Figure 5.1
Calcified tricuspid aortic valve stenosis seen in long axis (left) and short axis (right); note significant leaflet calcification restriction of motion (arrows). LA left atrium, LV left ventricle, RV right ventricle, Ao aorta, RA right atrium
2.
Calcific stenosis of congenitally abnormal valve – review of 932 excised aortic valves (in patients without concomitant mitral valve replacement or mitral stenosis) showed that 59 % of men and 46 % of women had bicuspid or unicuspid aortic valve [1]
Unicuspid aortic valve
Anatomy: One leaflet; acommissural (no commissure) or unicommissural-one commissure (Fig. 5.2a)
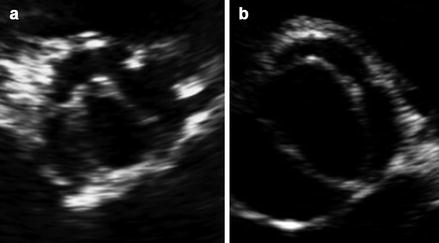
Figure 5.2
(a) Shows unicupsid aortic valve. (b) Shows bicuspid aortic valve with fusion of the right and left leaflets
Rare form of congenital aortic stenosis (0.02 % incidence)
3.
Rheumatic heart disease
Important etiology of aortic stenosis in developing countries
N.B. up to 80 % of patients with AS will also have AR
Interesting fact: First description and sketches of bicuspid aortic valve are attributed to Leonardo da Vinci [5]
Evaluation of Aortic Valve
Morphology of the valve
Aortic Stenosis velocity by continuous wave Doppler (note, the recorded velocity is at effective orifice area, not anatomic area) [6]. N.B. Measure maximal velocity at outer edge of dark signal
Mean and maximal transaortic gradient (do not forget that ΔP = 4 (V2max−V2proximal) for cases when proximal velocity is >1.5 m/s or aortic velocity is <1.5 m/s)
LVOT diameter – measure in mid systole (N.B. in many patients LVOT is elliptical and not circular leading to underestimation of AVA)
LVOT velocity by pulsed Doppler
N.B. pressure recovery has to be taken into account for aortic size <30 mm (pressure drop across the stenosis will be overestimated)
Low Flow Low Gradient Aortic Stenosis with decreased Ejection Fraction (present in 5–10 % of Severe AS patients) [9, 10]
LVEF < 40 %
Mean pressure gradient <30–40 mmHg
Effective orifice area <1.0 cm2
Possible situations: severe AS causing LV dysfunction limiting the ability to generate high transaortic valve gradients or patient with moderate AS and LV dysfunction from other etiology.
Dobutamine stress test:
Get images at rest, 2.5–5 μg/kg/min, 10 μg/kg/min, 20 μg/kg/min (increase dose every 3–5 min)
Record: LVOT diameter (at rest), AV VTI, LVOT VTI, AV mean pressure gradient, Aortic valve Vmax, Heart Rate
Stop when positive result is obtained or heart rate goes over 20 bpm over the baseline or exceeds 100 bpm, blood pressure drops, or when there are appearances of arrhythmias or symptoms.
Useful formulas:
Result interpretation [7]
Aortic Regurgitation
Etiology
Aortic Root Dilatation (Secondary)
Marfan’s syndrome
Idiopathic aortic dilation
Cystic medial necrosis
Senile aortic ectasia and dilation
Syphilitic aortitis
Giant cell arteritis
Takayasu’s arteritis
Ankylosing spondylitis
Valvular Abnormalities (Primary)
Rheumatic fever
Infective endocarditis
Collagen vascular diseases
Degenerative aortic valve disease
Bicuspid Aortic Valve
Unicuspid Aortic Valve
Quadricuspid Aortic Valve (Fig. 5.3)
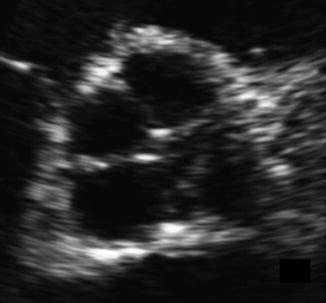
Figure 5.3
Quadricuspid aortic valve; all four leaflets best seen when valve is closed forming a characteristic cross sign
Evaluation
Aortic valve morphology
Aortic Root Morphology
Left Ventricle (dimensions and performance)
Aortic Flow
Left ventricular size and function
Flow in the aorta
Useful Formulas
Deceleration time:
Regurgitant Volume
Regurgitant Fraction
EROA
Mild | Moderate | Severe | |
|---|---|---|---|
Regurgitant Jet/LVOT Diameter | <0.25 | 0.25–0.45 mild-moderate 0.46–0.64 mod-severe | >0.65 |
Regurgitant Jet Area/LVOT Area (cross sectional area) | <0.05 | 0.05–0.2 mild-moderate 0.21–0.59 moderate to severe | ≥0.6 |
Regurgitant Volume (ml) | <30 | 30–44 mild-moderate 45–59 moderate to severe | ≥60 |
Regurgitant fraction | <30 % | 30–39 mild-moderate 40–49 moderate to severe | ≥50 % |
EROA (cm2) | <0.1 | 0.1–0.19 mild-moderate 0.2–0.29 mod-severe | ≥0.3 |
Vena Contracta (cm) | <0.3 | 0.3–0.6 | >0.6 |
Pressure Half-time (ms) (=0.29DT) | >500 | <200 | |
Decceleration rate (m/s2) | <2 | >3.5 | |
MV flow pattern | restrictive | ||
Aortic Doppler | Mild early diastolic reversal in descending aorta | Holodiastolic flow reversal in descending aorta | |
Doppler | Faint continuous Doppler sign | Dense continuous Doppler sign | |
LVEDD (mm) | <55 | >75 |
Mitral Valve Lesions
Mitral valve has such a name due to its resemblance to a mitre, a bishop’s headgear [14].
Mitral Stenosis
Etiology
Rheumatic Heart Disease (vast majority of cases)
Congenital mitral stenosis
Severe calcification of mitral annulus
Systemic lupus erythematosus (rare)
Fabry’s disease (rare)
Evaluation
Mitral valve morphology
Left Atrial size
Pulmonary Pressures
Rheumatic Mitral Stenosis (Fig. 5.4, Videos 5.5 and 5.6)
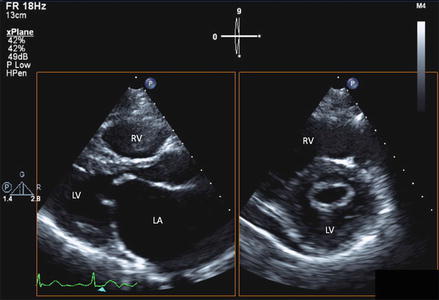
Figure 5.4
Parasternal long (left) and short axis (right) views showing rheumatic mitral stenosis. Note the hockey-stick appearance of the anterior leaflet (left image) consistent with rheumatic etiology of stenosis. Parasternal short axis view shows commissural fusion and “fish mouth” opening in rheumatic mitral stenosis. LA left atrium, LV left ventricle, RV right ventricle
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree