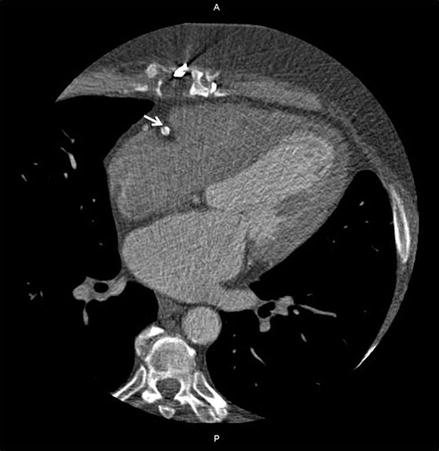
Figure 7.3
An axial multiplanar reformat demonstrating a short axis rendering of the right coronary artery (RCA, white arrow) coursing through the atrio-ventricular groove, the location of a high degree of RCA movement. Here, the RCA has sharp borders and demonstrates no motion artifact, making this phase an excellent starting phase for interpretation
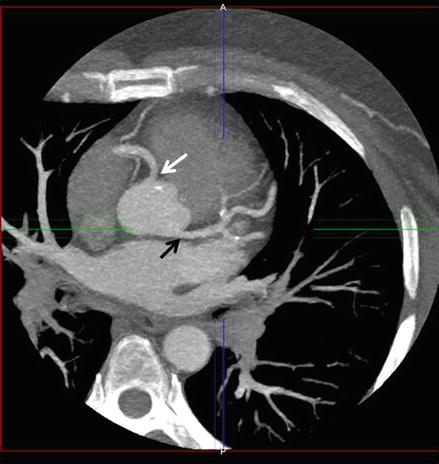
Figure 7.4
An axial thick maximum intensity projection demonstrating the normal origin of the right coronary artery from the right sinus of Valsalva (white arrow) and the left main coronary artery from the left sinus of Valsalva (black arrow), thus excluding a coronary anomaly. A thick MIP is shown here to demonstrate both arterial origins simultaneously. The arteries do not normally originate in the same axial plane
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


