Chapter 34 Cardiac Pacing Modes and Terminology
Pacemakers have the capability of sensing intrinsic cardiac activity and responding to sensed events depending on the pacing mode. Cardiac pacing terminology has evolved as the devices have become more sophisticated. Pacemakers have different programmable rates, pacing modes, and timing cycles that allow them to function predictably and respond to different circumstances. Understanding of pacing terminology and timing cycles (Tables 34-1 and 34-2) is important to differentiate between appropriate and inappropriate pacemaker functions.
Table 34-1 Revised NASPE/BPEG Generic Code for Antibradycardia, Adaptive-Rate, and Multiple-Site Pacing
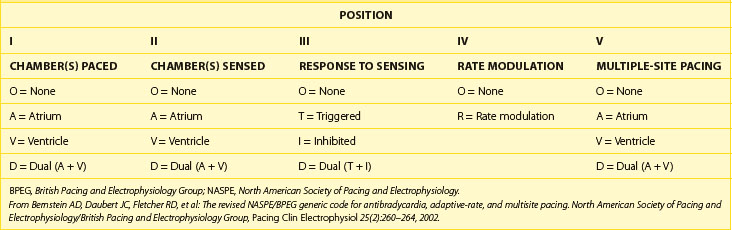
Table 34-2 Abbreviations and Description of Cardiac Events and Timing Cycles in Single-Chamber, Dual-Chamber, and Biventricular Pacemakers/Devices
| CARDIAC EVENTS/TIMING CYCLES (ABBREVIATION) | DESCRIPTION |
|---|---|
| SINGLE-CHAMBER (ATRIAL OR VENTRICULAR) PACEMAKER | |
| Atrial sensed event (P/AS) | Sensed a native Atrial depolarization (P wave) |
| Atrial paced event (A/AP) | Delivered Atrial Pacing output |
| Ventricular sensed event (R/VS) | Sensed a native Ventricular depolarization (QRS complex) |
| Ventricular paced event (V/VP) | Delivered Ventricular Pacing output |
| Atrial blanking period (AB) | Atrial sensing amplifier is “blind” and will not detect or respond to atrial sensed event |
| Ventricular blanking period (VB) | Ventricular sensing amplifier is “blind” and will not detect or respond to any ventricular sensed event |
| Atrial refractory period (ARP) | An atrial sensed event will be noted but ignored, without affecting pacemaker timing cycle |
| Ventricular refractory period (VRP) | A ventricular sensed event will be noted but ignored, without affecting pacemaker timing cycle |
| Lower rate limit (LRL) | Minimum pacing rate |
| Upper rate limit (URL) | Maximum pacing rate |
| Maximum sensor rate (MSR) | Maximum pacing rate by rate-responsive sensor |
| DUAL-CHAMBER (ATRIAL AND VENTRICULAR) PACEMAKER | |
| Atrioventricular sequential pacing (AV) | Atrial paced event followed by paced ventricular event |
| P-synchronous V-pacing (PV) | Atrial sensed event followed by paced ventricular event |
| VA Interval (VAI) | Interval from ventricular sensed or paced event to atrial paced event |
| AR (AP-AS) | Atrial paced event followed by ventricular sensed event |
| AV interval or delay (AVI) | Programmed atrioventricular pacing interval |
| Paced AV interval (Paced AVI) | AV interval/delay from atrial paced event (A) to ventricular paced event (V) |
| Sensed AV interval (Sensed AVI) | AV interval/delay from atrial sensed event (P) to ventricular paced event (V) |
| Maximum or upper tracking rate (MTR) | Maximum ventricular pacing rate allowed in response to high sensed atrial rates |
| Postatrial ventricular blanking period (PAVB) | Period when ventricular sensing is “OFF” after an atrial paced event |
| Post-ventricular atrial blanking period (PVAB) | Period when atrial sensing is “OFF” after a ventricular paced or sensed event |
| Post-ventricular atrial refractory period (PVARP) | Period after a ventricular event when the device can sense but not track an atrial event |
| Total atrial refractory period (TARP) | Sum of AVI and PVARP |
| Rate-responsive AV delay (RRAVD) | AV delay that adjusts by shortening as the rate increases. |
| CARDIAC RESYNCHRONIZATION THE RAPY/PACEMAKERS | |
| Biventricular pacing interval or LV offset (V–V) | Timing gap between RV and LV pacing |
| RV refractory period (RVRP) | An RV sensed event maybe noted but ignored, without affecting RV pacing timing cycle |
| LV refractory period (LVRP) | An LV sensed event maybe noted but ignored, without affecting LV pacing timing cycle |
| LV protection period (LVPP) | Period after a ventricular paced or sensed event that prevents inappropriate pacing during vulnerable period |
Pacing Nomenclature
A five-letter pacing mode nomenclature has been adopted (see Table 34-1).1 The first letter refers to the chamber being paced (Omitted or absent, Atrium, Ventricle, and Dual for atrium and ventricle), the second letter refers to the chamber being sensed (Omitted or absent, Atrium, Ventricle, and Dual for atrium and ventricle), and the third letter refers to the response of the pacemaker to a sensed event (Omitted or absent, Inhibit, Trigger or tracking, and Dual for inhibit and trigger). The fourth letter refers to the rate modulation or rate adaptive response to activity (Rate adaptive, and Omitted or absent rate response), and the fifth letter refers to multiple-site pacing (Omitted or absent, Atrium, Ventricle, and Dual for atrium and ventricle).
Pacing Modes
Available pacing modes depend on the location and number of leads implanted. Indications, advantages, and disadvantages of different pacing modes are reviewed in Table 34-3.
Table 34-3 Indications, Advantages, and Disadvantages of Commonly Used Pacing Modes
| PACING MODE | INDICATION/ADVANTAGES | DISADVANTAGES |
|---|---|---|
| Asynchronous (AOO, VOO, DOO) | Pacemaker-dependent patients exposed to noise (e.g., electrocautery during surgery) Avoids oversensing and asystole | Pacing regardless of intrinsic events Potential risk for arrhythmia induction |
| Single-chamber pacing (AAI, VVI) | AAI: sick sinus syndrome with intact AV node; preserves AV synchrony VVI: atrial fibrillation with slow VR and single-lead ICDs AAI/VVI require a single lead and increase battery longevity | AAI lacks ventricular pacing in the event of intermittent AV block VVI is associated with AV dyssynchrony (manifest as pacemaker syndrome) VVI has a higher incidence of atrial arrhythmias10 |
| DDD, DDDRV (CRT) | Preserves AV synchrony (less pacemaker syndrome) Low incidence of atrial arrhythmias and improved hemodynamics | Requires at least a two-chamber lead system and has less battery longevity |
| DDI | Functions as two different pacemakers (AAI and VVI) Used as mode switch to avoid tracking atrial tachyarrhythmias | Same as DDD: possible AV dyssynchrony and pacemaker syndrome (does not track atrial sensed events)2,9 |
| VDD | Appropriate sinus node function with AV node disease (e.g., MDT RV lead model 5038); dual chamber with high atrial pacing threshold to minimize battery depletion | Lack of atrial pacing Potential AV dyssynchrony at lower rate limit |
| DVI | Severe sinus bradycardia/standstill and atrial lead malfunction (oversensing) | Asynchronous atrial pacing Potential AV dyssynchrony |
AV, Atrioventricular; VR, ventricular regurgitation; ICDs, implantable-cardioverter-defibrillators; MDT, Medtronic, Inc.; RV, right ventricular.
Single-Chamber or Dual-Chamber Asynchronous Pacing
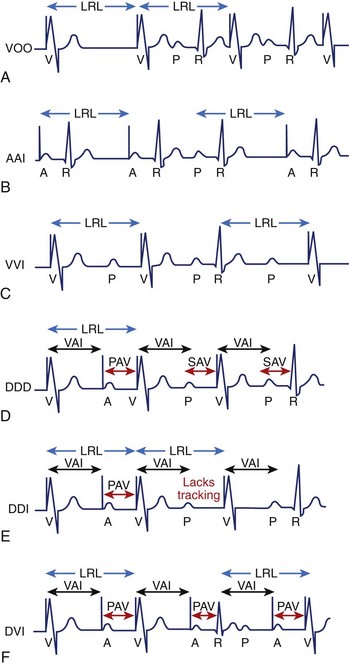
Asynchronous pacing refers to continuous atrial pacing, ventricular pacing, or both at a specific rate, regardless of the presence or absence of an intrinsic atrial event, ventricular event, or both (Figure 34-1, A). Such pacing mode is symbolized as AOO, VOO, or DOO. These pacing modes are used in limited circumstances, such as when pacemaker-dependent patients (without ventricular sensed events) are exposed to noise or artifact (e.g., electrocautery), which could result in asystole due to oversensing and pacing inhibition if the pacemaker has been programmed in a non-asynchronous pacing mode. Nevertheless, asynchronous pacing is often seen when the device is at the end of its life or when a magnet is placed over the pulse generator.
Single-Chamber (Atrial or Ventricular) Inhibited Pacing
Pacemakers with an atrial lead can be programmed to an atrial-inhibited mode referred to as AAI, whereas devices with a ventricular lead can be programmed to a ventricular-inhibited mode (VVI). The AAI pacing mode refers to atrial paced, atrial sensed, and inhibition of pacing output in response to an atrial sensed event (P wave), whereas the VVI pacing mode refers to ventricular paced, ventricular sensed, and inhibition of pacing output in response to a ventricular sensed event (R wave). Therefore the single chamber (atrium or ventricle) will only be paced if no sensed event (P wave or R wave) is detected faster than the programmed lower rate limit (LRL). In contrast, the single chamber (atrium or ventricle) will not be paced if a sensed event is detected (inhibited pacing) at a rate faster than the LRL (Figure 34-1, B and C).
Dual-Chamber (Atrioventricular) Sensing and Sequential, P-Synchronous Pacing with Inhibition (DDD)
The DDD pacing mode requires at least an atrial lead and a ventricular lead. The DDD mode refers to atrial and ventricular pacing as well as atrial and ventricular sensing with dual function (inhibit and trigger pacing) in response to an intrinsic atrial sensed event or a ventricular sensed event. In the DDD mode, the pacemaker will pace both the atrium and the ventricle (atrioventricular [AV] sequential pacing), with programmed AV delay if the intrinsic atrial and ventricular rates are below the LRL. If the atrial rate is slower than LRL, the device will pace the atrium while inhibiting ventricular pacing if an intrinsic ventricular event is sensed within a predetermined AV delay. If an atrial sensed event is faster than the LRL without an intrinsic ventricular event, the pacemaker inhibits atrial pacing but triggers ventricular pacing (P-synchronous pacing) after a predetermined AV delay (Figure 34-1, D). Finally, pacing will be completely inhibited if the intrinsic atrial and ventricular rates are above the LRL. This pacing mode is the most commonly used in dual-chamber devices (DDD or DDDR) and biventricular pacemakers (DDDOV or DDDRV).
Dual-Chamber (Atrioventricular) Sensing and Sequential, Non–P-Synchronous Pacing with Inhibition (DDI)
The DDI pacing mode refers to pacing both the atrium and the ventricle, sensing both the atrium and the ventricle and inhibiting pacing in response to an intrinsic atrial sensed event or a ventricular sensed event. In contrast to DDD, the DDI mode lacks the trigger or P-synchronous pacing in response to an atrial sensed event. Thus the pacemaker will not trigger ventricular pacing after an atrial sensed event, but atrioventricular sequential pacing will occur only after atrial pacing if no intrinsic ventricular event is present (Figure 34-1, E). The overall advantage is that it can function as two different atrial and ventricular pacemakers (AAI with a backup VVI). For example, in a patient with a high-degree AV block, a sinus rate of 80 beats/min, and a programmed LRL of 60 beats/min, the pacemaker will inhibit atrial pacing, but it will pace the ventricle at LRL with the development of AV dyssynchrony due to lack of the trigger or tracking feature. However, when the atrial rate drops below 60 beats/min, the pacemaker will pace both chambers at the LRL with preservation of AV synchrony.
