A presystolic wave (PSW) is commonly seen on Doppler examination of the left ventricular outflow tract (LVOT), but is little studied. We conducted a retrospective study to assess the prevalence of the PSW, correlations with various Doppler parameters, and its clinical significance. Two hundred echocardiograms, 100 with ejection fraction (EF) >55% and 100 with EF <45%, were reviewed. Mitral inflow velocities, septal annular velocities, LVOT, and PSW velocities were measured. Major adverse cardiovascular events (MACE [death, heart failure hospitalization, atrial fibrillation, and stroke]) were compared between those with and without a PSW, in both EF groups. Mean age was 58 ± 15 years; 56% were men and 69% were African-American. PSW prevalence was similar between normal (68%) and reduced EF groups (62%). However, its velocity was less in the low EF group (37 ± 10 vs 48 ± 16 cm/s, p <0.0001). In subjects with normal EF PSW velocity correlated with mitral A velocity (rho = 0.43, p = 0.0003). In subjects with reduced EF the association with A velocity was not significant (rho = 0.22, p = 0.09), but there was a significant association with annular a′ velocity (rho = 0.38, p = 0.002). Over a mean follow-up of 1.7 ± 0.3 years, 57 subjects (28%) experienced MACE. Those without a PSW had more MACE (39% vs 23%, p = 0.02); PSW absence remained predictive of MACE after adjustment for multiple variables, especially in patients with reduced EF. In conclusion, PSW is common in the LVOT. Its presence and magnitude are associated with measures of atrial contraction. Its absence is associated with increased rates of adverse events, especially in patients with low EF.
Highlights
- •
Presystolic wave (PSW) in the left ventricular outflow was seen in 65% of subjects.
- •
Presence and magnitude of PSW correlated with measures of atrial contraction.
- •
Absence of PSW was associated with increased rates of adverse events.
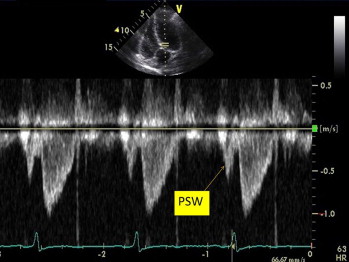
Mitral inflow and tissue Doppler annular velocities have been well validated for assessment of left ventricular diastolic function. The left atrium acts as a conduit in early diastole and as a pump in late diastole. In some patients, particularly those with reduced ejection fraction (EF), atrial contraction can be important in maintaining cardiac output. A presystolic wave (PSW; Figure 1 ) is a late diastolic event often seen on Doppler interrogation of the left ventricular outflow tract (LVOT). However, its prevalence, correlation with various Doppler echocardiographic parameters, and clinical significance have not been well described. The aims of this study were (1) to assess the prevalence of a PSW, both in normal EF and reduced EF cohorts; (2) to look for associations between the presence of a PSW and measures of atrial contraction and left ventricular compliance; and (3) to evaluate its clinical significance.
Methods
Consecutive Doppler echocardiograms, acquired on or after July 1, 2011, were reviewed until a study set of 200 was achieved; 100 with normal EF (>55%) and 100 with moderate to severe left ventricular systolic dysfunction (EF <45%). We deliberately excluded patients with EFs reported in the range of 45% to 55%, to clarify differences between the EF groups. Other exclusion criteria were nonsinus rhythm, valvular heart disease that was moderate or greater in severity, presence of a prosthetic valve in the aortic or mitral position, inadequate Doppler flow recordings in the LVOT or across the mitral valve, inadequate tissue Doppler of the mitral annulus, and fused E and A waves on Doppler examination of mitral inflow. For the normal EF group 298 echocardiograms were screened and for the low EF group 515 echocardiograms were screened to obtain 100 patients in each group. All studies were clinically indicated, and the study group included both inpatients and outpatients. This study was approved by the Institutional Review Board of the Einstein Healthcare Network.
Demographic and clinical data were collected from electronic medical records and included age, gender, race, height, weight, smoking history, history of hypertension, diabetes, and dyslipidemia. Body mass index and body surface area were calculated and recorded.
Doppler echocardiographic measurements were made per American Society of Echocardiography Guidelines for the evaluation of diastolic function. Mitral E- and A-wave peak velocities and velocity-time integral were obtained from pulse-wave Doppler in the apical 4-chamber view. Mitral annular velocities were obtained from pulse-wave tissue Doppler imaging performed in the apical views. Septal e′ velocity and septal a′ velocity were measured and E/e′ ratio was calculated to estimate left ventricular filling pressure. Pulse-wave spectral Doppler of the LVOT was evaluated in all patients by placing the pulse-wave sample volume in the LVOT, approximately 1 cm from the aortic valve. Peak LVOT velocity was recorded. The presence of a PSW preceding the LVOT flow was assessed in all patients. PSW peak velocity was obtained if a measurable PSW signal was present ( Figure 1 ). Left atrial volume was measured by the area-length method using apical 4-chamber and apical 2-chamber views at ventricular end-systole. It was indexed to body surface area to calculate the left atrial volume index.
