Figure 13.1
Right ventricular inflow view of a patient with Arrhythmogenic Right Ventricular Dysplasia. Note the right ventricular aneurysms (arrows). CS coronary sinus
Caused by progressive fibro-fatty replacement (dysplasia) of the RV myocardium.
LV may be occasionally involved, with relative sparing of the septum.
Patients may have ventricular arrhythmia of the left bundle branch morphology.
Familial linkage in approximately 30 % of patients (1st degree relative involvement).
Characteristics EKG finding is epsilon wave.
Morphologic features on imaging are hyperreflective moderator band, RV enlargement, RV dysfunction.
RV aneurysms are highly associated with this disorder and their presence portends a worse prognosis.
The presence of fat within the RV myocardium (as detected on MRI) is not a criterion required to satisfy the diagnosis.
Dilated Cardiomyopathy (Figs. 13.2 and 13.3)
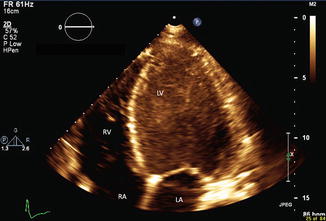
Figure 13.2
Apical four chamber view showing dilated cardiomyopathy. Note dilated and spherically shaped LV. Notice spontaneous echocardiographic contrast in the left ventricle consistent with low flow state
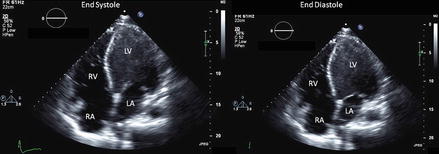
Figure 13.3
Apical four chamber view in systole and diastole showing poor ventricular function in patient with dilated cardiomyopathy
Characterized by dilation and reduced contractility of the LV or both the LV and RV.
End-diastolic and end-systolic dimensions and volumes are increased.
Systolic function indices such as ejection fraction, fractional shortening, systolic longitudinal motion of the mitral annulus, stroke volume, and cardiac output are diminished.
Wall thickness can be normal.
LV mass can be uniformly increased.
Secondary characteristics in this type of cardiomyopathy includes a dilated mitral annulus resulting in incomplete coaptation of the mitral valve leaflets and “functional” mitral regurgitation.
Other secondary features include low cardiac output, dilated atria, right ventricular dilation and associated left ventricular thrombus.
Interventricular conduction delay is common and results in intraventricular mechanical dyssynchrony.
First degree family members should undergo screening with echocardiogram or cardiac MRI due to the high incidence (20–50 %) of familial dilated cardiomyopathy [1].
PEARLS:
Pulmonary artery pressure estimated from the tricuspid regurgitation velocity is prognostics (velocity >3 m/s have a higher mortality).
Restrictive filling pattern (higher E/E’ ratio, low DT) is associated with high mortality and transplantation rate [2].
Mnemonic ABCCCDE for some causes of dilated cardiomyopathy: Alcohol, Beriberi (thiamine deficiency), Coxsackie, Chaga’s disease, Cocaine, Doxorubicin, Endocrine (hypothyroidism, thyrotoxicosis).
Hypertrophic Cardiomyopathy (Figs. 13.4, 13.5, and 13.6)
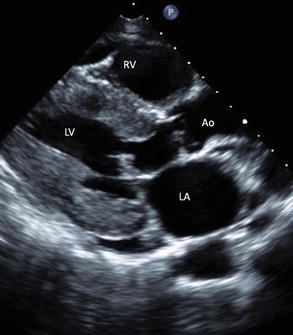
Figure 13.4
Parasternal long axis view of patient with hypertrophic cardiomyopathy (thickened septum and posterior walls). Please note the significant duration of SAM with LVOT obstruction with the M-mode in Fig. 13.5 (please note the anteriorly-directed motion of the anterior mitral leaflet towards the septum prior to LVOT obstruction [white arrow])
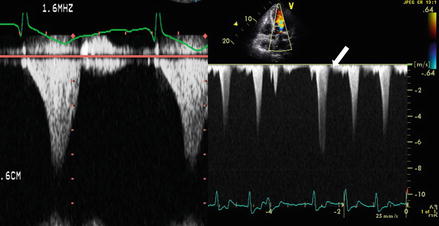
Figure 13.5
M-mode image showing dynamic LVOT obstruction (white arrow) in systole. Please notice duration of obstruction compared to the full cardiac cycle
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