Overall, the most commonly used pacing modes are VVI, DDD, and DDI without rate response or VVIR, DDDR, and DDIR with rate response. VDD and DVI are less commonly used pacing modes. The VDD mode refers to ventricular pacing only and atrial and ventricular sensing with inhibition and tracking function in response to a sensed event. This pacing mode is indicated in patients with normal sinus node function with AV nodal disease, as atrial pacing is not required. This dual-chamber pacing mode may be used with single-pass leads that incorporate both atrial and ventricular electrodes within a single lead body or in subjects with normal sinus node function and appropriate atrial sensing but a high atrial pacing threshold. DVI refers to atrial and ventricular pacing, ventricular sensing only, and inhibition to a ventricular sensed event. This mode lacks atrial sensing, and thus it will pace the atrium asynchronously at the LRL. This mode was used in first-generation pacemakers and thus is more of historical significance (Figure 34-1, F). However, DVI can still be used in patients with significant sinus bradycardia or atrial standstill and atrial lead malfunction (oversensing), in which atrial pacing is mandated (asynchronous pacing). Other pacing modes have a more historical use, such as VAT (ventricular pacing only, atrial sensing only, and tracking response), which could be used on pacemaker-dependent patients to avoid inhibition of ventricular pacing due to ventricular lead oversensing.2–4
Timing Cycles
Recognition of normal pacemaker function versus abnormal pacemaker function on the electrocardiogram (ECG) requires a clear understanding of pacemaker timing cycles. Overall, timing cycles are based on cardiac events such as atrial sensed events and ventricular sensed events (referred to as “P” and “R,” respectively), and atrial paced events or ventricular paced events (referred to as “A” and “V”, respectively). Appropriate sensing of cardiac events allows appropriate function and adaptation of the pacing mode, such as mode switching or noise reversion response (described below). Abbreviations and descriptions of pertinent cardiac events and pacemaker timing cycles are provided in Table 34-2.
Asynchronous pacing modes (AOO, VOO, and DOO) have the simplest timing cycle (they lack blanking and refractory periods) since there is neither sensing nor mode of response (see Figure 34-1, A). Thus, AOO or VOO have a fixed pacing interval, regardless of cardiac events, which depends on the programmable LRL. In addition, DOO has a programmable AV interval (AVI) as well as a ventriculoatrial (VA) interval that depend on the LRL. In contrast, non-asynchronous pacing modes have more timing cycles, including blanking and refractory periods.
Blanking and Refractory Periods
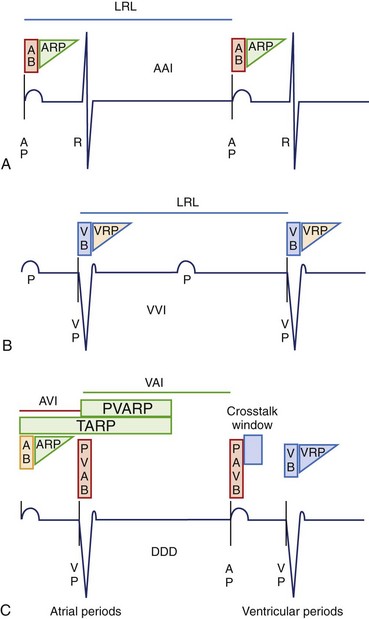
These are basic timing periods that avoid oversensing of inappropriate signals such as evoked potentials and repolarization. During the blanking period, the sense amplifier is “off” or “blind” and will not detect any event. Physiologically, this resembles the absolute refractory period during the cardiac action potential. The main purpose is to avoid cross-talk and oversensing related to evoked potentials. In contrast, the sensing amplifier is “on” during the refractory period and therefore allows detection of rapid signals or cardiac events. Physiologically, this corresponds to the relative refractory period of the cardiac action potential. Sensed events during this period are included in the counters but are ignored and generally do not trigger or reset timing cycles. The presence or absence of blanking and refractory periods depends on specific features of a manufacturer’s pulse generator as well as on the programmed pacing mode (Figure 34-2). Some blanking and refractory periods are not programmable.
