Coronary computed tomography angiography (CCTA) appears comparable to standard care, including exercise stress testing (EST), in diagnosing acute coronary syndrome in emergency department (ED) patients with chest pain but may increase downstream testing. The objective of this study was to investigate rates of post-CCTA versus post-EST testing for (1) invasive angiography and (2) all combined cardiac testing. This was a retrospective cohort study performed at 2 urban Canadian EDs involving patients aged up to 65 years with chest pain but no objective ACS findings that were evaluated with CCTA or EST at the physician’s discretion. The primary outcome was the proportion of patients who had 30-day invasive angiography in each group; secondary outcomes included all subsequent 30-day cardiac testing, including nuclear medicine scanning. From July 1, 2012, to June 30, 2014, we collected 1,700 patients: 521 CCTA and 1,179 EST. Demographics and risk factors were similar in both cohorts. In the following 30 days, 30 CCTA (5.8%) and 297 EST (25.2%) patients underwent any type of additional cardiac testing (difference 19.4%, 95% CI 16.0 to 22.6), whereas 12 CCTA (2.3%) and 20 EST patients (1.7%) underwent angiography (difference 0.6%, 95% CI −0.8% to 2.6%). No patients in either group died or had a myocardial infarction within 30 days. For ED patients with chest pain who underwent brief observation, CCTA and EST had similar 30-day angiography rates, but CCTA patients underwent significantly less overall cardiac investigations.
Approximately 8 million patients visit a United States emergency department (ED) annually with chest pain, and 10% to 15% will have an acute coronary syndrome (ACS) diagnosis. However, most patients—who will not have ACS—undergo observation, sequential investigations, and possibly hospitalization. Several randomized trials have demonstrated that cardiac computed tomography angiography (CCTA) in patients with chest pain with no objective evidence of ACS (such as electrocardiogram changes or cardiac biomarker elevations) can reduce the ED length of stay (LOS) by approximately 6 hours, compared with “standard care.” However, ED patients with chest pain who undergo CCTA appear to have higher rates of subsequent invasive cardiac angiography. The objective of this study was to investigate rates of post-CCTA versus post–exercise stress testing (EST) for (1) invasive angiography and (2) all combined cardiac testing. We hypothesized that CCTA would not be associated with increased downstream investigations.
Methods
This was an observational study of consecutive patients with chest pain from 2 university-affiliated EDs who received either CCTA or EST as part of a protocol to rule out ACS. St. Paul’s Hospital is a provincial cardiac referral site with access to 24-hour catheterization and cardiac surgery, and Mount St. Joseph’s hospital is an affiliated community center. This was a substudy of a prospective investigation to ascertain the safety of outpatient CCTA in ED patients with chest pain. An EST group, presenting during the same time frame as the collected CCTA group, was retrospectively identified as a comparator. The Providence Health Care and University of British Columbia research ethics boards approved the study.
Starting July 1, 2012, patients aged from 18 to 65 years with a primary complaint of nontraumatic chest pain were eligible. As previously described, patients at high risk of ACS (including those with elevated biomarkers or ischemic changes on electrocardiogram [EKG]) were referred to the inpatient cardiology service. Patients deemed to be not at risk of ACS ( Figure 1 ) were discharged home with no cardiac-specific follow-up.
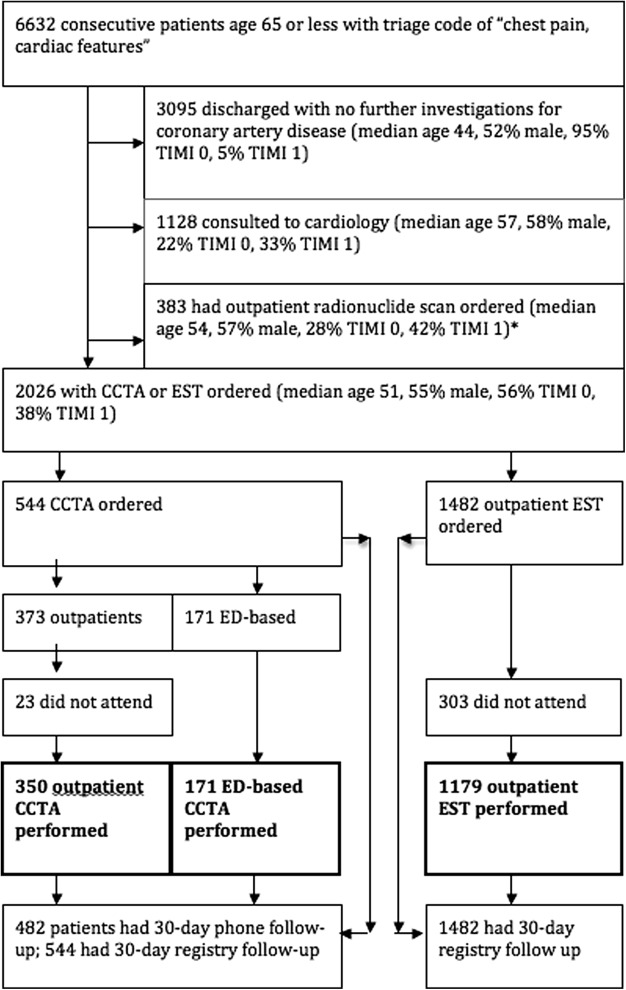
Patients at low-to-moderate risk were discharged and referred for outpatient follow-up testing, at the discretion of the individual physician, within 72 hours: CCTA (for patients with chest pain arriving from 4 a.m. to 2 p.m. , physicians had the option of completing the CCTA before discharge; for all other patients, CCTA was completed as an outpatient), EST, or radionuclide scanning (MIBI). MIBI was typically reserved for older patients, those with previous ACS, those with abnormal baseline EKGs, or those who could not complete the EST protocol, ensuring these patients were systematically different from those chosen for EST and CCTA evaluation. Further CCTA inclusion criteria included sinus rhythm, an estimated glomerular filtration rate >45 ml/min/1.73 m 2 , no previous allergy to contrast agents, and no history of acute reactive airway disease.
The CCTA protocol and follow-up have been previously reported. Briefly, on CCTA completion, attending cardiac radiologists interpreted the images and discussed results with patients. Radiologists discharged patients with <25% stenosis home, referred patients with 25% to 69% stenosis to an outpatient cardiology clinic, and referred those with ≥70% stenosis (or serious noncardiac findings such as pulmonary embolus or malignancy) to the ED for further management. The outpatient EST (based on the symptom-limited Bruce protocol) was supervised by a cardiologist who immediately interpreted and discussed results with patients. Those with low-risk ESTs were discharged home, patients with indeterminate tests were referred for the same-day MIBI, and those with high-risk ESTs (new chest pain or dyspnea, or ST-T segment changes) mandated referral to the ED for cardiology consultation.
The primary outcome was the number of invasive angiograms in the EST and CCTA groups in the 30 days after the index ED visit. The secondary outcome was the total combined number of additional cardiac investigations (after the initial CCTA and EST) in the following 30 days, including subsequent EST, CCTA, and MIBI testing. Additional outcomes included (1) predefined major adverse cardiac event (including ACS, percutaneous coronary intervention, coronary bypass grafting, chest compressions, or death) before their outpatient investigations, and at 30 days, and ( ) ED LOS. Safety end points included (1) median and mean radiation exposure, measured in milliSieverts (mSv) and (2) the number of contrast allergies requiring treatment.
All patients who had testing were identified through the ED database and had a chart review performed according to accepted standards. Risk factors such as hypertension, diabetes mellitus, and hyperlipidemia were defined as previous diagnoses of these diseases or receiving appropriate medications, whereas family history of coronary artery disease was defined as having a first-degree relative (women aged <65 years, men <55 years) with the disease. The Thrombolysis in Myocardial Infarction (TIMI) was obtained for each patient. Two staff emergency physicians and 4 medical students, all whom were blinded to the primary objective, independently collected data on standardized Microsoft Excel 2011 (Microsoft Corporation, Redmond, Washington) spreadsheets. Missing and conflicting data were resolved at regular meetings by further chart review and consensus. To ascertain reliability, a random 10% of charts were independently reevaluated by a second blinded reviewer, and κ values were obtained for all variables.
Thirty-day outcomes were ascertained by linking individual patient data with (1) records from all other regional hospitals which were reviewed to identify any possible ACS-related visits; (2) the British Columbia Cardiac Services Registry, which provides a database of all patients who undergo any cardiac procedure, including percutaneous coronary intervention or coronary bypass grafting; and (3) the British Columbia Vital Statistics registry, which was cross-referenced to identify patients who died.
Continuous variables were summarized with descriptive statistics, whereas discrete variables were summarized as proportions (SPSS Version 16.0.1; SPSS Inc., Chicago, Illinois). Confidence intervals were calculated using the adjusted Wald method.
Results
Over a 2-year period at the 2 hospitals, 6,632 patients aged ≤65 years had a triage code of “chest pain, cardiac features”, and 1,700 were included ( Figure 1 ). The provincial registries followed up all study patients at 30 days.
Interrater reliability data for all 1,700 patients can be seen in Appendix 1 . Table 1 summarizes baseline characteristics of study patients. The age, gender distribution, proportion of patient arriving by ambulance, initial vital signs, quality of chest pain, cardiovascular risk factors, and TIMI risk scores were similar in both groups.
| Characteristic | CCTA | EST | Risk Difference (95% CI) ∗ |
|---|---|---|---|
| n = 521 | n = 1179 † | Not applicable | |
| Demographics | |||
| Age (years), median (IQR) | 51 (44 to 59) | 51 (44 to 58) | 0 (−2 to 2) |
| Male | 322 (61.8%) | 655 (55.6%) | 6.2% (1.1 to 11.3) |
| EMS arrival | 94 (18.0%) | 228 (19.3%) | −1.3% (−5.3 to 3.0) |
| Initial vitals on index ED visit, median (IQR) | |||
| Heart rate (beats / min) | 76 (64 to 87) | 78 (65 to 88) | 2% (-8 to 10) |
| Systolic blood pressure (mmHg) | 141 (123 to 162) | 140 (122 to 159) | -1% (-11 to 11) |
| Diastolic blood pressure (mm Hg) | 81 (70 to 94) | 81 (71 to 93) | 0 (-5 to 5) |
| Respiratory rate (breaths / min) | 18 (16 to 20) | 18 (16 to 20) | 0 (-2 to 2) |
| Oxygen saturation | 99 (98 to 99) | 98 (97 to 99) | -1% (-2 to 0) |
| Temperature (degrees C) | 36.7 (36.5 to 36.9) | 36.7 (36.5 to 36.9) | 0 (-0.1 to 0.1) |
| Cardiac risk factors | |||
| Hypertension ‡ | 186 (35.7%) | 378 (32.9%) | 2.8% (-2.2 to 7.8) |
| Diabetes mellitus ‡ | 53 (10.2%) | 110 (9.6%) | 0.6% (-2.4 to 4.0) |
| Hypercholesterolemia ‡ | 110 (21.1%) | 231 (20.2%) | 0.9% (-3.2 to 5.4) |
| Family history coronary artery disease ‡ | 93 (17.9%) | 150 (21.0%) | -3.1% (-7.6 to 1.5) |
| Current smoker ‡ | 154 (29.6%) | 315 (28.7%) | 0.9% (-3.9 to 5.8) |
| Number of risk factors | |||
| 0 | 257 (49.3%) | 595 (49.7%) | -0.4% (-5.6 to 4.9) |
| 1 | 138 (26.5%) | 301 (25.2%) | 1.3% (-3.2 to 6.0) |
| 2 | 64 (12.3%) | 182 (15.2%) | -2.9% (-6.3 to 0.8) |
| 3 | 29 (5.6%) | 90 (7.5%) | -2.0% (-4.3 to 0.9) |
| ≥ 4 | 9 (1.7%) | 11 (0.9%) | 0.8% (-0.4 to 2.5) |
| Chest pain characteristics | |||
| Chest pain area | |||
| Central | 328 (63.0%) | 682 (64.6%) | -1.7% (-6.9 to 3.4) |
| Left | 166 (31.9%) | 314 (29.8%) | 2.1% (-2.8 to 7.1) |
| Right | 17 (3.3%) | 42 (4.0%) | -0.7% (-2.6 to 1.6) |
| Epigastric | 6 (1.1%) | 19 (1.8%) | -0.7% (-1.9 to 1.0) |
| Other | 4 (0.7%) | 0 (0.0%) | 0.7% (-0.1 to 2.1) |
| Chest pain quality | |||
| Pressure or tightness | 347 (66.6%) | 696 (69.5%) | -3.5% (-8.0 to 2.1) |
| Sharp or stabbing | 100 (19.2%) | 218 (21.8%) | -2.6% (-6.8 to 1.9) |
| Dull ache | 64 (12.2%) | 73 (7.3%) | 5.0% (1.8 to 8.5) |
| Burning or indigestion | 8 (1.5%) | 14 (1.4%) | 0.1% (-1.1 to 1.8) |
| Other | 2 (0.4%) | 0 (0.0%) | 0.4% (-0.2 to 1.5) |
| Associated symptoms | |||
| Dyspnea | 49 (9.4%) | 80 (6.8%) | 2.6% (-0.2 to 5.8) |
| Weakness | 34 (6.5%) | 71 (6.0%) | 0.5% (-2.0 to 3.4) |
| Diaphoresis | 11 (2.1%) | 27 (1.8%) | 0.3% (-1.1 to 2.2) |
| Presyncope or syncope | 14 (2.7%) | 19 (1.6%) | 1.1% (-0.4 to 3.1) |
| Nausea or vomiting | 47 (9.0%) | 68 (5.8%) | 3.3% (0.5 to 6.4) |
| Palpitations | 37 (7.1%) | 50 (4.2%) | 2.9% (0.4 to 5.7) |
| TIMI score | |||
| 0 | 296 (56.8%) | 709 (60.1%) | -3.3% (-8.5 to 1.8) |
| 1 | 212 (40.7%) | 426 (36.1%) | 4.5% (-0.5 to 9.7) |
| 2 | 13 (2.5%) | 24 (2.0%) | 0.5% (-1.1 to 2.4) |
∗ Difference is CCTA minus EST. Differences in proportion use Wilson’s continuity correction.
† There are missing values for the EST group (see appendix 1 ) and the denominator is not always 1179.
‡ As indicated by the patient or on previous medical documentation.
Table 2 describes clinical outcomes of both groups. Of the 521 patients who underwent CCTA, 12 (2.3%) had an angiogram; of the 1,179 patients who underwent an EST, 20 (1.7%) had an angiogram (risk difference of 0.6%, 95% CI −0.8% to 2.5%; risk ratio 1.36, 95% CI 0.78 to 2.75, p = 0.51). A subsequent cardiac investigation took place in 297 of 1,179 EST patients and 30 of 521 CCTA patients (risk difference 19.4%, 95% CI 16.0% to 22.6%; risk ratio 0.23, 95% CI 0.15 to 0.33, p <0.0001). The proportion of patients in the CCTA group who had a major adverse cardiac event was 1.3%, in comparison to 0.4% in the EST group (risk difference 0.9%, 95% CI −0.06 to 2.5; risk ratio 3.17, 95% CI 1.00 to 9.93, p = 0.05).
| Characteristic | CCTA (n = 521) | EST (n = 1179) | Difference (95% CI) ∗ |
|---|---|---|---|
| CCTA results | Not applicable | Not applicable | |
| Normal | 298 (55.5%) | ||
| Less than 25% stenosis | 124 (23.8%) | ||
| 25 – 49% stenosis | 65 (12.5%) | ||
| 50 – 69% stenosis | 27 (5.2%) | ||
| 70% or greater stenosis | 16 (3.1%) | ||
| EST results | Not applicable | Not applicable | |
| Normal | 869 (73.7%) | ||
| Ischemia | 50 (4.2%) | ||
| Non diagnostic | 260 (22.1%) | ||
| Invasive angiography at 30 days | 12 (2.3%) | 20 (1.6%) | 0.6% (-0.8 to 2.5) |
| < 50% maximal stenosis | 5 (1.0%) | 13 (1.1%) | -0.1% (-1.3 to 1.2) |
| > 50% maximal stenosis | 7 (1.3%) | 7 (0.6%) | 1.1% (0.01 to 2.8) |
| Stent placed | 7 (1.3%) | 5 (0.4%) | 0.9% (-0.06 to 2.5) |
| Subsequent cardiac testing within 30 days † | |||
| EST | 20 (3.9)% | Not applicable | Not applicable |
| Normal | 17 (3.3%) | ||
| Ischemia | 0 | ||
| Non diagnostic | 3 (0.6%) | ||
| Radionuclide scan | 10 (1.9%) | 260 (22.1%) | -20.1% (-22.8 to -17.3) |
| Normal | 6 (1.1%) | 192 (16.3%) | -15.1% (-17.5 to -12.6) |
| Reversible ischemia | 2 (0.4%) | 25 (2.1%) | -1.7% (-2.8 to -0.4) |
| Indeterminate | 2 (0.4%) | 43 (3.7%) | -3.3% (-4.6 to -1.8) |
| Stenosis by CCTA (diameter reduction) | Not applicable | 37 (3.1%) | Not applicable |
| Normal | 33 (2.8%) | ||
| 0 to 25% | 3 (0.3%) | ||
| 26 to 49% | 1 (0.1%) | ||
| 50 to 75% | 0 | ||
| ≥ 75% | 0 | ||
| Total subsequent cardiac testing within 30 days † | 30 (5.8%) | 297 (25.2%) | -19.4% (-22.6 to -16.0) |
| 30 day major adverse cardiac events ‡ | |||
| Myocardial infarction | 0 | 0 | 0 (-0.9 to 0.4) |
| Invasive Angiogram | 12 (2.3%) | 20 (1.7%) | 0.6% (-0.8 to 2.5). |
| Percutaneous coronary intervention | 7 (1.3%) | 5 (0.4%) | 0.9% (-0.06 to 2.5) |
| Coronary artery bypass grafting | 0 | 0 | 0 (-0.9 to 0.4) |
| Chest compressions | 0 | 0 | 0 (-0.9 to 0.4) |
| Death | 0 | 0 | 0 (-0.9 to 0.4) |
| Total adverse cardiac events | 7 (1.3%) | 5 (0.4%) | 0.9% (-0.06 to 2.5) |
| Additional outcomes | |||
| Median ED LOS (hours) (IQR) | 7.0 (6.3 to 9.1) | 6.9 (6.2 to 8.8) | 0.1% (-0.9 to 1.0) |
| Median total radiation exposure (IQR) (mSv) | 4.1 (2.9 to 6.7) | 0 (0 to 0.0) § | 4.1% (2.5 to 6.7) |
| Mean total radiation exposure (SD)(mSv) | 5.3 (3.3) | 1.7 (3.8) | 3.6 (3.5) |
| Allergic reactions | 2 (0.4%) | 0 | 0.4% (-0.2 to 1.5) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


