Cardiovascular (CV) assessment in prerenal transplant patients varies by center. Current guidelines recommend stress testing for candidates if ≥3 CV risk factors exist. We evaluated the CV assessment and management in 685 patients referred for kidney transplant over a 7-year period. All patients had CV risk factors, and the most common cause of end-stage renal disease was diabetes. Thirty-three percent (n = 229) underwent coronary angiography. The sensitivity of stress testing to detect obstructive coronary artery disease (CAD) was poor (0.26). Patients who had no CAD, nonobstructive CAD, or CAD with intervention had significantly higher event-free survival compared with patients with obstructive CAD without intervention. There were no adverse clinical events (death, myocardial infarction, stroke, revascularization, and graft failure) within 30 days post-transplant in patients who had preoperative angiography (n = 77). Of the transplanted patients who did not have an angiogram (n = 289), there were 8 clinical events (6 myocardial infarctions) in the first 30 days. In conclusion, our results indicate that stress testing and usual risk factors were poor predictors of obstructive CAD and that revascularization may prove beneficial in these patients.
Chronic kidney disease is a potent risk factor for cardiovascular disease (CVD) and a significant harbinger of morbidity and mortality. The risk of CV complications and death is particularly high for patients with end-stage renal disease (ESRD). Although kidney transplantation improves morbidity and mortality in ESRD, CVD remains the primary cause of death. There exists a need to ensure that recipients are optimized from a CV standpoint before transplantation. Past and current guidelines and position statements are limited by a lack of randomized data as these data do not exist, which results in considerable variability in assessments that are performed. The 2012 American Heart Association/American College of Cardiology (AHA/ACC) consensus statement regarding CV evaluation before kidney and liver transplantation recommends preoperative stress testing only if at least 3 CV risk factors are present but only as a IIb recommendation. In contrast, some transplant centers use a more aggressive angiographic and revascularization strategy, which may improve survival in these patients. Here, we report our experience with the CV assessment and management in patients with ESRD being evaluated for renal transplantation.
Methods
The study was approved by the University of Utah Institutional Review Board (IRB project #00069927). All consecutive patient records who were referred for kidney transplantation from January 2007 to December 2013 were reviewed. These patients were presented at the Kidney Transplant Selection Committee (KTSC) at the University of Utah, a large, tertiary academic referral center for a 6 state region. The KTSC comprised a multidisciplinary team of transplant nephrologists, transplant surgeons, and other specialized support staff. During the study period, a cardiologist was not part of the KTSC. Data were gathered prospectively by support staff and recorded in the minutes of the KTSC meeting. These minutes and the patients’ electronic health records were then systematically reviewed and entered into a database. Patients were excluded if they were <18 years or if they had not been evaluated in the prerenal transplant clinic before being presented at the KTSC. The database comprises demographic information and the 8 risk factors according to the AHA/ACC consensus statement (age >65 years, history of CVD, left ventricular hypertrophy, diabetes mellitus, hypertension, hyperlipidemia, smoking, and dialysis >1 year). The patient’s preoperative CV assessment (i.e., stress testing, angiography, echo, etc.) was also recorded. At the conclusion of the KTSC, a patient was either felt to be at acceptable risk for listing/transplantation or excluded from listing/transplantation. Exclusion reasons were also recorded in the database.
Clinical end points were defined as death, nonfatal myocardial infarction (MI), stroke, revascularization, and graft failure defined as the need for permanent (>3 months) renal replacement therapy after transplant.
The KTSC reviewed the baseline CV assessment in all patients that included a detailed history and examination and any testing that had been done by the referring provider. There were no set protocols used by referring providers or transplant nephrologists/surgeons for CV assessment. It was typical for the KTSC to recommend or require that at least some CV assessment be done in all patients, at a minimum an electrocardiogram and echocardiogram at rest if not done before. Most patients underwent some form of stress testing and/or angiography before or at the recommendation of the KTSC. Some of the patients were referred for angiography even in the setting of a negative stress test based on high pretest suspicion. The decision to revascularize obstructive coronary artery disease (CAD) found at the time of angiography was left to the discretion of the interventional cardiologist and transplant nephrologist. Obstructive CAD was typically defined as a major epicardial coronary artery stenosis of >70% and/or a fractional flow reserve value of ≤0.8.
All statistical analyses were performed with SAS, version 9.4 (SAS Institute Inc., Cary, North Carolina). Descriptive summaries were generated for pertinent and clinically relevant variables and examined to ensure complete and reasonable ranges. An α = 0.05 was considered statistically significant. All hypothesis tests were 2 sided, all p values are nominal, and no adjustments were made for multiple comparisons. Survival analyses were performed with PROC LIFETEST using the Kaplan-Meier method and differences compared with log-rank test. Logistic regression was performed with PROC LOGISTIC without stepping.
Results
A total of 685 consecutive patients over a 7-year time period were included in the analysis. The majority were men (56%) with a mean age (±SD) of 48 ± 15 years at the time of evaluation. At least one of the 8 risk factors was present in all patients. The most common risk factor was hypertension. Most patients (n = 480, 70%) underwent some form of stress testing as part of their workup ( Table 1 ).
| Age (years) | 48 ±15 |
| Male | 386 (56%) |
| Female | 299 (44%) |
| Body mass index (kg/m 2 ) | 28 ± 5 |
| Age >60 | 195 (28%) |
| Prior diagnosis of CVD | 109 (16%) |
| Hypertension | 574 (84%) |
| Hyperlipidemia | 280 (41%) |
| Diabetes Mellitus | 252 (37%) |
| Smoker | 43 (6%) |
| Dialysis >1 year | 268 (39%) |
| Left ventricular hypertrophy | 85 (12%) |
| ESRD etiology | |
| Diabetes mellitus | 216 (32%) |
| Hypertension | 65 (9%) |
| Graft failure | 108 (16%) |
| Other | 296 (43%) |
| Angiogram performed | 229 (33%) |
| Transplanted | 77 (43%) |
| Awaiting transplant | 126 (55%) |
| Denied transplant | 26 (11%) |
| Received renal transplant | 366 (53%) |
| Stress test | 247 (67%) |
| Angiogram | 77 (21%) |
| No stress test nor angiogram | 42 (11%) |
| Living donor | 123 (34%) |
| Denied transplant | 88 (13%) |
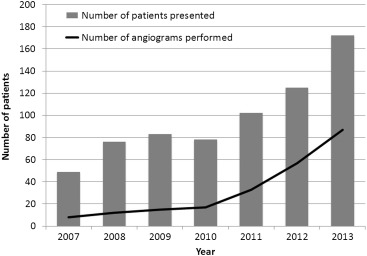
The number of new patients presented at the KTSC meeting increased annually during the study period as did the number and percentage of patients who had a coronary angiogram as part of their pretransplant assessment ( Figure 1 ).
There were 64 patients who were initially considered unsuitable for transplantation and were, therefore, denied waitlisting/transplantation. In addition, 24 patients were later deemed unsuitable for transplantation for a total of 88 patients denied waitlisting/transplantation. Although there were a variety of reasons to not proceed with transplantation, the most common reason was because of CV disease ( Table 2 ). There were 15 clinically significant end points during the follow-up period of those 88 patients including 13 deaths. Twelve of the 13 deaths (92%) were attributed to CVD.
| Reason for Denial | Number Denied |
|---|---|
| Cardiovascular | 25 |
| Psychosocial | 19 |
| Co-morbidity | 18 |
| Oncology | 10 |
| Pulmonary | 7 |
| Patient refusal | 3 |
| Gastroenterology | 2 |
| Obesity | 2 |
| Urologic | 1 |
| Infectious disease | 1 |
Of the 685 patients, 229 (33%) underwent coronary angiography. Of those who underwent coronary angiography, 31% had obstructive CAD, 46% had nonobstructive CAD, whereas only 23% had normal angiographic coronary arteries. Of the 72 patients with obstructive CAD, 60 (83%) underwent some revascularization procedure (16 = coronary artery bypass grafting [CABG] and 44 = percutaneous coronary intervention). Of the 229 patients, 28 (12%) were considered to be unsuitable for transplant and 16 of 28 deemed unsuitable because of CVD. Of those 16 patients who were deemed unsuitable because of CVD, 6 went on to a revascularization procedure (3 PCI and 3 CABG) as recommended during their transplant workup; however, they were subsequently deemed unsuitable regardless. Four of those 28 patients died during the follow-up period.
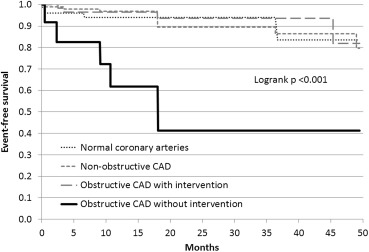
Event-free survival was no different between those with angiographically normal coronary arteries, those with nonobstructive CAD, and those with revascularized CAD. Those 3 groups all had a significantly higher event-free survival compared with the patients who had obstructive CAD but were not revascularized (log-rank p <0.001 comparing all 4 groups, p <0.0001 comparing those with obstructive CAD without revascularization to all others with angiography) ( Figure 2 ).
Most of the angiographic cohort (174 of the 229, 76%) underwent some form of stress testing before coronary angiography. Stress testing sensitivity to detect obstructive CAD was poor (0.26). In a multivariable regression analysis, the only risk factor that predicted the presence of obstructive CAD with statistical significance was a history of known CVD. The other risk factors failed to predict the presence of obstructive CAD ( Table 3 ). Indeed, even age of those with obstructive CAD (ages 24 to 77) entirely overlapped with patients who had normal coronary arteries (ages 24 to 74).
| Risk factor | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Age (per year) | 1.02 | 0.99-1.04 | 0.27 |
| Male | 1.27 | 0.68-2.3 | 0.46 |
| History of CVD ∗ | 2.42 | 1.20-4.9 | 0.014 |
| Diabetes | 1.56 | 0.81-3.0 | 0.19 |
| Hypertension | 1.18 | 0.46-3.0 | 0.73 |
| Hyperlipidemia | 1.41 | 0.66-3.0 | 0.37 |
| Smoking | 1.01 | 0.36-2.9 | 0.98 |
| LVH | 2.00 | 0.81-4.90 | 0.13 |
| Dialysis >1year | 1.02 | 0.56-1.9 | 0.94 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