Single-chamber pacing modes have simpler blanking and refractory periods. AAI would start an atrial blanking period (ABP) and an atrial refractory period (ARP) after an atrial sensed or atrial paced event, which would avoid oversensing atrial evoked potentials, atrial repolarization, or ventricular depolarization. Similarly, VVI would start a ventricular blanking period (VBP) and a ventricular refractory period (VRP) after a ventricular sensed or ventricular paced event to avoid oversensing of ventricular evoked potentials and T waves (Figure 34-2, A and B).
Conversely, dual-chamber pacing modes have more complex timing cycles (Figure 34-2, C). An atrial paced event starts a postatrial ventricular blanking (PAVB) to avoid ventricular oversensing during atrial pacing, whereas a ventricular paced or sensed event starts a PVAB to avoid atrial oversensing during ventricular pacing. If an atrial pacing artifact were to be detected on the ventricular channel, ventricular pacing would be inhibited (cross-talk), resulting in potential asystole in a pacemaker-dependent patient. Thus blanking periods are safety mechanisms that prevent cross-talk. Following the PAVB is a timing period called the ventricular triggering period or cross-talk sensing window, and in the event that a ventricular sensed event occurs during this period, safety pacing will take place. Safety pacing is a feature in which ventricular pacing occurs at an AVI typically shorter than the programmed AVI, often about 100 to 120 ms (programmable interval in some devices), to prevent ventricular asystole. Therefore, cross-talk should be suspected if AV pacing occurs at shorter than programmed AVI (Figure 34-3). Cross-talk can be resolved by extending the PAVB period, decreasing atrial output, or decreasing ventricular sensitivity.2–4
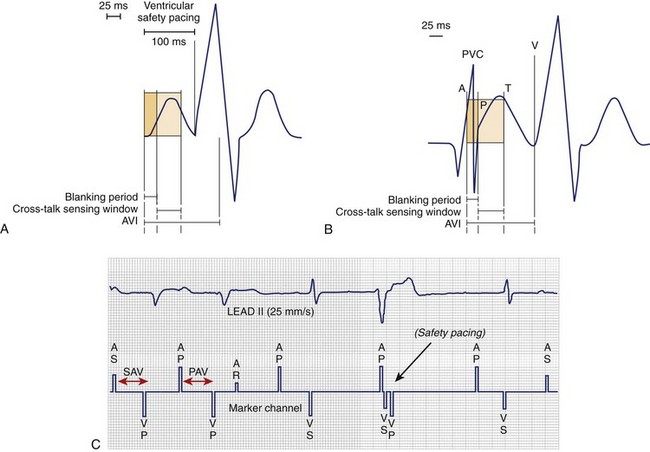
FIGURE 34-3 Blanking period, cross-talk sensing window, and safety pacing. A, Represents ventricular safety pacing at 100 ms when ventricular amplifier senses an event during cross-talk sensing window. B, Premature ventricular contraction (PVC) is not sensed, since it falls within postatrial ventricular blanking followed by ventricular pacing (VP) after completion of the atrioventricular interval (AVI).4 C, PVC occurs simultaneously as the lower rate limit times out and delivers an atrial paced event. Inappropriate safety pacing (100-ms AVI) occurs, since the PVC is sensed during the cross-talk window. PAV, Paced AV interval; SAV, sensed AV interval.
(A and B, From Ellenbogen KA, Wood MA: Cardiac pacing and ICDs, ed 4, Malden, MA, 2005, Blackwell.)
