Fig. 11.1
A 3D CT scan revealing multiple ipsilateral displaced rib fractures and a postoperative radiograph following open reduction and plate fixation. This fixation rapidly restored chest wall integrity and facilitated rapid weaning from mechanical ventilation
Ventilator Days
Patients suffering from flail chest injuries have a high likelihood of requiring mechanical ventilation. A recent review of data from the National Trauma Data Bank revealed that of 3,467 patients with flail chest injuries, 59 % required mechanical ventilation for a mean of 12.1 days [2]. These numbers increased in patients with concomitant head injuries.
Results of studies comparing rib fixation using modern techniques and implants to nonoperative management of flail chest injuries consistently demonstrate shorter mechanical ventilation times in patients treated operatively. A recent meta-analysis pooling the results of 11 clinical studies of operative treatment of flail chest injuries demonstrated a mean 7.5-day reduction in ventilator days in patients treated operatively compared with those managed nonoperatively. A similar result was seen (mean 8.3-day decrease) when the data from the randomized controlled trials alone were reviewed [3]. In the study of Ahmed et al., 21/26 patients with flail chest injuries treated with open reduction and internal fixation (ORIF) of their rib fractures were weaned from the ventilator in 1.3 days, with a mean ventilator time of 3.9 days, compared with a mean of 15 ventilator days in patients managed nonoperatively [1]. Even more dramatic results were seen by Kim et al., who demonstrated a 17-day mean difference in ventilator times of those treated operatively compared with those treated nonoperatively [5]. Lardinois et al. reported that immediate postoperative extubation following surgical fixation of flail chest injuries was possible in 47 % of patients, and the median length of postoperative intubation was only 2.1 days; no nonoperative control group was available for this study [6, 7]. Voggenreiter showed that early operative intervention (<48 h after injury) resulted in a mean ventilator time of 6.5 days and that operative treatment reduced ventilator days by a mean of 16.4 days [8]. The results of Althausen et al. support the decreased ventilator time in patients treated operatively [9]. In that series, patients treated operatively required a mean of 4.1 ventilator days, compared with 9.7 days in patients treated nonoperatively, with immediate postoperative extubation possible in 18 % of operatively treated patients (Table 11.1). In another series with matched cohorts of operatively and nonoperatively treated patients, Doben et al. demonstrated a decrease in mean ventilator days in patients that underwent surgical rib fixation (4.5 days vs. 16 days) compared with those treated nonoperatively [10].
Table 11.1
These data from Althausen et al. where 2.7 mm locking plates were utilized for operative fixation of flail chest injuries, summarizes the potential benefits of operative treatment of flail chest injuries
Operative patients (mean) | Nonoperative patients (mean) | p-Value | |
|---|---|---|---|
ICU LOS | 7.6 (7.43) | 9.7 (9.18) | 0.018 |
Hospital LOS | 11.9 (7.79) | 19.0 (12.64) | 0.006 |
Days on vent | 4.1 (6.66) | 9.7 (9.18) | 0.007 |
Tracheostomy | 13.6 % (3/22) | 39.3 % (11/28) | 0.042 |
Pneumonia | 4.6 % (1/22) | 25 % (7/28) | 0.047 |
Re-intubation | 4.6 % (1/22) | 17.9 % (5/28) | 0.034 |
Home O2 | 4.6 % (1/22) | 17.9 % (5/28) | 0.034 |
A recent prospective, randomized, controlled trial by Marasco et al. demonstrated a less dramatic reduction in ventilator support following rib fixation than many other studies. In this study, no significant difference was found in ventilator time between operative and nonoperative patients. The authors did, however, find a significant decrease in the duration of noninvasive ventilatory support and in ICU length of stay in patients treated operatively. There are a few potential explanations for this lack of improvement in ventilator time in operatively treated patients. First, the inclusion criteria for enrollment into the study were vague and, more importantly, subjective. In this study, patients were enrolled if they had a flail chest injury, were ventilator dependent, and had “no prospect of successful weaning within the next 48 h.” There were numerous exclusion criteria, which, when combined with subjective enrollment criteria, may have limited the patient population available for study to a greater extent than in prior studies. Additionally, the duration of ICU time prior to enrollment for patients in this study varied greatly. Operatively managed patients were enrolled at a mean ICU time of 61.6 h, with a standard deviation of 36.1 h, and nonoperatively managed patients were enrolled at a mean of 81.3 h, with a standard deviation of 84.2 h. Patients treated operatively remained in the ICU for a mean of 49.4 h after randomization until surgery or a mean ICU time prior to surgery of 111 h. Finally, while no significant difference in the time of mechanical ventilation was found between the two groups, a huge amount of variance within the data was noted. This great degree of variance, especially within the nonoperative group’s mechanical ventilation times, could potentially mask a true difference, particularly with a small sample size.
These studies demonstrate the need for further large-scale randomized trials with clear, objective inclusion and exclusion criteria.