Major adverse cardiovascular events (MACE) were defined as a composite of all cause death, heart failure hospitalization, atrial fibrillation occurrence, and ischemic stroke. These were obtained from the electronic database of Einstein Medical Center. Mortality data were obtained using the Social Security Death Index. Follow-up for MACE occurred until May 2013.
Data are reported as mean ± SD for continuous variables and as number and percentage for categorical variables. Baseline characteristics for patients with versus without PSW were compared in the normal and low EF groups using the t test for continuous variables and the chi-square test and/or Fisher’s exact test (as appropriate) for categorical variables. Parsimonious modeling (forward or backward or mixed) was used to assess echocardiographic variables significantly associated with a PSW. Logistic regression was performed to assess the independent relations between the PSW and clinical outcomes, namely death, heart failure hospitalization, atrial fibrillation, stroke, and a composite outcome of all these variables. A 2-tailed p value <0.05 was considered significant in advance. Statistical analyses were performed using JMP 9.0 (SAS, Cary, North Carolina).
Results
Baseline characteristics for the group as a whole and for the PSW and EF subgroups, are displayed in Table 1 . There were no significant differences in baseline characteristics between those with and without a PSW. However, comparing the normal and low EF groups, the latter were more likely to be men and hypertensive.
Variable | Total cohort (n=200) | Presystolic wave | p-value | Ejection Fraction | p-value | ||
|---|---|---|---|---|---|---|---|
| Absent (n=70) | Present (n=130) | Normal (n=100) | Low (n=100) | ||||
| Age (years) | 58 ±15 | 55 ± 17 | 58 ± 13 | 0.20 | 56 ± 17 | 58 ± 12 | 0.34 |
| Men | 111 (56%) | 36 (51%) | 75 (58%) | 0.29 | 44 (44%) | 67 (67%) | 0.003 |
| Asian | 11 (6%) | 3 (5%) | 8 (6%) | 5(5%) | 6(6%) | ||
| Black | 131 (69%) | 48 (75%) | 83 (66%) | 61 (66%) | 70(72%) | ||
| White | 33 (17%) | 9 (14%) | 24 (19%) | 21 (23%) | 12(12%) | ||
| Hispanic | 14 (7%) | 4 (6%) | 10 (8%) | 5 (5%) | 9(9%) | ||
| Hypertension | 140 (80%) | 46 (75%) | 94 (82%) | 0.32 | 59(73%) | 81(85%) | 0.04 |
| Diabetes mellitus | 62 (35%) | 23 (38%) | 39 (34%) | 0.61 | 25(31%) | 37(39%) | 0.26 |
| Dyslipidemia | 77 (44%) | 28(46%) | 49 (43%) | 0.67 | 32(40%) | 45(47%) | 0.29 |
| Smoker | 48 (27%) | 20 (33%) | 28 (24%) | 0.24 | 17(21%) | 31(33%) | 0.06 |
| Body mass index (kg/m 2 ) | 29±7.4 | 28.6±6.8 | 29.3±7.7 | 0.23 | 28.9±7.7 | 29±7.1 | 0.35 |
The overall prevalence of a PSW was 65%, with similar prevalence in the normal EF and low EF groups (68% vs 63%, p = NS). Echocardiographic variables by presence or absence of a PSW are listed in Table 2 . Compared with subjects without a PSW, subjects with a PSW had greater A-wave velocity, greater a′ velocity, and lower E/A and e′/a′ ratios. Table 3 lists echocardiographic variables significantly associated with PSW velocity after parsimonious modeling analysis. Overall, mitral A velocity and septal a′ velocity were significantly associated with PSW velocity. Interestingly, there was no significant difference in left atrial volume index between those with and without a PSW.
| Variable | Presystolic wave | p-value | |
|---|---|---|---|
| Absent (n= 70) | Present (n=130) | ||
| E (cm/s) | 78 ± 20 | 72 ± 22 | 0.06 |
| A (cm/s) | 66 ± 22 | 75 ± 19 | 0.006 |
| E/A ratio | 1.3 ± 0.6 | 1.0 ± 0.5 | 0.0003 |
| Septal e′ (cm/s) | 6.6 ± 3.0 | 5.8 ± 2.1 | 0.04 |
| Septal a′ (cm/s) | 6.6 ± 2.3 | 7.9 ± 1.8 | 0.0001 |
| E/e′ ratio | 14.4 ± 7.6 | 13.6 ± 5.6 | 0.42 |
| e′/a′ | 1.1 ± 0.6 | 0.8 ± 0.3 | <0.0001 |
| Left atrial volume index (ml/m 2 ) | 31.0 ± 10 | 29.0 ± 9.2 | 0.17 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


