Described herein is a 67-year-old woman who underwent replacement of both tricuspid and pulmonic valves because of severe isolated right-sided systolic heart failure. The cause of the heart failure preoperatively was believed to be the result of left breast radiation a year earlier. At operation, however, the pulmonic valve was excised and a biopsy of the stiff-walled right atrium was performed, and histologic examination of each was classic of carcinoid heart disease. She never awoke postoperatively. Postoperatively, computed tomography disclosed numerous masses in the liver. Retrospectively, clues to the presence of carcinoid heart disease include thickening of both the tricuspid and pulmonic valve leaflets by echocardiogram, a pressure gradient, albeit small, across the pulmonic valve, the plastering of the septal tricuspid-valve leaflet to the ventricular septum, the total absence of left-sided heart disease, and the presence of extremely low 12-lead QRS electrocardiographic voltage.
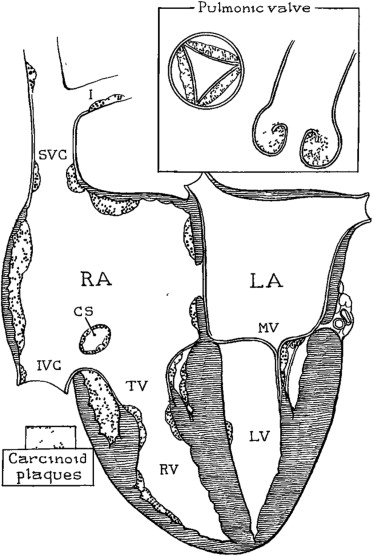
The most common cause of right-sided heart failure is left-sided heart failure. Isolated right-sided heart failure is far less common than that associated with left-sided heart failure, and usually results from pulmonary disease (parenchymal, vascular and/or bellows-system abnormalities), all of which produce pulmonary hypertension. Constrictive pericardial diseases and isolated congenital pulmonic-valve stenosis are far less common causes. Carcinoid heart disease as a cause of right-sided heart failure is rare, but distinctive clues to its presence are usually discernible ( Figure 1 ). This report describes a patient with undiagnosed carcinoid heart disease and discusses certain clinical clues which may have established the proper diagnosis and prevented the unsuccessful right-sided double-valve replacement.
Case Description
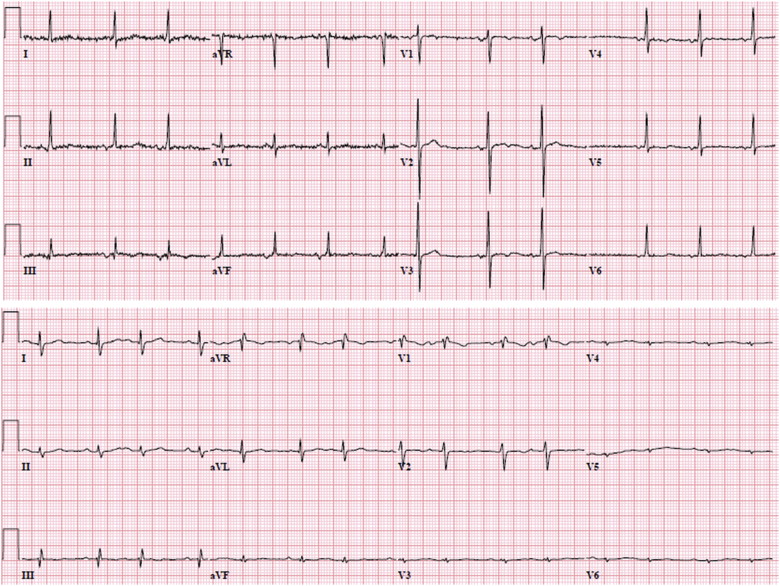
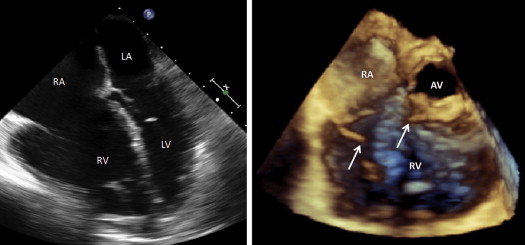
This 67-year-old white woman apparently had been in her usual state of health until age 57 when she had a knee replacement (December 2001) because of osteoarthritis. An electrocardiogram at the time showed total 12-lead QRS voltage to be 158 mm (measured with normal [10 mm] standardization [10 mm = 1 mV]) ( Figure 2 ). At age 66 (2012), she underwent left breast lumpectomy for confirmed cancer and received radiation to that breast and to the left axillary region. At age 67, peripheral edema, abdominal swelling, and weight gain appeared and each progressively worsened over a 6-month period during which time she gained 40 pounds. Examination in August 2013 confirmed the presence of anasarca. Facial flushing, diarrhea or labile blood pressure, if present, was not recorded. A precordial murmur was described as absent. An electrocardiogram now showed total 12-lead QRS of 51 mm; incomplete right bundle branch block and atrial premature complexes ( Figure 2 ). Echocardiogram disclosed both pulmonic and tricuspid valve regurgitation, thickening of both valvular leaflets, immobility of the tricuspid valve leaflets, severe dilatation of both right sided chambers, and no dilatation of the left-sided chambers ( Figure 3 ). Cardiac catheterization disclosed the following pressures in mm Hg: pulmonary artery, 30/10; right ventricle, 43/18; right atrial mean 18 with V wave 25 and pulmonary arterial wedge mean 8. The cardiac index was 1.4 L/min/m 2 . The left ventricular ejection fraction was approximately 60%. Coronary angiography disclosed insignificant narrowing (<30% diameter reduction).
In September 2013, the pulmonic valve was replaced with a homograft and the tricuspid valve, with a bioprosthesis (Edwards, Magna Ease). The tricuspid valve leaflets and chordae were sclerotic. Early postoperatively, excessive bleeding necessitated reexploration. Computed tomographic examination of the heart during the postoperative period disclosed an enlarged liver (23 cm in greatest dimension) containing innumerable masses ( Figure 4 ) and “… focal thickening of the cecum and terminal ileum.” During the entire 10-day post-operative period, the patient never awoke and had fatal multi-organ “failure”.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


