The factors that influence decision making in severe aortic stenosis (AS) are unknown. Our aim was to assess, in patients with severe AS, the determinants of management and prognosis in a multicenter registry that enrolled all consecutive adults with severe AS during a 1-month period. One-year follow-up was obtained in all patients and included vital status and aortic valve intervention (aortic valve replacement [AVR] and transcatheter aortic valve implantation [TAVI]). A total of 726 patients were included, mean age was 77.3 ± 10.6 years, and 377 were women (51.8%). The most common management was conservative therapy in 468 (64.5%) followed by AVR in 199 (27.4%) and TAVI in 59 (8.1%). The strongest association with aortic valve intervention was patient management in a tertiary hospital with cardiac surgery (odds ratio 2.7, 95% confidence interval 1.8 to 4.1, p <0.001). The 2 main reasons to choose conservative management were the absence of significant symptoms (136% to 29.1%) and the presence of co-morbidity (128% to 27.4%). During 1-year follow-up, 132 patients died (18.2%). The main causes of death were heart failure (60% to 45.5%) and noncardiac diseases (46% to 34.9%). One-year survival for patients treated conservatively, with TAVI, and with AVR was 76.3%, 94.9%, and 92.5%, respectively, p <0.001. One-year survival of patients treated conservatively in the absence of significant symptoms was 97.1%. In conclusion, most patients with severe AS are treated conservatively. The outcome in asymptomatic patients managed conservatively was acceptable. Management in tertiary hospitals is associated with valve intervention. One-year survival was similar with both interventional strategies.
Aortic stenosis (AS) is the most common valvular heart disease in developed countries and has a poor prognosis when symptoms appear. As about 3/4 of elderly patients with severe AS are symptomatic, the overall burden of disease due to severe symptomatic AS is substantial. Moreover, the impact of severe AS on public health is expected to increase, because of aging Western populations. Aortic valve replacement (AVR) improves prognosis and has been proposed as an option even in patients with severe but asymptomatic AS. Also, transcatheter aortic valve implantation (TAVI) has emerged as an alternative to AVR in symptomatic patients with high surgical risk. However, patients with severe AS are frequently treated conservatively because of several reasons that include geographic disparities, absence of severe symptoms, co-morbidity, overestimation of operative risk by currently used risk scoring systems, and patient preference. Previous data regarding the natural history of severe AS in asymptomatic patients have shown a low overall mortality rate, with an annual rate of sudden death under 1%. In contrast, asymptomatic patients are usually younger and have less risk factors and co-morbidities than those who are symptomatic ; thus, the independent influence of symptoms in this condition is not clear. Moreover, the likelihood of remaining free of symptoms decreases with time. Also, the factors that influence decision making in severe AS are unknown and some data suggest that current guidelines are being overlooked in real-life practice. The objectives of this study are to assess, in patients with severe AS, the determinants of management and prognosis.
Methods
Influencia del Diagnóstico de Estenosis Aórtica Severa (IDEAS)—Influence of the Severe Aortic Stenosis Diagnosis—is a multicenter registry that enrolled all consecutive adults diagnosed with severe AS (mean gradient >40 mm Hg or valve area <1 cm 2 ) in the echocardiographic laboratory of 48 Spanish centers, during January 2014.
The only exclusion was any previous aortic valve intervention, including valvuloplasty, AVR, and TAVI. Informed consent was obtained. Variables registered included clinical and echocardiographic parameters, Charlson co-morbidity index, EuroSCORE II, and hospital characteristics (we considered tertiary centers those with cardiac surgery). The symptoms of dyspnea, angina, or syncope were determined by chart review. One-year follow-up was obtained in all patients and included vital status, aortic valve intervention (AVR or TAVI), and time from echocardiography to intervention. In cases treated conservatively, the main reason for the decision was recorded using the following subgroups: absence of symptoms, co-morbidity, dementia (based on chart review), age, and patient decision. The local site investigators for the study stated if, in their opinion, an intervention should have been performed according to patient characteristics and clinical practice guidelines. This was compared with the actual treatment that the patient received. The study complies with the Declaration of Helsinki and was approved by the Ethics Committee of Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Comparisons between groups were performed using the chi-square or Fisher’s exact test for categorical variables and Student’s t test or ANOVA for continuous variables. Predictors of conservative management were determined using a multinomial logistic regression model. The modeling process involved forward and backward stepwise methods with a threshold for exit set at p >0.10 and for enter at p <0.10. The aim was a parsimonious model, with the minimum number of variables per logit explaining the greater amount of variability. To determine independent predictors of mortality, proportional hazards model of Cox, that included all significant variables (with p value <0.05) in the univariate analysis, was used. We used SPSS, version 12.0, for Windows (SPSS Inc., Chicago, Illinois).
