CHAPTER 84 Cardiac Devices for the Treatment of Bradyarrhythmias and Tachyarrhythmias
HISTORICAL PERSPECTIVE AND OVERVIEW
Paul Zoll developed the first transcutaneous electronic pacemaker in 1952 for the treatment of life-threatening bradycardia.1 The first internal pacemaker was implanted in 1958 for the treatment of complete heart block2 and in the management of Stokes-Adams seizures.3 Early pacemaker models were simple, fixed-rate devices. Thoracic surgeons performed the majority of early implants by placing epimyocardial leads directly on the exposed heart; these leads were connected to an abdominally implanted pulse generator. Modern pacemakers have sophisticated microprocessors that apply diagnostic and therapeutic algorithms, which have dramatically increased their versatility.
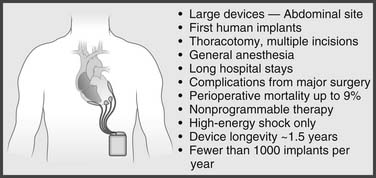
The development of the implantable cardioverter-defibrillator (ICD) was pioneered by Michel Mirowski.4–6 The initial purpose of the ICD was to provide immediate, automatic defibrillation to ambulatory patients who were victims of a lethal ventricular arrhythmia. Mirowski performed the first human ICD implantation in 1980.5 First-generation ICDs were composed of large generators (>200 cm3 volume) implanted in an abdominal pocket with epicardial defibrillator patches; these early ICDs were capable only of high-energy shocks. Current ICDs are small (<40 cm3 volume) but contain all the advanced pacing functions of modern pacemakers as well as complex tachycardia treatment options (Figs. 84-1 and 84-2). Despite their diminutive size, newer ICDs have become progressively superior in their sensing, detection, and treatment of arrhythmias. Since the late 1990s, ICDs have emerged as the single most effective lifesaving intervention in modern medicine.7–11
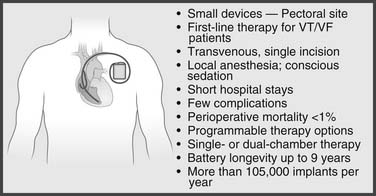
Figure 84–2 Implantable cardioverter-defibrillators today. VT/VF, ventricular tachycardia/ventricular flutter.
(Courtesy of Medtronic Inc.)
With increased sophistication and miniaturization of pulse generators and the development of the much simpler and safer transvenous approach for implantation of cardiac devices, indications for cardiac pacing as well as for ICDs have dramatically expanded.12,13 It is estimated that nearly 800,000 cardiac devices were implanted in North America in 2007 and more than 1,500,000 worldwide.14
INDICATIONS FOR IMPLANTATION OF CARDIAC DEVICES
The American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines for device-based therapy of cardiac rhythm abnormalities were updated in May 2008.13,15
Temporary Pacemakers
Indications
Placement of a temporary pacemaker is indicated whenever hemodynamic compromise is present because of a bradyarrhythmia. Temporary pacemakers should also be placed prophylactically if high risk for development of hemodynamically important bradycardia is present. Specific guidelines for placement of temporary pacemakers in the setting of acute myocardial infarction exist.16 Temporary transvenous pacing is indicated in symptomatic sinus bradycardia, sinus pauses of more than 3 seconds, or sinus bradycardia with a heart rate below 40 beats per minute associated with hypotension or hemodynamic compromise, if unresponsive to maximum doses (2 mg) of intravenous atropine. Other class I indications for temporary transvenous pacing in acute myocardial infarction include ventricular asystole, alternating left and right bundle branch block, and new bundle branch block or fascicular block and right bundle branch block in the setting of Möbitz II second-degree atrioventricular (AV) block.16
Venous Access
Table 84-1 summarizes the different sites that can be used for insertion of a temporary pacemaker.17 Careful consideration of the site to be used is important as it relates to the particular patient and advantages and disadvantages of each site. For instance, the internal jugular and subclavian veins may be chosen when need for stability and longer pacing requirement is anticipated. If a permanent pacemaker will be required in the future, the temporary pacemaker should be placed through a vein remote from the preferred site for permanent pacemaker implantation. Use of the antecubital veins minimizes bleeding in the coagulopathic patient. However, the risk of cardiac perforation or lead dislodgement is higher if the arm is not kept fully immobilized.
Table 84–1 Sites for Placement of a Temporary Pacemaker
| Site | Advantages | Disadvantages |
|---|---|---|
| Femoral vein | Easy access | Leg must remain immobilized |
| High infection risk | ||
| Fluoroscopy required for proper placement | ||
| Patient must lie flat | ||
| Internal jugular vein | Good site for pacer placement (right better than left) | Risk of pneumothorax, inadvertent carotid artery puncture |
| Patient must lie flat for access; Trendelenburg’s position preferred to avoid air embolism | ||
| Subclavian vein | Good site for pacer placement (left better than right) | Risk of pneumothorax, hemothorax with inadvertent subclavian artery puncture |
| Patient must lie flat for access; Trendelenburg’s position preferred to avoid air embolism | ||
| Antecubital vein (basilic, median basilic, or cephalic) | Access is low risk | Risk of dislodgement; arm must remain immobilized |
| Good site for pacer placement (left better than right) | Basilic or median basilic preferred (cephalic has tortuous course to central veins) | |
| Fluoroscopy required for pacer placement |
From Baim DS, Grossman W, editors. Grossman’s cardiac catheterization, angiography, and intervention. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2000.
Permanent Pacemakers
Indications
Symptoms from bradycardia generally result from inappropriate cardiac output. Such symptoms may be vague and include fatigue, decreased exercise tolerance, dyspnea on exertion, lightheadedness, dizziness, congestive heart failure, presyncope, and syncope. Patient-triggered ambulatory cardiac monitoring is often helpful in establishing that symptoms, which may be nonspecific, are in fact the result of symptomatic bradycardia. Boxes 84-1 through 84-12 summarize the indications for permanent cardiac pacing published by the American College of Cardiology/American Heart Association Task Force on Practice Guidelines in May 2008.13
Box 84–1 Recommendations for Permanent Pacing in Sinus Node Dysfunction
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class IIa
Class III
Box 84–2 Recommendations for Acquired Atrioventricular Block in Adults
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class IIa
Class IIb
Class III
Box 84–3 Recommendations for Permanent Pacing in Chronic Bifascicular Block
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class IIa
Class IIb
Box 84–4 Recommendations for Permanent Pacing after the Acute Phase of Myocardial Infarction
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class III
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Box 84–6 Recommendations for Pacing After Cardiac Transplantation
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Box 84–8 Recommendations for Pacing to Prevent Tachycardia
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Box 84–9 Recommendation for Pacing to Prevent Atrial Fibrillation
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Box 84–10 Recommendations for Cardiac Resynchronization Therapy in Patients with Severe Systolic Heart Failure
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class IIa
Class IIb
Box 84–11 Recommendations for Pacing in Patients with Hypertrophic Cadiomyopathy
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class IIb
From Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons.13
Class I
Class IIa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree