Chapter 23 Comparison of Noninvasive Techniques for Myocardial Perfusion Imaging
INTRODUCTION
A variety of noninvasive techniques permit the assessment of regional myocardial perfusion at rest and during exercise or pharmacologic stress. These techniques include radionuclide imaging employing single-photon emission computed tomography (SPECT) or positron emission tomography (PET) methodologies, contrast echocardiography, computed tomography (CT), and cardiac magnetic resonance (CMR) imaging. All have particular strengths and weaknesses. The reader is directed to earlier chapters in this section of the book for detailed descriptions of the use of these perfusion imaging techniques for detecting functionally significant coronary artery stenoses or abnormal coronary flow reserve due to endothelial and microcirculatory abnormalities. In the paragraphs to follow, the major strengths and weaknesses of these diverse approaches to myocardial perfusion imaging (MPI) will be reviewed, with the understanding that advances in technology for all of these imaging methodologies are continuously being reported. Table 23-1 provides a summary of the strengths and limitations of these four diverse imaging technologies used for the assessment of myocardial perfusion under rest and stress conditions.
Table 23-1 High-Risk SPECT Imaging Variables
| Multiple perfusion defects in > 1 coronary supply region (multivessel coronary artery disease scan pattern) |
| An extensive area of stress-induced hypoperfusion, even if confined to the territory of a single coronary artery (e.g., proximal left anterior descending coronary artery scan pattern) |
| A high ischemic burden reflected by multiple reversible defects |
| Transient ischemic left ventricular cavity dilation |
| Multiple abnormal regional wall-motion or thickening abnormalities, even if not associated with perfusion defects |
| A gated SPECT ejection fraction of < 40% |
| Increased diastolic and end-systolic volumes on quantitative SPECT, increased lung-to-heart ratio of thallium uptake when Tl-201 used for exercise imaging |
SPECT, single-photon emission computed tomography.
RADIONUCLIDE MYOCARDIAL PERFUSION IMAGING (See Chapters 14 to 16)
Stress and rest SPECT myocardial perfusion imaging (MPI) is the most commonly performed imaging technique to detect CAD among patients presenting with chest pain or other symptoms thought to be secondary to ischemia. Table 23-1 shows the main strengths and limitations of radionuclide SPECT MPI relative to other noninvasive techniques for assessing myocardial perfusion. The sensitivity, specificity, and normalcy rate for SPECT MPI for detection of coronary artery disease (CAD) are 86%, 74%, and 89%, respectively.1 The prognostic value of SPECT MPI has been proven with multiple studies reported in the literature (see Chapter 16).2 For patients undergoing exercise stress SPECT imaging who have a normal perfusion scan, the annual death or myocardial infarction rate is 0.7% annually, compared to 5.6% for those with an abnormal scan.2 Similarly, for pharmacologic stress SPECT MPI, the annual hard event rate with a normal scan is 1.2% per year versus 8.3% for patients with an abnormal scan.2,3 The higher event rates with pharmacologic stress MPI are attributed to a higher pretest clinical risk in patients deemed unable to exercise. The greater the stress perfusion abnormalities, the higher the event rates.3 The percentage of the left ventricle rendered ischemic with stress has proven clinically useful in separating patients who might benefit from coronary revascularization versus those who have a good outcome beginning medical therapy.4 The percent left ventricular (LV) ischemia can also be used to serially evaluate response to therapy. The COURAGE nuclear substudy showed that patients who did not experience a 5% or more decrease in ischemic defect size after 1 year of therapy had a substantially higher cardiac event rate over 6 to 7 years of follow-up, compared to patients who showed a greater than 5% reduction in ischemic defect size.5 Interestingly, those patients who had no residual ischemia had no future events during follow-up. Patients with diabetes6 and those with chronic kidney disease7 have higher cardiac event rates with ischemic SPECT studies than patients without diabetes or chronic kidney disease. Such patients also have a higher risk of cardiac death or nonfatal myocardial infarction with normal SPECT scans.2
Specificity of SPECT MPI is enhanced when gated images are obtained, since fixed defects due to attenuation artifacts can be distinguished from myocardial scar on stress and rest images.8 Those due to scar (or severe ischemia) will show abnormal wall motion or abnormal wall thickening, whereas those due to attenuation artifacts, as with breast attenuation in women or inferobasilar wall attenuation in men, will show normal regional function. Gated SPECT MPI can provide functional information that contributes to the diagnostic and prognostic value of the test.9 Functional variables include the left ventricular ejection fraction (LVEF), systolic and diastolic volumes at end-systole and end-diastole, and extent of regional wall-thickening or wall-motion abnormalities. Regional wall-motion or thickening abnormalities seen on SPECT images correlate well with measurements made on echocardiography and MRI. Transient ischemic cavity dilation from stress to rest images can also be identified and in most cases represents stress-induced subendocardial ischemia that resolves with rest. It is a scintigraphic marker of high-risk CAD.10
Attenuation correction algorithms have been introduced for clinical SPECT imaging and have enhanced the accuracy of CAD detection, chiefly by reducing false-positive studies that interpret attenuation artifacts as perfusion abnormalities.11 Standardization of attenuation correction methods from one vendor to another has not yet been achieved. Another variable that may confound the interpretation of SPECT tomograms is high visceral activity, which may interfere with the evaluation of the inferior wall. This is more of an issue with vasodilator stress than with exercise stress. Image quality is also diminished with marked obesity, requiring 2-day stress/rest studies to optimize quality by having more activity injected with the rest image than is possible in same-day, low-dose rest and high-dose stress studies. The SPECT artifacts that interfere with accurate interpretation of MPI images are very well summarized in Chapters 6 and 7.
Stress myocardial perfusion imaging, employing the technetium (Tc)-99m-labeled tracers underestimates the extent of significant coronary artery stenoses.12 Some patients with left main and/or three-vessel CAD may have uniform tracer uptake on vasodilator stress perfusion SPECT images if coronary flow reserve is diffusely reduced in the supply regions of all three major coronary vessels. In the study by Lima et al., only a small percentage of patients with angiographic three-vessel disease had perfusion abnormalities in the distribution of all three affected coronary arteries13; on gated SPECT images, 23% had perfusion and/or regional wall-motion abnormalities in the myocardial supply zones of the three stenotic vessels (defined as =50% stenosis). Even using quantitative analysis of relative differences in regional counts on vasodilator stress SPECT, 12% of the patients in this study with three-vessel CAD had no perfusion or function abnormalities on their SPECT studies. Similarly, Berman et al.14 reported that among 101 patients with left main CAD (=50% stenosis) and no clinical evidence of prior infarction, 40% had low-risk SPECT scans with less than 10% LV ischemia, and 15% had no ischemic defects.
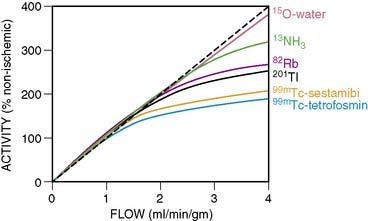
The underestimation of the extent of CAD with SPECT is perhaps more common when 99mTc perfusion agents are used (sestamibi and tetrofosmin) rather than 201Tl.15 The first-pass myocardial extraction fraction is higher with 201Tl (80%) than the other two tracers (55% to 60%), and myocardial uptake is more proportional to flow in the hyperemic flow ranges after vasodilator administration. But in fact all three perfusion agents plateau at high flows (Fig. 23-1). This particularly adversely affects the detection of mild to moderate stenoses.16 Standard SPECT imaging normalizes counts to the region of the myocardium with the highest activity (regional counts). If diffuse multivessel disease is present, that “normal” area may also have subnormal perfusion in response to vasodilator infusion. In this situation, counts in that region may not be higher than in other perfusion zones, since flow reserve is diffusely diminished. When the activity is homogeneous throughout the myocardium in such patients, “balanced ischemia” is often present. If postischemic myocardial stunning or chronic hibernation is present, or if the patient had a prior subendocardial infarction, abnormal regional function can be detected on gated images that would render the interpretation of the stress study as abnormal, despite the absence of focal perfusion abnormalities. Also, transient ischemic dilation of the LV cavity from stress to rest images can at times be observed with normal or minimally abnormal perfusion scans. This finding would hint at the possibility of more extensive underlying CAD.17 A larger LV cavity post stress (compared to rest) is thought to be due to transient stress-induced subendocardial hypoperfusion.
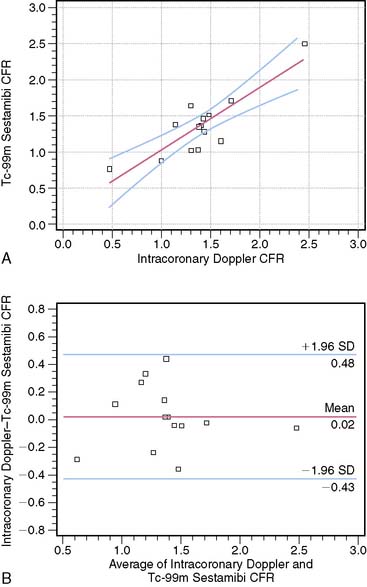
Some attempts have been undertaken to quantitate coronary flow reserve with SPECT perfusion imaging.18 This would address the limitation of standard SPECT in which only relative differences in perfusion from one area of the myocardium to another area are assessed. Estimation of coronary flow reserve (CFR) by SPECT18 involves acquiring anterior planar list-mode images of the heart after intravenous tracer administration. Counts from a right pulmonary artery region of interest are quantified to estimate the arterial input function of the tracer. An estimate of myocardial tissue perfusion is determined by dividing myocardial counts on the SPECT images by the integrated arterial input function. Perfusion values for the stress studies are divided by the corresponding values from the rest studies to obtain myocardial perfusion reserve. Limitations of SPECT that do not allow absolute quantitation of regional myocardial blood flow in mL/min/g are factors such as scatter, attenuation, partial-volume effect, and low resolution. Nevertheless, just being able to evaluate CFR by measuring the ratios of tissue and arterial counts at rest and stress might enhance the detection of multivessel CAD. Figure 23-2 shows the relationship between SPECT-estimated CFR and intracoronary Doppler CFR measurements. Studies continue to be performed to try to achieve absolute quantitation of perfusion with dynamic SPECT imaging.19 Using an experimental canine model, these investigators demonstrated that the kinetic analysis of quantitatively assessed myocardial 201Tl accumulation provided myocardial blood flow measurements that agreed well with flows obtained using radioactive microspheres.
Recent advances have been made in SPECT technology, permitting high-speed imaging using a bank of independently controlled detector columns with large-hole tungsten collimators and multiple cadmium zinc telluride crystal arrays (see Chapter 9).20 Using this high-speed camera, the entire stress/rest 99mTc sestamibi MPI procedure could be completed within 30 minutes. The stress and rest acquisition times were 16 and 12 minutes for conventional SPECT MPI and 4 and 2 minutes for high-speed SPECT. Image quality was high, and myocardial count rates were significantly higher versus conventional SPECT. Diagnostic performance for high-speed SPECT was as good as for conventional SPECT, with summed stress scores and summed reversibility scores correlating extremely well (r = 0.93). Introduction of this new technology will reduce the long procedure time for a full stress/rest study as currently performed with conventional SPECT.
POSITRON EMISSION TOMOGRAPHY (See Chapter 19)
PET MPI is an attractive alternative to SPECT for detecting CAD and determining its extent. PET perfusion tracers used clinically for MPI are rubidium (Rb)-82 and nitrogen (N)-13-ammonia. 82Rb is eluted from a generator and has a short half-life of 78 seconds. It is only used with pharmacologic stress and not exercise, which is a limitation. 13N-ammonia requires a cyclotron for production and has a half-life of 10 minutes. They both show a plateau in myocardial activity with increasing coronary flow, although the flow-uptake relationship is better than that of the 99mTc SPECT perfusion tracers (see Fig. 23-1). In the meta-analysis of clinical studies reported in the literature, the sensitivity and specificity of PET MPI are 89% and 86%, respectively.1 When CT is used for attenuation correction, sensitivity is increased to 93% and 95% for detecting patients with multivessel disease.21 Bateman et al.22 compared SPECT with PET for CAD detection in different groups of patients studied in the same time period. They showed that the sensitivity and specificity were higher for PET (87% versus 82% and 93% versus 73%, respectively), as was the prediction of multivessel disease (71% versus 48%). Some reasons for the improved accuracy of PET over SPECT include higher spatial and contrast resolution and the fact that depth-independent attenuation correction is more easily performed, since it is intrinsic to PET methodology. Since the half-lives of the tracers used for PET MPI are so short, fast sequential evaluations of regional flow can be achieved. This promotes improved throughput of patients in clinical laboratories.
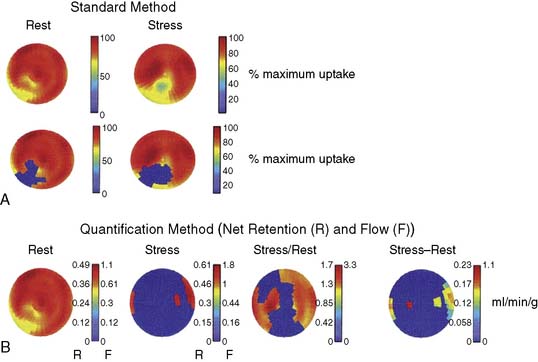
PET has the capability for rapid dynamic imaging of tracer kinetics, permitting absolute quantitation of myocardial blood flow not easily achieved by SPECT technology. This capability is one of the most important advantages of PET over SPECT and other noninvasive technologies for assessing myocardial perfusion. Quantitating regional myocardial blood flow in mL/min/g using tracer kinetic models with rapid dynamic imaging, and obtaining accurate values for CFR rather than just assessing relative differences in perfusion (myocardial counts) from one myocardial region to another, can be achieved. Oxygen-15-labeled water is a positron emitter that is metabolically inert, freely diffusible, and cyclotron-generated. There is virtually complete extraction of this tracer by the myocardium, independent of flow rate and myocardial metabolic state. This makes it the ideal radionuclide for quantitating absolute myocardial blood flow. Quantitation of blood flow with any of the PET tracers includes corrections for the partial volume effect (that causes an underestimation of myocardial tracer concentration), activity spillover from the blood pool to the myocardium, and physical decay. Parkash et al.23 showed that quantitation of 82Rb net retention and estimation of absolute perfusion at rest and with dipyridamole stress defined a greater extent of CAD in patients with three-vessel disease than using the standard approach of assessing relative differences in perfusion (69% of LV sectors versus 44%). The absolute stress-minus-rest perfusion difference in the myocardium is measured in this approach. Figure 23-3 shows an example of the comparison of the standard method for identification of perfusion defects with the quantification method in a patient with stenoses in the left anterior descending (LAD), right, and circumflex coronary arteries. A very good relationship was found between dipyridamole-induced myocardial blood flow in mL/min/g by 82Rb quantitation and stenosis severity in patients with CAD.24 The repeatability of rest and hyperemic myocardial blood flow measurements with 82Rb PET is excellent.25 Myocardial blood flow determinations were highly reproducible in this study of 15 healthy volunteers who underwent two rest and pharmacologic stress studies 60 minutes apart.