Pneumonia and Septicemia
Although researchers have grappled with the exact definition, ventilator-associated pneumonia (VAP) is a well-described, dreaded, and potentially fatal complication of rib fractures and flail chest injuries. Reported rates of pneumonia in flail chest injuries vary and approach 100 % in some series when time of mechanical ventilation exceeds 8 days [11]. Dehghan et al. recently reported that the rate of pneumonia in 3,467 patients with flail chest injuries identified from the National Trauma Data Bank was 21 % [2]. Consequences of pneumonia secondary to flail chest injury can include increased antibiotic usage, increased need for mechanical ventilation, increased ICU length of stay (LOS), increased cost, sepsis, and death.
Some studies have demonstrated a reduction in the rate of pneumonia with operative treatment of flail chest injuries or rib fractures. In their meta-analysis, Slobogean et al. reported an odds ratio of 0.18 for the development of pneumonia in patients treated operatively compared with those treated nonoperatively. The number needed to treat reported in their study was three. This implies that for every three flail chest patients treated with rib ORIF, one case of pneumonia will be prevented. In seven of the eight studies reporting pneumonia as an endpoint included in the meta-analysis, the odds ratio for operative versus nonoperative treatment was found to significantly favor ORIF (odds ratio range 0.034–0.714). In the remaining study, although the rate of pneumonia was lower in the operative group, the odds ratio did not reach statistical significance. When the results of the randomized controlled trials alone were analyzed, an odds ratio of 0.06 (i.e. a patient treated with ORIF was almost 17 times less likely to develop pneumonia) was found [3]. Supporting these findings, Althausen et al. recently reported that 4.5 % of patients treated operatively developed pneumonia compared with 25 % of patients managed nonoperatively [9]. Even more dramatic results were demonstrated by Ahmed et al., with 50 % of nonoperatively managed patients developing “chest infection” compared with 15 % of those treated operatively. This reduction in pneumonia rates is likely in part due to the reduction in the mean number of ventilator days and likely contributes to a decrease in mean ICU LOS.
Septicemia is a dreaded complication of flail chest injuries and may occur secondary to the development of pneumonia. The meta-analysis of Slobogean et al. also reviewed the results of four studies reporting septicemia as an outcome and discovered an odds ratio of 0.36 favoring operative management (i.e. operatively treated patients had roughly one third the chance of developing septicemia than nonoperatively treated patients did), with a number needed to treat of 7 [3].
Tracheostomy
Tracheostomy is a procedure commonly associated with the long-term need for mechanical ventilation. Complications of tracheostomy include bleeding at the time of insertion, obstruction of the tracheostomy tube, and stomal infection [12]. The rate of tracheostomy for all patients with flail chest injuries was reported by Dehghan et al. to be 21 % from 2007 to 2009 [2]. Likely due to the fact that operative treatment of flail chest injuries has been shown to lead to shorter mean mechanical ventilation times, surgical fixation of rib fractures in flail chest injuries has been shown to reduce the rate of tracheostomy. Slobogean reported an odds ratio for tracheostomy of 0.12 for patients treated operatively compared with those treated nonoperatively [3]. In the series by Althausen et al., operative intervention reduced the need for tracheostomy from 39 % in patients treated nonoperatively to 13.6 % in those treated with chest wall ORIF (Figs. 11.2 and 11.3) [9]. Ahmed et al. demonstrated similar results, with 11 % of patients treated operatively requiring tracheostomy, compared with 37 % of patients treated nonoperatively [1]. Reduction in the need for tracheostomy not only helps avoid a secondary surgical procedure but also helps avoid its associated complications.



Fig. 11.2
This CT scan demonstrates impalement of the lung by a displaced posterior rib fracture (red arrow). This degree of visceral injury by a rib fracture represents, in itself, an indication for surgical extrication, fracture reduction, and fixation, irrespective of the overall injury pattern of the chest wall

Fig. 11.3
Another operative indication is seen on this CT scan that demonstrates lung tissue (red arrow) outside the chest wall. Again, lung herniation of this nature represents a specific indication for operative repair irrespective of the overall chest wall injury pattern
Pulmonary Contusion
Longer periods of mechanical ventilation and a higher rate of pulmonary complications have been noted by several authors when flail chest injury occurs with concomitant pulmonary contusion [8, 11, 13]. Voggenreiter et al. compared ventilator days in patients with flail chest injuries with and without pulmonary contusions managed nonoperatively. Patients with pulmonary contusions required a mean ventilator time of 30.8 days, compared with 6.5 days in patients without pulmonary contusions. Additionally, pulmonary contusion increased the mortality rate in operatively treated patients from 0 % to 30 % [8]. The direct effect of surgical fixation of flail chest injuries in patients with concomitant pulmonary contusions on duration of mechanical ventilation remains controversial, but current evidence would suggest a similar reduction in ventilator days with surgical stabilization.
Results of rib fixation for flail chest injuries in the setting of pulmonary contusion have been variable, and current data does not show the same success in improving ventilator and ICU times when compared with ORIF in patients without pulmonary contusion (Fig. 11.4). To date, the studies that have investigated the effect of pulmonary contusions in surgical treatment of flail chest injuries—most notably the Voggenreiter study—have been limited by small sample sizes, particularly in the groups with pulmonary contusions. Additionally, small retrospective studies such as the Voggenreiter study can be limited by selection bias with regard to how patients with pulmonary contusions are treated (operative vs. nonoperative).
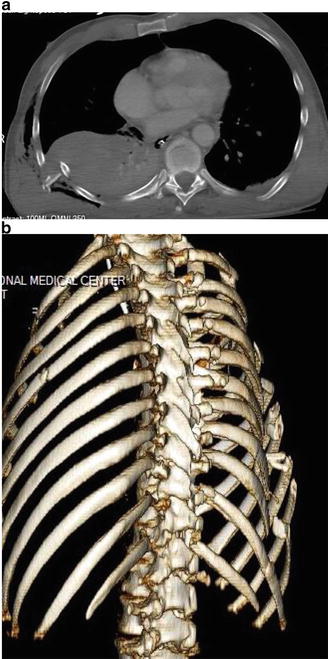
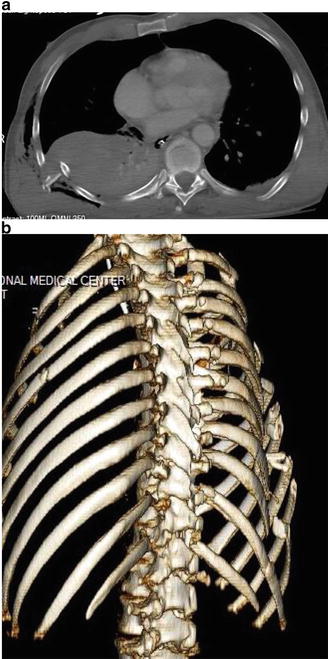
Fig. 11.4
A CT scan (a) demonstrates severe displacement of multiple posterior rib fractures with significant underlying soft tissue injury including hemothorax and pulmonary injury. A 3D CT scan (b) confirms the injury pattern and assists in the surgical planning: this pattern of injury (multiple ipsilateral segmental rib fractures with displacement) represents the most common current indication for operative fixation of the chest wall
Ultimately, in these cases, the pulmonary contusion may be the rate-limiting factor for liberation from the ventilator, and ORIF may not be of substantial benefit. Further investigation into the effect of pulmonary contusions on the outcome of flail chest injuries is certainly warranted.
Mortality
Mortality in trauma patients is a multifactorial entity, and it can be very difficult clinically and statistically to demonstrate differences in mortality with specific interventions. Regardless of treatment modality, flail chest injuries are life-threatening injuries irrespective of associated injuries. Dehghan et al. reported the overall mortality rate of patients with flail chest injuries to be 16 % based on data from 2007 to 2009 in the National Trauma Data Bank [2]. The difference in mortality between nonoperatively and operatively managed patients is difficult to determine as most retrospective studies lack a comparative or control group. However, current data indicates that there may be a reduction in mortality for operatively treated flail chest patients.
The mortality rates of patients with flail chest injuries treated nonoperatively reported in the current literature are alarmingly high. Ahmed et al. reported a mortality rate of 29 % in nonoperatively managed patients [1]. Voggenreiter et al. reported a 39 % mortality rate in patients with flail chest injuries and without pulmonary contusions managed nonoperatively [8]. Balci et al. noted similarly poor results, with 21–33 % mortality in nonoperatively treated patients [14]. Landercasper et al. noted a lower rate of mortality, with 13 % of patients expiring during the initial hospitalization and an additional 8 % expiring between 1 month and 9 years of the injury [15]. Rib fractures alone imparted a 5.7 % mortality rate in the report by Sirmali et al., with a 3.3 % mortality rate due to pulmonary causes. In the subgroup of patients with rib fracture who expired due to pulmonary causes, patients with >6 rib fractures accounted for 85 % of deaths [16].
Most studies that report mortality data in patients with flail chest injuries treated operatively report lower mortality rates than patients treated nonoperatively. Pooling the data from 7 studies and 582 patients, Slobogean found an odds ratio for mortality of 0.31 in patients treated operatively versus those treated nonoperatively and a number needed to treat of only five (treating five patients operatively prevented one death) [3]. Ahmed et al. report an 8 % mortality rate in patients treated operatively compared with a 29 % mortality rate in those treated nonoperatively [1]. Similarly, Mouton et al. reported an 8.7 % mortality rate in patients treated operatively (there was no nonoperative cohort in this study) [7], and Lardinois et al. report an 11 % mortality rate in patients undergoing surgical stabilization (no nonoperative cohort) [6]. Despite demonstrating 21–33 % mortality in nonoperative patients, Balci et al. reported a substantial improvement in operative patients, who had a 10 % mortality rate [14]. Although limited by small numbers in each group, Voggenreiter et al. reported 100 % survival in patients with flail chest injuries (without pulmonary contusions) treated operatively [8]. In this series, operatively treated patients with pulmonary contusions fared significantly worse, with a mortality rate of 30 %. Despite the notable increase in mortality rate associated with pulmonary contusion, these patients still showed a lower mortality rate than nonoperatively treated patients without pulmonary contusions, who suffered an extremely high 39 % mortality rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