Results
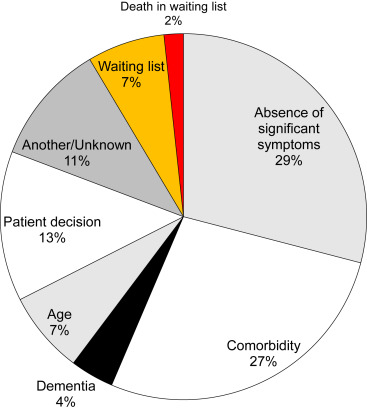
A total of 726 patients were included, mean age was 77.3 ± 10.6 years, and 377 were women (51.8%). The most common management strategy was conservative therapy in 468 (64.5%), followed by AVR in 199 (27.4%), and TAVI in 59 (8.1%). Table 1 lists the comparison of clinical and echocardiographic data according to management. Patients treated with AVR were younger, with less co-morbidity, and lower surgical risk than patients managed without open-heart surgery. They also presented higher creatinine clearance, higher valve gradients, and were less frequently women. Compared with patients treated with aortic valve interventions, patients treated conservatively were managed in tertiary hospitals less frequently, and presented lower aortic valve gradients. The variables independently associated with aortic valve intervention (AVR or TAVI) are listed in Table 2 . The strongest association found was patient management in a hospital with cardiac surgery. In the 468 patients with conservative treatment, the 2 main reasons to choose this option were the absence of significant symptoms and the presence of co-morbidities ( Figure 1 ). The local site investigators for the study disagreed with the decision of conservative treatment in 135 cases (28.8%). The rates of agreement with this decision were different according to the main reason to choose conservative treatment ( Figure 2 ).
| Variable | Conservative (N=468) | AVR (N=199) | TAVI (N=59) | P ∗ |
|---|---|---|---|---|
| Age (mean±SD) (years) | 79.0±10.9 | 72.2±9.1 | 80.6±5.7 | <0.001 |
| Women | 257 (54.9 %) | 87 (43.7 %) | 32 (54.2 %) | 0.03 |
| Charlson index (mean±SD) | 2.4±2.1 | 1.7±1.7 | 2.3±1.8 | <0.001 |
| EuroSCORE II (mean±SD) (%) | 4.5±5.9 | 2.9±3.2 | 5.8±9.0 | <0.001 |
| Creatinine clearence (mean±SD) (ml/min) | 60.9±24.8 | 71.1±22.5 | 57.2±16.4 | <0.001 |
| Cardiac surgery | 313 (66.9%) | 157 (78.9%) | 53 (89.8%) | <0.001 |
| Hospitalized patient | 152 (32.5%) | 62 (31.2%) | 25 (42.4%) | 0.26 |
| Echocardiography (mean±SD) | ||||
| Maximum aortic-valve gradient (mmHg) | 75.2±24.0 | 86.4±23.7 | 85.9±24.6 | <0.001 |
| Mean aortic-valve gradient (mmHg) | 45.6±15.4 | 52.9±15.6 | 52.5±16.4 | <0.001 |
| Aortic-valve area (cm 2 ) | 0.74±0.18 | 0.70±0.19 | 0.67±0.18 | <0.005 |
| Ejection fraction (%) | 60.9±11.8 | 60.7±11.8 | 57.9±14.5 | 0.22 |
| OR (95% CI) | p | |
|---|---|---|
| Age | 0.96 (0.94-0.97) | <0.001 |
| Charlson Index | 0.91 (0.83-1.0) | 0.047 |
| Maximum valve gradient | 1.03 (1.02-1.03) | <0.001 |
| Ejection fraction | 0.97 (0.95-0.98) | <0.001 |
| Tertiary hospital | 2.7 (1.8-4.1) | <0.001 |
During 1-year follow-up, 132 patients died (18.2%). The main causes of death were heart failure and noncardiac diseases ( Figure 3 ). Mean time from echocardiography to intervention was 114.4 ± 101.5 days for AVR versus 89.0 ± 98.2 days for TAVI, p = 0.09. One-year survival for patients treated conservatively, with TAVI, and with AVR was 76.3%, 94.9%, and 92.5%, respectively, p <0.001 ( Figure 4 ). Independent predictors of mortality are listed in Table 3 . Aortic valve intervention was independently associated with survival and TAVI seemed to be particularly beneficial for patients with high co-morbidity or high surgical risk ( Figure 5 ). One-year survival of patients treated conservatively in the absence of significant symptoms was 97.1% ( Figure 6 ).
| HR (95% CI) | p | |
|---|---|---|
| Charlson index | 1.2 (1.1-1.3) | <0.001 |
| Maximum valve gradient | 1.011 (1.003-1.018) | 0.004 |
| Ejection fraction | 0.98 (0.96-0.99) | 0.002 |
| EuroSCORE II | 1.06 (1.04-1.08) | <0.001 |
| Aortic valve intervention | 0.29 (0.18-0.49) | <0.001 |
| Hospitalized patient ∗ | 2.8 (1.9-4.0) | <0.001 |
| Creatinine clearance | 0.987 (0.977-0.996) | 0.005 |
∗ If echocardiography was performed in a patient that was hospitalized.
Results
A total of 726 patients were included, mean age was 77.3 ± 10.6 years, and 377 were women (51.8%). The most common management strategy was conservative therapy in 468 (64.5%), followed by AVR in 199 (27.4%), and TAVI in 59 (8.1%). Table 1 lists the comparison of clinical and echocardiographic data according to management. Patients treated with AVR were younger, with less co-morbidity, and lower surgical risk than patients managed without open-heart surgery. They also presented higher creatinine clearance, higher valve gradients, and were less frequently women. Compared with patients treated with aortic valve interventions, patients treated conservatively were managed in tertiary hospitals less frequently, and presented lower aortic valve gradients. The variables independently associated with aortic valve intervention (AVR or TAVI) are listed in Table 2 . The strongest association found was patient management in a hospital with cardiac surgery. In the 468 patients with conservative treatment, the 2 main reasons to choose this option were the absence of significant symptoms and the presence of co-morbidities ( Figure 1 ). The local site investigators for the study disagreed with the decision of conservative treatment in 135 cases (28.8%). The rates of agreement with this decision were different according to the main reason to choose conservative treatment ( Figure 2 ).



