Cardiovascular Manifestations of Rheumatic Diseases
Nicola J. Goodson
Daniel H. Solomon
Introduction
The rheumatic diseases encompass a broad spectrum of conditions, all of which primarily cause joint and musculoskeletal pathology. It has long been recognized that cardiac pathology occurs in association with many rheumatic conditions. Until recently, most accepted that cardiac involvement took the form of structural abnormalities such as pericardial disease or valvulopathies. However, many chronic inflammatory rheumatic conditions appear to be associated with premature atherosclerotic disease and a reduced life expectancy. There is emerging evidence that chronic inflammation is associated with the occurrence of cardiac events in people both with and without chronic inflammatory joint disease. However, both atherosclerosis and many rheumatic diseases have a complicated etiology and it is likely that inflammation contributes to other environmental and host risk factors in these patients.
Cardiovascular disease (CVD) is common in many inflammatory arthritides and, as much of this remains clinically silent, it is difficult to measure the true incidence and prevalence of cardiovascular involvement in each rheumatic condition (Table 35E.1). This chapter discusses the cardiovascular involvement in many of the more common rheumatologic conditions. Many treatments used in rheumatic conditions also have potential cardiovascular effects, and these are discussed later.
Cardiac Involvement in Osteoarthritis
It is unclear whether there is a direct link between osteoarthritis and CVD. Obesity is a common risk factor for both conditions. The sedentary lifestyle that often accompanies osteoarthritis of the lower extremities may predispose toward CVD. There are some data to suggest that the cardiovascular risk profile in patients with osteoarthritis is more severe than the non-osteoarthritis population (1). However, one large population-based study did not find an increase in the risk of cardiovascular outcomes in patients with osteoarthritis compared with non-arthritis subjects (2).
Cardiac Involvement in Rheumatoid Arthritis
Rheumatoid arthritis (RA) is one of the more common rheumatic conditions, affecting approximately 0.5% to 1.0% of the adult population. The incidence of RA rises with
increasing age, and females are affected two to three times more frequently than males. The underlying etiology is not known. However, genetic, host, and environmental risk factors for RA have been identified that influence susceptibility and progression of the disease (3).
increasing age, and females are affected two to three times more frequently than males. The underlying etiology is not known. However, genetic, host, and environmental risk factors for RA have been identified that influence susceptibility and progression of the disease (3).
TABLE 35E.1 Prevalence of Rheumatic Disorders and Summary of Cardiovascular Involvement | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
RA is characterized by widespread chronic inflammation of synovial tissues, in a symmetrical distribution, that leads to joint damage and disability. Although RA is primarily an inflammatory disease of joint tissues, it has systemic effects and can involve many organ systems including the cardiovascular system.
Patients with RA have a reduced life expectancy when compared to the general population. This equates to an average loss of 4 to 8 years of life. Although it is known that RA patients have increased mortality from infections, renal disease, gastrointestinal disorders, and lymphoproliferative disease, these causes of death represent only a small proportion of all RA deaths (4). CVD is responsible for 35% to 50% of all RA deaths and most of the excess mortality observed in RA cohorts is due to increased rates of CVD mortality (5,6,7,8).
Excess mortality is not just limited to clinic based cohorts of established RA patients as study of community based RA cohorts and early inflammatory polyarthritis cohorts have also demonstrated excess CVD mortality (9,10). This suggests that mechanisms which promote CVD mortality are not restricted to patients with severe RA and are also present early in the RA disease process (11).
Structural cardiac lesions including pericarditis and nonspecific mitral and aortic valve abnormalities are commonly described in autopsy series and echocardiographic studies of RA patients. However, these lesions usually remain clinically silent and rarely lead to significant hemodynamic disturbances. Therefore, it is difficult to record the prevalence of this “rheumatoid heart disease” and assess how it contributes to the excess CVD mortality observed in RA patients.
More recently, there has been much interest in coronary heart disease (CHD) in RA. This condition has been shown to be highly prevalent in RA cohorts. It is also often asymptomatic and frequently diagnosed at autopsy. However, CHD in RA is not a benign disease and appears to be responsible for much of the observed excess mortality. Indeed, CHD appears be the single largest cause of CVD deaths in RA populations (8,12,13).
Pericardial Disease
Rheumatoid pericarditis was first described by Charcot in 1881 (14) and is thought to be a common CVD manifestation of RA (Fig. 35E.1). Autopsy studies have reported pericardial disease in up to 50% of RA patients (15) and more recently echocardiographic studies have reported that pericardial disease occurs in up to 30% of RA cases (16). However, clinically significant pericarditis is observed infrequently in RA, affecting fewer than 2% of patients (17,18). It is possible that the prevalence of pericarditis in RA is declining because of more effective disease-modifying antirheumatic drugs (DMARD) or because RA is becoming a less severe disease (19). Pericarditis is associated with increased disease severity and is more common in male RA patients. Patients are usually rheumatoid factor positive and they frequently have rheumatoid nodules and erosive joint disease. Systemic symptoms are common and include fatigue, weight loss, and other extraarticular system involvement (18).
The pericardial fluid is classically exudative containing leukocytes, elevated levels of lactate dehydrogenase, and a low concentration of glucose, but these findings are not universal (18). Chronic inflammation can cause thickening of the pericardium that can lead to constrictive pericarditis, which is a rare sequela of severe or recurrent pericarditis in RA (20). Calcification of the pericardium is rarely seen in RA pericarditis (21). Pericardial effusions that develop owing to infection are rarely seen in RA. However, if there is any suspicion that the pericarditis may be infectious, cultures for tuberculosis and fungi as well as standard culture of pericardial fluid should be obtained; many RA patients are immunosuppressed by their DMARDs.
The vast majority of patients respond to treatment with non-steroidal anti-inflammatory drugs (NSAIDs). After infection has been ruled out, short courses of oral steroids may be used, and DMARD therapy should be increased to control active rheumatoid disease. Colchicine has been used to treat recurrent non-RA pericarditis; however, it is not clear whether this is beneficial in RA pericarditis (22).
Endocardial and Valve Involvement
There are rare case reports of rheumatoid nodules affecting the endocardium or heart valves causing valve dysfunction. In particular, there have been several reports of aortic valve nodulosis causing regurgitation requiring aortic valve replacement (23,24) and mitral valve nodules causing embolic disease (25). There has also been one report in the literature of an endocardial nodule mimicking an atrial myxoma (26).
Based on autopsy studies, diffuse endocardial involvement in RA appears to be a relatively common manifestation of RA (27). Valvular abnormalities are frequently seen on echocardiographic studies and it has been hypothesized that heart valve involvement may be an additional extraarticular manifestation of RA (28). Hospital-based studies report a prevalence of nonspecific aortic and/or minimal mitral regurgitation in 5% to 30% of RA patients (29,30,31). Mitral valve insufficiency seems to be associated with nodular RA, which suggests that heart valve involvement reflects more severe RA disease (32). It appears
that the valve lesion is due to infiltration of inflammatory cells that leads to thickening and calcification at the base of the valve and valve ring (27,33). However, symptomatic valve disease is a very rare manifestation of RA.
that the valve lesion is due to infiltration of inflammatory cells that leads to thickening and calcification at the base of the valve and valve ring (27,33). However, symptomatic valve disease is a very rare manifestation of RA.
Myocardial and Conduction System Involvement
Myocarditis occurs in RA either as the result of focal granulomatous disease affecting the myocardium or more diffuse fibrosing lesions, and is a common finding at autopsy (33). It is commonly asymptomatic, but may lead to the development of cardiac failure or disruption of the conducting system of the heart.
It seems that ECG evidence of conduction abnormalities and arrhythmias are common in patients with RA. One study reported that 50% of RA patients had evidence of cardiac arrhythmias on 24-hour ECG monitoring, although this arrhythmia prevalence was similar to that seen in a hospital-based non-RA control group (34). Another study reported a higher prevalence of abnormal ventricular repolarization in RA patients compared to control patients (35). Complete heart block (CHB) has been described in association with RA, possibly due to disruption of the atrioventricular (AV) node by rheumatoid granulomata (36,37). Autonomic nervous system disturbance has been observed in RA cohorts (38,39), which may be a risk factor for silent CVD events (40,41).
Coronary Artery Disease
There is increasing evidence that RA patients have an increased prevalence of CHD due to atherosclerosis. This appears to be responsible for much of the excess CVD mortality observed in RA. Several studies have shown that RA patients have a two- to threefold increase in rates of myocardial infarction (MI) when compared to the general population (42,43). In addition, Maradit-Kremers et al. (41) have highlighted that RA patients are more likely to experience silent ischemia and sudden cardiac death. In one UK RA cohort cardiovascular admissions were not increased despite increased cardiovascular mortality (8). Therefore, it is possible that the true prevalence of CHD events in RA is underestimated by these hospital-based studies. Also patients who fail to present with typical CHD symptoms are unlikely to benefit from interventions to improve CHD outcomes. There is a need to educate both physicians and patients to be more aware that CHD events may not present typically in association with RA.
TABLE 35E.2 Cardiovascular Effects of Rheumatic Disease Medications | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||
Several CVD risk factors, including cigarette smoking and obesity, have also been identified as risk factors for the development of RA (44). Some of these, including age, smoking, hypertension, and lipid levels have been associated with subclinical atherosclerosis in RA (45). Cigarette smoking is associated with more severe RA and it may be this disease severity and inflammation that promotes atherosclerosis in RA. However, studies of RA populations have not found that traditional CVD risk factors explain the increased CVD events seen in these patients (42,43). One study revealed that a low body mass index (BMI) was associated with increased CVD mortality and it has been hypothesized that a low BMI reflects increased inflammatory disease burden in RA (46). This demonstrates how difficult it is to separate the effects of the RA disease activity from the effects of CVD risk factors when investigating CVD in RA.
CVD epidemiology in the general population has revealed the importance of several novel CHD risk factors including homocysteine, thrombotic markers, insulin resistance, and markers of inflammation (47). There is a high prevalence of these “novel” risk factors in patients with inflammatory joint disease. Patients with RA have been found to have abnormal homocysteine metabolism (48), which may be exacerbated further by the use of methotrexate or sulphasalazine (49). However, it is not known whether elevated homocysteine levels predict future CHD events in RA patients. Thrombotic markers may be increased in RA due to systemic inflammation and have been associated with CHD events in RA (50). Insulin resistance has been recognized to complicate RA. It is also associated with inflammation, obesity, steroid use, and CVD (51). Of particular interest in RA is the association between inflammation and CVD. Atherosclerosis is now thought to be an inflammatory condition (52) and prospective study has recognized markers of inflammation, including C-reactive protein (CRP), are predictors of future CHD events in both the general (53) and in inflammatory polyarthritis populations (54). Other studies have found that erythrocyte sedimentation rate (ESR) measurements predict CHD events in RA (55). It seems that in RA an elevated CRP is associated with endothelial dysfunction (56), which may promote atherosclerosis in RA patients.
Understanding the pathogenesis of CHD in RA is complicated; several factors, including inflammation, RA disease severity, and cardiovascular risk factors, all interact with each other. It may be that with a combined approach, allowing for modification of CHD risk factors and reduction of inflammation using immunosuppressive agents, the cardiovascular mortality in RA can be reduced. Although coronary arteritis is observed at autopsy in 10% of RA cases (27), this rarely leads to MI or damage.
Cardiac Involvement in Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a common chronic inflammatory disease that involves the sacroiliac joints and the axial skeleton and may cause enthesitis and peripheral joint inflammation. Extraarticular organ and peripheral joint involvement are markers of more severe AS. Although acute anterior uveitis is the most common extraarticular manifestation, occurring in 20% to 30% of cases, clinically significant cardiovascular involvement occurs in approximately 10% of patients with AS. The prevalence of AS is higher in males than females and the condition is more common in populations with a higher prevalence of HLA B27; that is, higher among Caucasians and Native Americans than African Americans and Asians.
A number of clinic-based studies have demonstrated increased mortality rates and excess CVD mortality in AS patients compared to the general population (57,58). Much of this excess CVD mortality was due to AS-specific cardiovascular complications (57).
Several characteristic cardiovascular lesions are described as being complications of AS. These include valvular heart disease, which occurs in approximately 10% of patients. However, the cardiovascular system may also be affected by the systemic inflammation associated with AS. Pericarditis is rarely seen in association with AS, although echocardiographic studies have revealed pericardial thickening and effusion in 5% of asymptomatic patients (59).
Valvular Involvement
Clinically significant aortic regurgitation occurs in approximately 2% to 10% of patients with AS. The prevalence of valve disease increases with longer disease duration and AS severity. Stenotic aortic valve lesions have not been described in association with AS. Inflammation of the ascending aorta
at the level of the sinuses of Valsalva causes distortion and dilatation of the aortic ring. Fibrotic thickening and downward retraction of the valve cusp bases with inward rolling of the edges of the valve cusps occur, and these factors contribute to the development of aortic incompetence (60). These “characteristic” pathologic findings have also been described in association with other seronegative spondarthropathies. Fibrosis may extend down from the nonseptal portion of the aorta to involve the mitral leaflet. This can occasionally give rise to mitral valve insufficiency. Mitral insufficiency may also develop secondary to left ventricular dilatation caused by aortic regurgitation. Asymptomatic mitral prolapse is observed in approximately 10% of patients with AS.
at the level of the sinuses of Valsalva causes distortion and dilatation of the aortic ring. Fibrotic thickening and downward retraction of the valve cusp bases with inward rolling of the edges of the valve cusps occur, and these factors contribute to the development of aortic incompetence (60). These “characteristic” pathologic findings have also been described in association with other seronegative spondarthropathies. Fibrosis may extend down from the nonseptal portion of the aorta to involve the mitral leaflet. This can occasionally give rise to mitral valve insufficiency. Mitral insufficiency may also develop secondary to left ventricular dilatation caused by aortic regurgitation. Asymptomatic mitral prolapse is observed in approximately 10% of patients with AS.
Arrhythmias
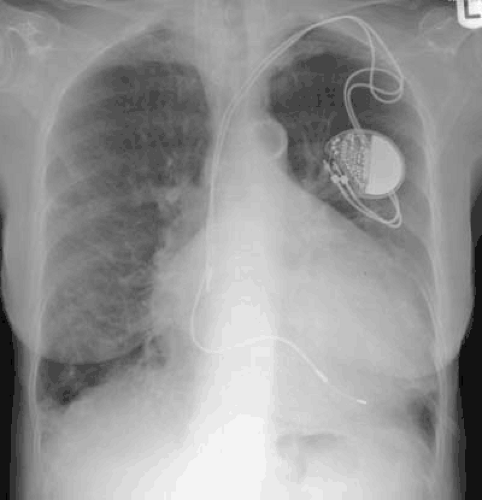
AV conduction blocks have been reported in association with AS and other spondarthropathies and are thought to represent the most common cardiac complication of AS. However, the prevalence of these conduction defects varies markedly between studies. One early study of 190 patients described first-degree AV block in 15% of AS patients whereas another study found ECG evidence of AV block in only 6% (61). It seems that HLA B27 related disease processes are more prevalent in cardiology patients requiring permanent pacemakers (62) and there is some evidence that AV block may occur intermittently in AS patients. This suggests that the conduction disturbance may be initially due to a reversible inflammatory process rather than disruption owing to fibrosis (60). Other arrhythmias include increased frequencies of both atrial and ventricular arrhythmias with evidence of prolonged QT dispersion being noted in nearly 60% of AS patients in one study (61). This suggests that the whole conducting system may be affected in AS and damage is not limited to AV nodal tissue.
Disturbance of the autonomic nervous system has been described in AS, with evidence of decreased parasympathetic activity (63). These findings were more marked in AS patients with active inflammatory disease and as similar findings have been observed in other systemic inflammatory conditions this disturbance of the autonomic nervous system may be related to systemic inflammation rather than specifically due to AS.
Myocardium
Although patients with known aortic valve insufficiency may develop ventricular failure as a secondary phenomenon, myocardial involvement in AS may also occur in the absence of aortic valve disease. Left ventricular dilatation and impaired diastolic function of the left ventricle have been described in association with AS (64) and diastolic ventricular dysfunction is observed even in patients with less severe AS disease.
Coronary Artery Disease
AS is not typically associated with accelerated atherosclerosis. One small study revealed ECG evidence of ischemic heart disease in 18% of AS patients (65). However, a study utilizing data from the UK General Practice Research Database did reveal that men with AS had a 40% increase in rates of first MI compared to men without AS (66). Rates of traditional CVD risk factors appear to be similar in AS patients (64), so it is possible that chronic inflammation associated with AS may promote accelerated atherosclerosis in this condition. NSAIDs are the main treatment for AS symptom control and many patients will have long-term exposure to these drugs. Therefore, these patients may be at increased risk of NSAID-associated cardiovascular side effects, including hypertension (67), and congestive cardiac failure given the association between AS and left ventricular dysfunction (68).
Cardiac Involvement in Gout
Gout is a common rheumatic disease with a prevalence of 2.8 to 8 per 1,000 population. It is more common in men and premenopausal women are usually spared. Its classical clinical presentation is with acute, exquisitely painful swelling affecting the first metatarsophalangeal joint, although other joints can be affected. Gout is a crystal arthropathy and demonstration of monosodium urate crystals in the joint fluid or soft tissues is required for a firm diagnosis.
Apart from rare case reports of valvular pathology owing to gouty tophi (69), there is little evidence of any other structural cardiac involvement that develops in association with gout. Hyperuricemia is the common metabolic abnormality that leads to the development of gout in some people and there is a substantial body of research that has linked hyperuricemia and gout with CVD. It is widely accepted that diuretic use and hypertension are both risk factors for developing gout (70). However, there are also data linking gout and hyperuricemia to an elevated risk of CVD (71,72). It is not clear in which direction the causal arrow should be drawn. Other factors including obesity, the metabolic syndrome, and renal impairment may also contribute to the development of both gout and coronary artery disease.
There has been growing interest in the link between uric acid levels, xanthine oxidoreductase, and CVD. Xanthine oxidoreductase exists in two forms, xanthine oxidase and xanthine dehydrogenase. Both of these enzymes are responsible for metabolizing uric acid from hypoxanthine and xanthine. Allopurinol, a drug commonly used to treat gout, lowers serum uric acid by inhibiting xanthine oxidoreductase.
Xanthine oxidoreductase is also an important source of reactive oxygen species in the cardiovascular system (73




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree