Chronic Venous Insufficiency—Postthrombotic Syndrome
JOSEPH D. RAFFETTO
Presentation
A 45-year-old male presents with a 5-year history of left lower extremity swelling, which is progressive over the course of the day. The swelling involves his leg and knee and extends into the thigh. The patient wears 30 to 40 mm Hg thigh-high compression stockings. His past history is significant for traumatic injury of the back at age 35, which required an anterior open fusion of his L4-L5 spine. The surgery was complicated by a hematoma requiring an exploratory laparotomy. One week later, the patient developed a venous thromboembolism (VTE) requiring an inferior vena cava (IVC) filter. Given his progressive edema, he underwent left iliac angioplasty 3 year ago with minimal relief. His pulse exam is normal, there are no skin changes or ulcers, and he has no other medical issues.
Differential Diagnosis
Both the clinical history and presentation are suggestive of a chronic venous insufficiency and postthrombotic syndrome. In addition, his history of iliac vein angioplasty is suggestive that he has a central venous problem in the iliac vein. Because of his history of VTE, one needs to consider recurrent deep venous thrombosis. Other possibilities of unilateral edema are infection, lymphedema, trauma, and tumors.
Workup
Color flow duplex ultrasound was performed and demonstrated recanalized left femoral vein with chronic thrombus that was not occlusive and flow in the vein (Fig. 1). Further evaluation determined that the left popliteal vein had chronic recanalized thrombus with venous flow (Fig. 2A), but significant reflux (4.84 seconds) in the popliteal vein (Fig. 2B). The common femoral vein (CFV), deep femoral vein (DFV), tibial veins, and great/small saphenous veins were all normal. The suggestion of central vein obstruction and significant swelling that involved both the leg and thigh warranted further evaluation of the iliac venous system. A computerized axial tomographic venography (CTV) demonstrated a patent IVC (Fig. 3A), a severely compressed left common iliac vein (CIV, Fig. 3B), a patent left external iliac vein (EIV) but with postthrombotic changes (Fig. 3C), and patent left femoral vein but with chronic postthrombotic changes (Fig. 3D). Both the ultrasound and CTV favor a diagnosis of chronic venous insufficiency with postthrombotic syndrome and CIV obstruction. In fact, there is no suggestion of pelvic tumors in the pelvis and no evidence of infection or clinical presentation of lymphedema.
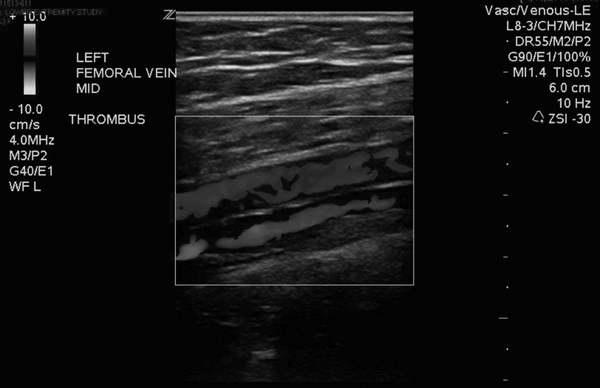
FIGURE 1 Color flow duplex ultrasound (CFDUS) demonstrating the femoral vein (blue on CFDUS, the red color is the femoral artery). Note the irregularity on the vein wall.
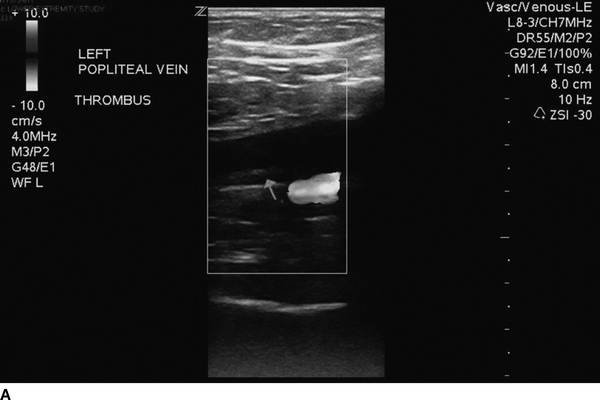
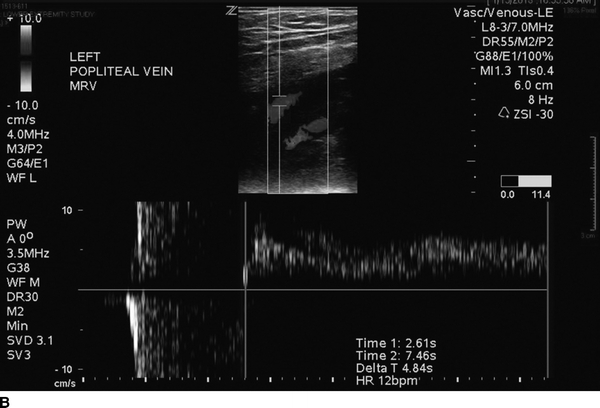
FIGURE 2 A: Color flow duplex ultrasound (CFDUS) demonstrating the popliteal vein (arrow) with chronic thrombus (hyperechoic). B: Spectral Doppler waveform demonstrating reflux in the popliteal vein of 4.84 seconds.



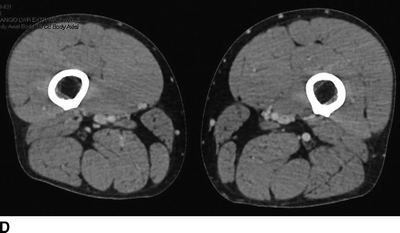
FIGURE 3 Computerized tomographic venography of inferior vena cava, iliac and femoral veins. A: Normal inferior vena cava. B: Compressed left iliac vein, note metallic prosthesis in the lumbar spine. C: Left external iliac vein patent with minimal post-thrombotic changes (right external iliac vein patent and normal). D: Left femoral vein patent with post-thrombotic changes (right femoral vein patent and normal).
Diagnosis and Treatment
The patient’s symptoms are related to several problems. He has postthrombotic syndrome secondary to recanalized chronic DVT with severe reflux in the popliteal vein, which explains the leg edema; however, the edema of the lower extremity extends into the thigh, suggesting that the CIV obstruction and EIV with a postthrombotic recanalized vein are also contributing to the problem. The primary treatment of postthrombotic syndrome is compression therapy. Vein valve transplantation is reserved for patients with recalcitrant venous ulcers and skin changes, which the patient does not exhibit. There is no indication or studies to support endovascular angioplasty and stent treatment of the femoral-popliteal recanalized vein segments. Importantly, given the central venous obstruction, both surgical and endovascular approaches need to be considered to relieve the venous hypertension in the limb. Endovenous treatment of iliofemoral or iliocaval obstruction is the primary treatment modality, and open surgical venous reconstruction techniques are reserved for failed endovenous procedures.
Surgical Approach
Endovenous procedures involving the iliac vein and IVC can be approached from either the femoral vein or popliteal vein. Procedures should be performed in a fixed imaging suite for optimal imaging, reduction in radiation exposure, and safety. Approaching from the popliteal vein provides further options to treat the entire iliac vein, including stenting into the CFV if needed, but this is usually reserved for acute DVT of the iliofemoral region. In addition, if there is segmental occlusion of the femoral vein, a popliteal approach would not be favorable. In chronic postthrombotic iliocaval and iliofemoral vein obstruction, the common femoral vein or femoral vein is the optimal access site. All venous access sites should be performed under ultrasound guidance to avoid the artery, especially in the femoral region, and by micropuncture technique. In this patient, the CFV approach was performed with ultrasound-guided micropuncture with a 0.018-inch wire and 5-French sheath, since the most significant problem was in the left CIV and proximal EIV. The patient is administered intravenous heparin. Venography is performed via the side port of the sheath and in multiple views including anterior-posterior (AP), right anterior oblique (RAO), and left anterior oblique (LAO) in order to provide the required information of the venous anatomy (Fig. 4A–C). The venogram demonstrated a compressed left CIV in the area of the lumbar spine hardware and postthrombotic trabeculations within the EIV. It is important to note that venography can be normal in appearance, but it does not exclude the possibility of iliac vein obstruction, hence the importance of using intravascular ultrasound (IVUS).
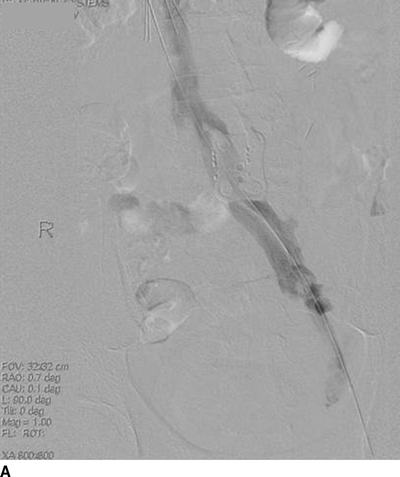
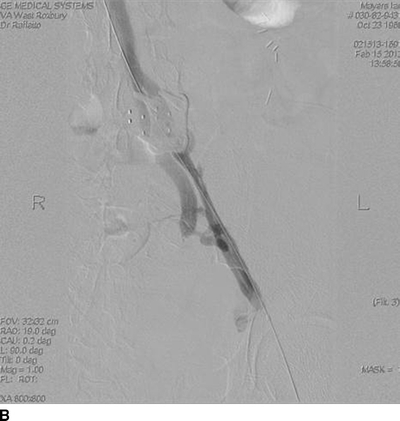
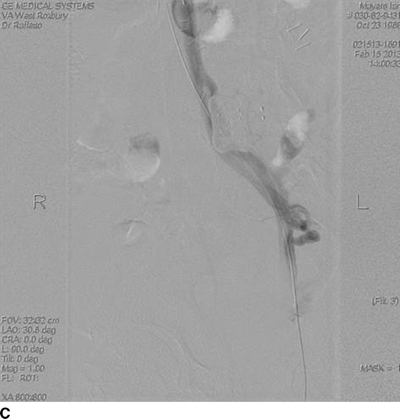
FIGURE 4 Venography of the left iliofemoral veins. A: Anterior-posterior view, note compression of the left common iliac vein, but contrast is lightly opacifying the vein. B: Right anterior oblique view, persistent compression of the left common iliac vein, with visualization of left internal iliac vein, and narrowed but patent left external iliac vein. C: Left anterior oblique view, with compression of the left common iliac vein.