Furthermore, an atrial sensed event or an atrial paced event starts ARP and AVI. After the AVI is timed out, the pacemaker will deliver a ventricular paced event if no intrinsic ventricular sensed event is noted. A ventricular sensed event or a ventricular paced event starts VRP and postventricular atrial refractory period (PVARP). The VRP avoids sensing the evoked response and T wave, whereas PVARP avoids inappropriate atrial oversensing of ventricular repolarization, tracking of retrograde P wave, or both. The total atrial refractory period (TARP) is the sum of AVI and PVARP (see Figure 34-2, C). During TARP, any atrial sensed event noted does not affect the timing cycle. As a consequence, TARP limits the maximum tracking rate (MTR) in the DDD (P-synchronous) mode, as well as the upper rate limit (URL) or maximum sensor rate (MSR) in a non–P-synchronous mode and a rate-adaptive response, respectively. Thus, lengthening TARP will subsequently decrease the MTR, URL, or MSR. Atrial sensed events falling in TARP may not be tracked in a DDD pacing mode, but they will be detected and counted to detect higher atrial rates and trigger the mode-switch algorithm. PVARP should be extended to include a retrograde P wave only if VA conduction is present. Inappropriately short PVARPs can lead to a sensed retrograde P wave after a premature ventricular contraction (PVC), which will start an AVI followed by a ventricular paced event. This can set up a cycle of sensed retrograde P waves, causing an endless-loop pacemaker tachycardia, also called pacemaker-mediated tachycardia (PMT). PMT is a form of AV dyssynchrony or VA synchrony. PMT should be suspected when P-synchronous ventricular pacing is noted at the MTR with a sudden onset that occurs after PVC (Figure 34-4, A). Commonly, PMT may also be seen during atrial threshold testing, such as auto threshold, which causes a ventricular paced event after loss of atrial capture. This, in turn, leads to retrograde VA conduction with initiation of PMT if the atrial sensed event occurs beyond PVARP. More complex algorithms cause suspicion of PMT when the VP-P interval is stable, and they will confirm PMT if the measurement of the VP-P interval remains stable after alteration of the next P-V interval (Figure 34-4, B).5 However, if the VP-P interval lengthens or shortens after changing the P-V interval, the device excludes PMT and continues with P-synchronous tracking of the atrial rhythm. All device manufacturers have algorithms to interrupt suspected PMT. The most common algorithms include a withholding of a single ventricular pacing output, an extension of PVARP for a single cycle, and interruption of P-synchronous pacing after the AVI is met followed by sequential AV pacing (see Figure 34-4, B).5–7
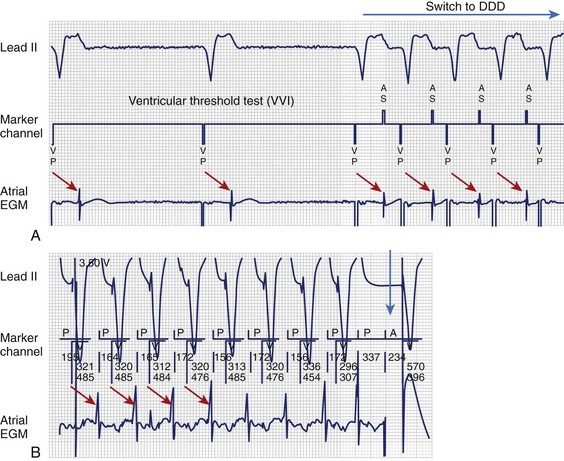
FIGURE 34-4 Pacemaker-mediated tachycardia (PMT). A, PMT initiated once the V-V interval (VVI) pacing mode switches to DDD during the ventricular pacing threshold. Red arrows illustrate VA timing from VP to atrial electrogram (EGM), which is only sensed and tracked after the device changes to the DDD mode. B, VP-P interval (red arrow) remains stable after changing the PV interval or sensed AV interval (P-synchronous pacing), which confirms retrograde VA conduction and PMT. Sequential atrial and ventricular pacing (blue arrow) is delivered to terminate PMT.4
(From Ellenbogen KA, Wood MA: Cardiac pacing and ICDs, ed 4, Malden, MA, 2005, Blackwell.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree