Cardiac Trauma
Samir R. Kapadia
Eric J. Topol
Overview
Among young people, trauma is the most common cause of death, with cardiovascular mortality being the major contributor. Patients with injury to the thorax, blunt or penetrating, should be transferred rapidly to a trauma center for fast and expert surgical evaluation. In unstable patients, echocardiography helps to identify critical injury and facilitates early surgical exploration, which can be lifesaving. In more stable patients, the goal of evaluation is to rule out significant occult cardiac and thoracic great vessel injury. Echocardiography, computed tomography (CT), thoracoscopy, and magnetic resonance imaging (MRI) can enable the clinician to make an accurate diagnosis of these injuries. Although a normal electrocardiogram (ECG) helps to identify low-risk patients with blunt cardiac injuries, the significance of an abnormal ECG and cardiac enzyme elevation in this setting remains unclear.
Trauma is a leading cause of death for young adults in the United States (1), with thoracic trauma accounting for 30% to 50% of 150,000 total deaths from trauma occurring annually (2,3,4,5). The heart and thoracic great vessels are commonly involved in blunt and penetrating trauma. Most serious injuries to these vital organs are rapidly fatal. Therefore, fast transport of these patients to trauma centers, rapid recognition of injury, and expeditious expert treatment are essential for better survival.
Injury to the Heart
Classification of Cardiac Injury
Physical trauma to the heart can be penetrating or blunt. A penetrating injury results when a foreign object enters the body and pierces the heart. Blunt injury, conversely, results from physical forces acting externally on the body. Iatrogenic injuries to the heart and great vessels from invasive procedures are not uncommon. Electrical and radiation injuries are other uncommon mechanisms of cardiovascular trauma.
Penetrating Cardiac Injury
Historical Perspective
Penetrating cardiac injury has been well recognized for centuries, with earliest descriptions by Homer in The Iliad (6). In 1761, Morgagni (7) noted that blood in the pericardial sac could lead to compression of the heart. Fischer (8), in 1868, reported pericardial drainage after injury in 452 cases, with 10% survival. Even in this era, however, there was serious skepticism about the therapy. One of the prominent surgeons of this time, Billroth, stated the following: “The surgeon who should attempt to suture a wound of heart would lose respect of his colleagues” and “Let no man dare to operate on the heart” (9,10). In 1896, Cappelen performed the first repair of a human left ventricle and left anterior descending artery, but the patient did not survive. Rehn (11), at about the same time, is credited with the first right ventricular repair in which the patient survived. In 1902, Hill (12) became the first American surgeon to suture a myocardial injury, in a 13-year-old boy, by the flickering lights of kerosene lamps on a kitchen table.
Anatomic Considerations
The classic precordium is defined as an area of chest bounded by the sternal notch superiorly, the xiphoid process inferiorly, and the nipples laterally. Most stab wounds injuring the heart enter through the classic precordium. Most gunshot wounds strike the heart without entering this zone. The relative frequency of cardiac chamber involvement depends on the anatomic location of the chamber as well as the type of penetration. The right ventricle, with its maximum anterior exposure, is at the greatest risk for injury. In a series of penetrating wounds to the heart, the right ventricle was involved in 42%, the left ventricle in 33%, the left atrium in 6%, and the right atrium in 15% (13). Pericardial reflections are important to recognize because they are positioned on portions of the ascending aorta, the main pulmonary artery, portions of the right and left pulmonary arteries, portions of the pulmonary veins, and portions of the superior and inferior vena cava. This is important because even trivial injuries to the intrapericardial portions of these vessels can result in cardiac tamponade.
Etiology
Penetrating wounds to the heart commonly result from puncture wounds, knife wounds, and gunshot wounds (14). Puncture wounds are caused by ice picks, needles, or pellets from an air gun or a distant shotgun, typically involving a single chamber. Knife injuries also frequently involve a single chamber, producing a slitlike defect. Small-caliber gunshot wounds can cause multiple-chamber perforations along with injuries to the great vessels. In contrast, large-caliber gunshot wounds result in fatal gaping cardiac defects.
Pathophysiology
The size of pericardial defect and the severity of cardiac injury determine the clinical presentation and subsequent outcome. If the defect in the pericardium is small, a blood clot may seal this defect. If the bleeding from the heart or proximal vessels continues in the closed pericardial sac, intrapericardial pressure rapidly increases. Rapid accumulation of blood, even when small (about 100 mL), leads to a sufficient rise in intrapericardial pressure to cause tamponade. Conversely, if the defect in the pericardium is large, rapid exsanguination and death will occur. The number of cardiac structures involved determines the severity of cardiac injury. Multiple-chamber injury is usually fatal. Involvement of one or more cardiac valves with damage to the leaflets, annulus, chordae, or papillary muscle can lead to hemodynamic compromise (15). Conduction system damage (16) and coronary artery injury, although less common than in blunt trauma, have been reported with penetrating injury (17).
Clinical Profile
Patients presenting to the emergency room (ER) with penetrating cardiac injury may be dead on arrival, alive but hemodynamically compromised, or hemodynamically stable. A few patients who are dead on arrival can be revived with resuscitative thoracotomy in the ER. Identifying this small subgroup of patients is important to conserve resources because the yield of indiscriminate resuscitative thoracotomy is very low (<5%). Patients who show some signs of life on transport have up to a 30% chance of successful resuscitation (18). Patients with stab wounds compared with gunshot wounds and patients presenting with cardiac tamponade have a better chance of survival. In the second group of patients with hemodynamic compromise, it is important to recognize cardiac tamponade. Dyspnea, diaphoresis, agitation, confusion, apathy, or a feeling of strangling oppression should alert the physician to look for cardiac tamponade (19). Only 10% to 40% of trauma victims with tamponade present with the Beck triad of hypotension, jugular distention, and muffled heart sounds (20,21,22). Neck vein distention may be absent because of accompanying hypovolemia. Pulsus paradoxus is neither sensitive nor specific for tamponade in this situation.
The third, more stable group should be examined in detail after primary assessment of airway, breathing, and circulation. The entry site is especially important with stab wounds. An entrance wound high on the right side is likely to involve the aorta and right atrium. Lower right and left parasternal wounds involve the right ventricle, whereas inferolateral left parasternal wounds typically signify left ventricle involvement (23). In a gunshot wound, the entry site may be deceptive. If the entry site involves the “danger zone” of Suer and Mordax, which includes the precordium, epigastrium, and superior mediastinum, cardiac injury is typically present (13). The trajectory of the gunshot should also be determined. If the trajectory suggests juxtacardiac passage, the physician should keep a high index of suspicion for cardiac injury.
Management
Rapid transport of the patient to the trauma center is essential for better outcome. The so-called scoop and run policy, without an attempt to stabilize the patient in the field, is the best approach (24). Even roadside thoracotomy done by medical teams flown to the scene is without benefit (25). Intubation is beneficial for patients with cardiac arrest or hemodynamic instability (26,27). Closed chest cardiopulmonary resuscitation (CPR) is not only ineffective but also contraindicated if an impaling weapon is present. An intravenous line can be started en route to the hospital, although the role of intravenous fluids is controversial (28,29).
For patients who are dead on arrival, diagnostic and therapeutic endeavor consists of an ER thoracotomy with a goal to relieve tamponade, control hemorrhage, and restore cardiac function (27,30,31). After resuscitation, the patient should be rapidly transferred to the operating room for definitive surgery.
In patients with hemodynamic compromise, rapid operating room thoracotomy by a cardiothoracic trauma surgeon appears to be the most effective procedure. The role of ER thoracotomy has been a constant source of debate, but it should be restricted to patients who arrive in a moribund state or who rapidly deteriorate after arrival (32,33,34,35). ER thoracotomy with the use of staples to control cardiac bleeding and to minimize the risk of personal contamination from a needle stick remains controversial (36). Staples to the heart can enlarge the wound and at times are difficult to remove during definitive surgery. Definitive surgical treatment is detailed elsewhere, but the general principles are as follows (4,37,38). Myocardial rupture is repaired in all cases. In patients with distal coronary artery injury, ligation is sufficient. Definitive valve or shunt surgery is usually deferred until later. Approach to a foreign body is variable, but most commonly only those objects projecting into cavities or involving the left ventricle are removed.
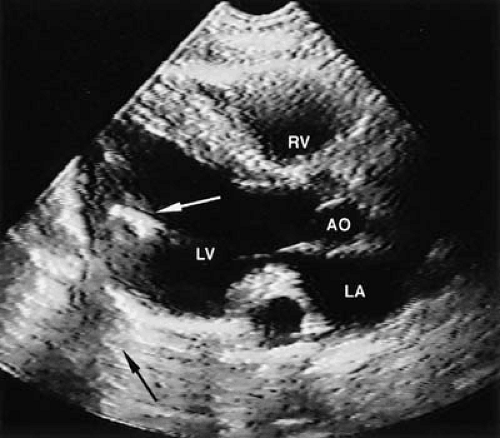
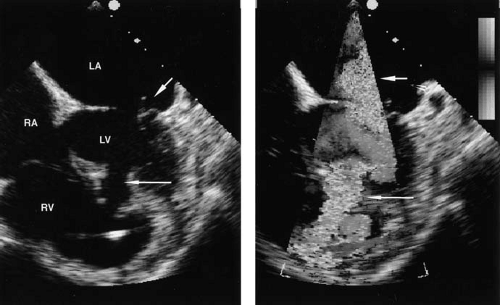
In hemodynamically stable patients or those stabilized with volume, transthoracic echocardiography (TTE) should be performed rapidly to diagnose pericardial effusion (PE). PE, however small, serves as a marker for cardiac penetration (39). When compared prospectively with a surgical gold standard (subxiphoid window), echocardiography has high specificity and sensitivity in diagnosing PE (40). It has rapidly become a modality of choice to assess patients with thoracic trauma (41). However, in the presence of hemothorax, its sensitivity is significantly decreased (42). Transesophageal echocardiography (TEE) can overcome this limitation of TTE, but in many patients it either is not feasible because of other injuries or is not expeditiously available and hence is of limited usefulness (43,44,45,46). Subxiphoid pericardial window was the traditional way to rule out PE in patients with suspected penetrating wound to the heart. It is best performed in the operating room with the patient under light general anesthesia. Although it is a safe procedure and provides a definitive diagnosis of hemopericardium (47,48,49,50), it typically results in a negative exploration rate of 75% to 80% (49). The availability of TTE in the ER has significantly reduced the frequency of this operation, which is now used only in few difficult situations to complement echocardiography (51,52,53). Thoracoscopic pericardial window is another alternative that has been shown to be safe and effective in diagnosing cardiac injury (54). However, echocardiography has other advantages in that it is a reliable tool to localize foreign bodies (55,56,57,58) (Fig. 38.1) and helps in diagnosing and monitoring structural abnormalities such as valvular regurgitations and shunts (59,60) (Figs. 38.2 and 38.3). Therefore, the availability of TTE in the ER is shown to decrease time to definitive therapy, thus leading to a better outcome (61,62).
Importantly, the ECG is not helpful in evaluating penetrating injury. It inconsistently shows the injury pattern and, if negative, does not rule out significant injury (49). The chest radiograph may help by identifying patients with hemothorax who are difficult to image with ultrasound. However, other findings, such as an enlarged cardiac shadow or pneumopericardium, are infrequently present (20). Pericardiocentesis is not indicated for diagnosis in stable patients and can actually be harmful (63).
Prognosis
Various indices to categorize patients with penetrating cardiac trauma are available. Trauma indices describing anatomic
severity, such as American Association for the Surgery of Trauma (AAST) Organ Injury Scaling (OIS), Heart Injury Scale, Penetrating Cardiac Trauma Index (PCTI), Penetrating Thoracic Trauma Index (PTTI), Penetrating Trauma Index (PTI), Cardiovascular-Respiratory Score (CVRS) component of Trauma Score, and Injury Severity Score (ISS), are good predictors of outcome. However, the general condition of the patient plays a significant role in determining the prognosis of cardiac trauma. For this reason, a general condition index such as the Physiologic Index (PI) can be combined with anatomic indices to categorize a patient more accurately.
severity, such as American Association for the Surgery of Trauma (AAST) Organ Injury Scaling (OIS), Heart Injury Scale, Penetrating Cardiac Trauma Index (PCTI), Penetrating Thoracic Trauma Index (PTTI), Penetrating Trauma Index (PTI), Cardiovascular-Respiratory Score (CVRS) component of Trauma Score, and Injury Severity Score (ISS), are good predictors of outcome. However, the general condition of the patient plays a significant role in determining the prognosis of cardiac trauma. For this reason, a general condition index such as the Physiologic Index (PI) can be combined with anatomic indices to categorize a patient more accurately.
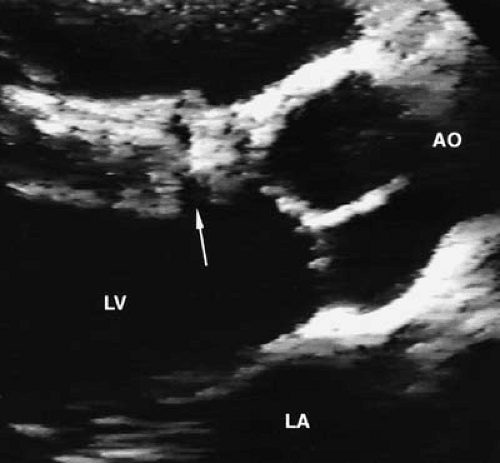
Patients who reach the operating room without requiring ER thoracotomy have a favorable outcome (64,65). Overall, patients with stab wounds have a better prognosis than those with gunshot wounds (35,66,67). Single-chamber injury to the heart with hemodynamic stability, shorter duration of CPR before arriving at the hospital, successful intubation, and younger age are all factors associated with better outcome (27,68,69). The presence of pericardial tamponade is thought to be a favorable predictor because it possibly prevents exsanguination (70). Late sequelae such as pseudoaneurysm, ventricular septal defect, valvular regurgitation, and constrictive pericarditis have been reported (66,71,72,73,74). Surveillance for these anatomic sequelae with echocardiography is recommended (16,60,75,76) (Fig. 38.4).
Blunt Cardiac Injury
In civilian life, the most common cause of blunt cardiac injury is a motor vehicular accident (MVA). Falls from heights, falling objects, direct trauma from assault, and blast injury are other less common causes. Injury patterns in MVAs are governed by the location of the victim in the vehicle and the direction of impact. In a front impact, abrupt deceleration against the steering wheel is the most common cause of cardiovascular trauma. Side impact generates a high shearing force, more commonly causing an aortic injury. Seat belts and airbags also play a major role in determining the injury patterns. For unrestrained drivers, each cardiac and aortic injury occurs in approximately 20% of cases (77). Even in restrained drivers, significant thoracic injuries can still occur from contact with the steering wheel
and from deceleration, but the number of deaths from thoracic injuries is significantly lower (78,79,80). The air bag has been associated with rupture of the right atrium (81).
and from deceleration, but the number of deaths from thoracic injuries is significantly lower (78,79,80). The air bag has been associated with rupture of the right atrium (81).
Myocardial Contusion
Historical Perspective
Myocardial contusion was first noted by Burch in 1676 in an 8-year-old boy. In 1859, Schnabel noted a hematoma with a right atrial tear in a 49-year-old man who died several hours after the blunt injury. In 1954, Burchell aptly observed “and always with heart contusion, arise both doubt and much confusion” (82). The confusion is still prevalent in literature because myocardial contusion is a pathologic diagnosis without an accurate clinical counterpart (83,84




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree