Cardiac Arrhythmias
To understand the disorders of heart rhythm, it’s essential to see them recorded in the electrocardiogram. Without this remarkable device, modern diagnosis and treatment of cardiac arrhythmias would be impossible.
Normal Sinus Rhythms
Logic will tell you what should appear in the ECG. Each impulse starts in the sinus node and travels across the atria, down the AV node, and through the ventricles, following the same track, moving at the same speed.
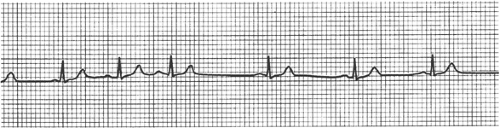
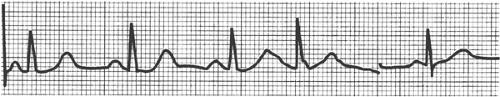
As a result, P waves will appear at regular intervals. Each P wave will be followed at identical intervals by QRS complexes and T waves. Every beat will look exactly like every other beat (Fig. 12-1).
Sinus Arrhythmia
Take your pulse by putting two fingers on your wrist, just below the thumb. When you feel the pulse, take a deep breath in and let it out. The pulse will probably speed up as you inhale and slow as you exhale. This is a normal phenomenon, caused by reflexes
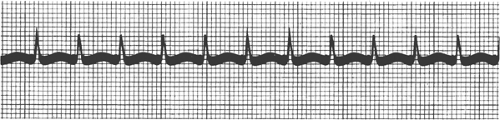
triggered by breathing. It can be quite pronounced, especially in young people. It should never be confused with a serious arrhythmia (Fig. 12-2).
triggered by breathing. It can be quite pronounced, especially in young people. It should never be confused with a serious arrhythmia (Fig. 12-2).
Ectopic Beats
The word ectopic means “outside the normal site.” An ectopic pregnancy, for example, arises outside the uterus.
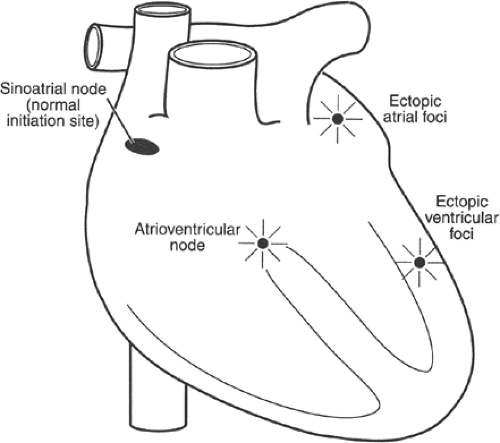
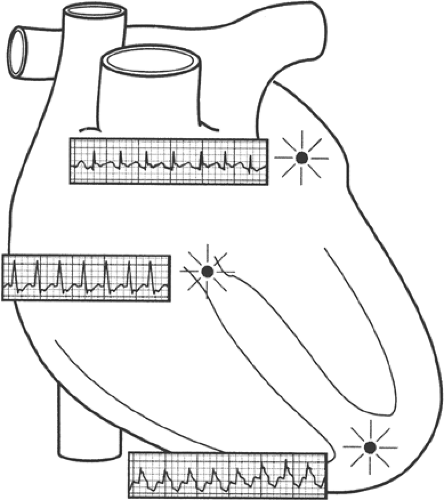
If the sinus node were the only pacemaker of the heart, higher life would have vanished from the earth a long time ago. The cells of the sinus node can become sick and may fail to fire, and if there were no other source of a heartbeat, life would end. Fortunately, there are hundreds of reserve pacemakers in the heart: tiny areas of tissue that can discharge a beat if needed. The heart is just like a car with 10 extra coils and 500 extra sparkplugs, organized in “fail-safe” systems. These ectopic pacemakers are scattered through the atria, the AV node, and the ventricles (Fig. 12-3).
Extrasystoles
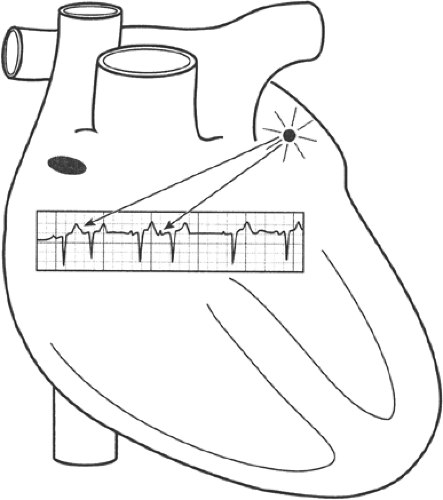
Everyone has them. You feel your heart “skip a beat”; there’s an odd pause and you wonder if your heart is going to start again. What happens is that one of the ectopic pacemakers becomes “irritable” and fires early, when it isn’t needed. The ectopic beat cuts into a normal sinus rhythm like this:
| beat beat beat beatBEAT beat |
The heart pauses after the early ectopic beat, and the next normal beat comes in where it would have if there had been a normal beat instead of the ectopic one—hence the pause (Fig. 12-4). It’s easy to detect an ectopic beat on the ECG. It’s also easy to tell exactly what part of the heart an ectopic beat comes from—that is, whether it comes from the atria, the AV node, or the ventricles. The pattern on the ECG is specific. Here are the rules:
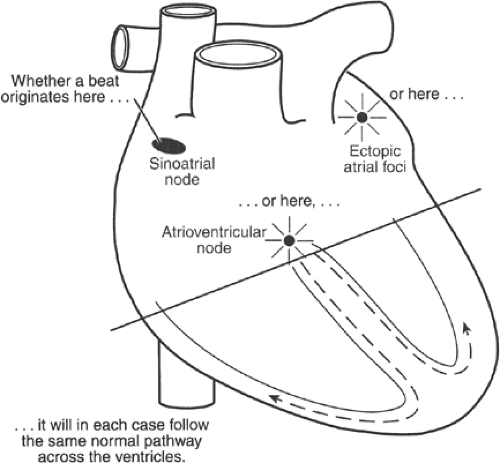
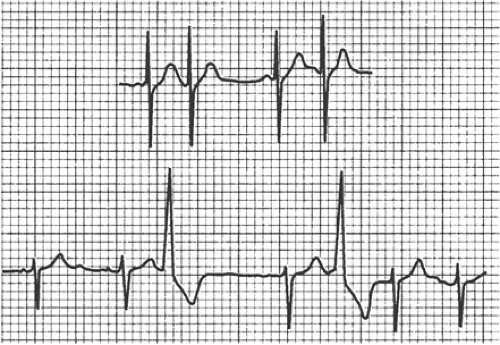
If an ectopic beat arises in the top half of the heart, it will follow the normal track down across the ventricles. In other words, the ventricular track of an ectopic beat arising in the top half of the heart will look exactly like the ventricular track of a normal sinus beat. Like the sinus beat, it will be narrow—less than 0.12 second—because the ectopic impulse is conducted along the “fast track” in the ventricles at 4 meters per second. Beats arising in the top half of the heart are called supraventricular beats because they arise above the ventricles (Fig. 12-5). Figures 12-6 and 12-7 illustrate the phenomenon of atrial ectopic beats.
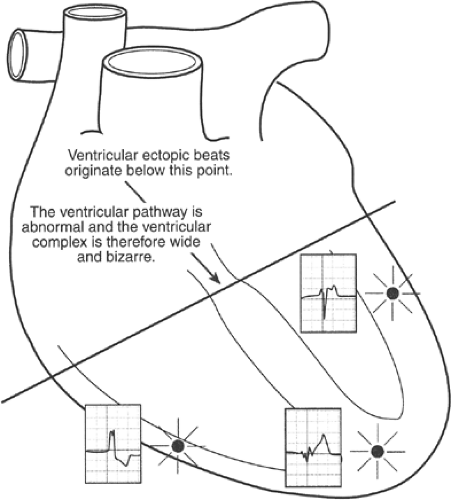
If an ectopic beat arises in the ventricles outside the normal conducting system, it has to move slowly because it’s outside the normal track, like a car on a muddy detour. The impulse moves directly through the muscle of the left ventricle at 0.5 meter per second, or about one eighth of normal speed. Since the impulse takes a long time to move across the ventricles, the track on the ECG will be wide; it will always include at least three time lines or 0.12 second, never less. Because the activating wave is following a winding, complicated, backward track across the ventricles, the shape of the QRS and T waves will be completely different from the shape of normal beats (Fig. 12-8). Figure 12-9 illustrates the obvious differences in electrocardiographic pattern between supraventricular and ventricular ectopic beats.
It’s often possible to tell whether ectopic beats arise in the atria or in the AV node, but that’s not important at this point. What is important is to know that:
There are ectopic beats.
They arise in all parts of the heart.
Beats from the top of the heart are narrow and those from the bottom are wide.
It’s also important to know that ectopic beats are a normal phenomenon. They feel strange, but they don’t mean anything and they very rarely need treatment.
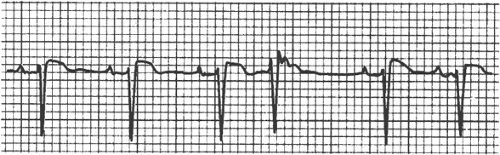 FIGURE 12-4 Normal sinus rhythm interrupted by an early beat (the fourth). This beat is caused by the premature discharge of an ectopic pacemaker. |
Paroxysmal Tachycardia
Sometimes an ectopic focus goes on firing, rapidly and regularly, for a long time—minutes, hours, or even days. (A paroxysm is something that starts and stops abruptly. Tachycardia means a rapid heart rate.) The change is like this:
| beat beat beat beat beatbeatbeatbeat |
and so on for some time. The rate may be as high as 260 to 270 beats per minute (bpm) or as low as 130 to 140 bpm. This kind of beating is called paroxysmal tachycardia.
Like ectopic beats, paroxysmal tachycardia can arise from the atria, the AV node, or the ventricles (Fig. 12-10). The most important thing to know about a paroxysm of tachycardia is which part of the heart it arises in. If it arises in the top half of the heart, it isn’t serious. Paroxysmal supraventricular tachycardia often appears in people with otherwise normal hearts, and it’s easy to treat.
If paroxysmal tachycardia arises in the ventricles, it’s always serious. Paroxysmal ventricular tachycardia almost always arises in damaged hearts, and it can threaten life. When it appears, a careful search should be made for some form of associated heart disease.
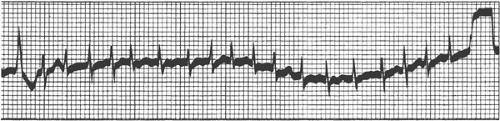
To make the distinction between the two types of paroxysmal tachycardia, you use the same trick you used in analyzing ectopic beats. If the ventricular complexes during a paroxysmal tachycardia are narrow, the tachycardia arises in the top half of the heart, and it’s the harmless variety (Fig. 12-11). If the ventricular complexes are wide, the tachycardia almost certainly arises in the ventricles, and it’s dangerous (Fig. 12-12). There are rare exceptions to this rule, but only a skilled electrocardiographer can make the distinction.
If you can count to three, you can tell the difference between supraventricular and ventricular tachycardia. The complexes of ventricular tachycardia will always be three squares wide (0.12 second); supraventricular tachycardia complexes will be less than three squares wide.
A patient will almost always feel some sensation when paroxysmal tachycardia starts—maybe a “pounding in the chest” or a “feeling as if the heart is running away.” If the tachycardia is ventricular, the patient may become dizzy or start to lose consciousness. It’s practically always possible to stop paroxysmal tachycardia with medicine, but there’s a caution. The right treatment for supraventricular tachycardia may be very wrong for ventricular tachycardia and may even kill the patient.
The only way to tell the difference between the two varieties is to record an electrocardiogram while the tachycardia is going on. “Blind” treatment without a precise
diagnosis may be useless or dangerous. The moral is obvious: it’s often possible to stop a paroxysmal tachycardia with medication. Adenosine, a drug that blocks the AV node for about 6 seconds, will almost always stop AV nodal reentrant tachycardia—which is the commonest type of supraventricular tachycardia. (Remember, the term supraventricular means “narrow beat tachycardia.”)
diagnosis may be useless or dangerous. The moral is obvious: it’s often possible to stop a paroxysmal tachycardia with medication. Adenosine, a drug that blocks the AV node for about 6 seconds, will almost always stop AV nodal reentrant tachycardia—which is the commonest type of supraventricular tachycardia. (Remember, the term supraventricular means “narrow beat tachycardia.”)
Drugs used now for ventricular tachycardia include the very safe, old reliable lidocaine or the newer and very powerful amiodarone.
If paroxysmal supraventricular tachycardia recurs, drug therapy with digitalis, beta blockers, or calcium blockers is often effective. If drugs don’t work, the patient should be sent to a good electrophysiology laboratory. (See the section later in this chapter called “Invasive Treatment of Arrhythmias.”)
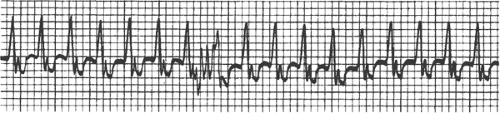 FIGURE 12-12 Paroxysmal tachycardia arising in the ventricles. The beats look like ventricular ectopic beats, which, of course, is what they are. |
Amiodarone is the only drug used today to prevent recurrence of ventricular arrhythmias: older drugs such as procaine amide and quinidine have fallen into disuse because of rare but dangerous complications. In fact, even amiodarone must be used with careful supervision because of toxic side effects.
Again, recurrent ventricular arrhythmias that resist drug therapy can be treated by invasive methods, but the results aren’t as good as with the supraventricular type.
Important Note: Supraventricular tachycardias don’t necessarily mean heart disease: they frequently occur in patients with otherwise normal hearts, and they never threaten life. Ventricular tachycardias of the common type almost always indicate heart disease and they indicate an urgent need for careful and thorough study.
If medicine doesn’t work, the tachycardia can be halted by a timed electric shock. Equipment to deliver this type of shock is available in every hospital and emergency room in the country and the technique is simple and safe.
Atrial Fibrillation
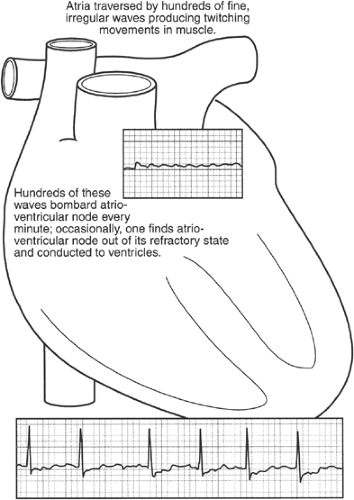
Imagine that you’re looking at a beating heart. The atria are contracting regularly, in rhythm with the ventricles. Now imagine that the atria stop their regular beat and begin a fine, fast twitching motion. This kind of abnormal motion is called fibrillation. The electrocardiogram records fine, fast, irregular waves—just what you’d expect (Fig. 12-13).
The electric waves from the atria are hitting the AV node very rapidly and irregularly, like a shower of sparks from a pinwheel. They hit the AV node about 425 times a minute. The AV node cannot possibly conduct that fast. The cells in the AV node perform actual work with each passage. This work leaves them tired, and they can’t conduct another impulse until they’ve had time to recover. This period is called the refractory period.
When fibrillating impulses are banging at the AV node 425 times a minute, many of these impulses will arrive when the cells are fatigued, or refractory from the previous passage, and the impulses won’t be conducted. Only those impulses that find the AV node cells ready to conduct will reach the ventricles, and this is a matter of pure chance. The ventricular rhythm will therefore be completely irregular. “Like ‘shave-and-a-haircut-six-bits’ repeated fast a lot of times” was the way one of my interns put it. Good description. Delirium cordis, or “delirium of the heart,” was the term physicians used a couple of hundred years ago to describe the fast, wildly irregular pulse (see Fig. 12-13).
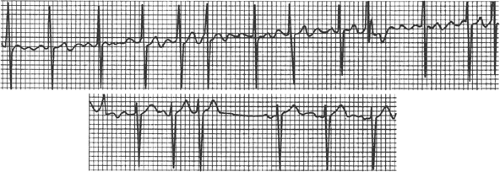
Atrial fibrillation is dangerous because it drives the ventricles too fast. They can’t pump efficiently. Imagine trying to squeeze water out of a bulb syringe. You could do pretty well squeezing 60 or 80 times a minute, but if you suddenly started twitching your hand a couple of hundred times a minute, you wouldn’t pump much water. The syringe would never have a chance to fill between beats. This is what happens with atrial fibrillation: the pumping action of the heart fails, blood backs up into the lungs, and congestive heart failure follows (Fig. 12-14).
The first step in treatment is to slow the heart rate by slowing conduction through the AV node. This is done with digitalis, the oldest known cardiac drug. Digitalis actually poisons the AV node so that it can’t conduct too fast. By giving the right dose, it’s possible to bring the ventricular rate down to normal and relieve the congestive heart failure.
Calcium-blocking drugs and beta-blocking drugs will also slow conduction through the AV node and are often used today. Both these drugs, however, can drop blood pressure, and beta blockers can depress ventricular function, so digitalis is preferable in the acute setting. For chronic control of rate with atrial fibrillation, it’s essential to combine digitalis with a calcium blocker or a beta blocker for one very practical reason: digitalis
will control the heart rate with atrial fibrillation when the patient is at rest but as soon as the patient begins to exercise, the digitalis effect is lost or diminished. This happens because exercise stimulates the sympathetic nervous system, whereas digitalis works by stimulating the opposing system (i.e., the parasympathetic nerves, chiefly the vagus).
will control the heart rate with atrial fibrillation when the patient is at rest but as soon as the patient begins to exercise, the digitalis effect is lost or diminished. This happens because exercise stimulates the sympathetic nervous system, whereas digitalis works by stimulating the opposing system (i.e., the parasympathetic nerves, chiefly the vagus).
There’s a debate going on today about the proper management of chronic atrial fibrillation.
There are two potential approaches:
Convert the patient to a normal sinus rhythm and attempt to maintain that rhythm with medication.
Simply control the rate with medication and give anticoagulants to prevent discharge of blood clots.
Some simple rules apply.
First, if the atrial fibrillation comes on suddenly with an obvious cause (overactive thyroid gland, congestive heart failure) it’s sensible to correct the cause and then try to restore a normal heart rhythm. Caution: If the atrial fibrillation has been going on more than 48 hours, anticoagulant therapy to suppress blood clots should be given for 3 weeks before any attempt is made to convert to a normal rhythm. If the atrial fibrillation has only been going on for a day or so, it’s reasonable to try to convert the heart to a normal rhythm as quickly as possible. Conversion to sinus rhythm can be achieved by drugs (see below) or by electroshock. (Atrial fibrillation produced by heavy drinking or what the British call “Monday morning heart” is a prime example of a condition calling for prompt cardioversion.)
Second, if atrial fibrillation is chronic and no specific cause can be detected, the best course at this time appears to be to let the patient go on fibrillating, control the rate to keep it within normal bounds, and administer anticoagulant therapy.
A number of drugs are available to convert to sinus rhythm and maintain it, but they all carry a certain risk. Sotalol, mexiletine, procainamide, disopyramide, flecainide, quinidine, and amiodarone all present a risk of about 1% per year of potentially catastrophic arrhythmia (torsade).
As an interesting note about physicians and medical fads, quinidine is one of the oldest cardiac drugs we have and it’s very effective early in atrial fibrillation. So is procainamide which is practically the same as quinidine in action and toxicity. These two drugs are much more effective in early cardioversion than the others listed. Amiodarone isn’t very effective at all in cardioverting to a sinus rhythm, although it’s useful in maintaining a sinus rhythm once it’s been established. Physicians, however, are swayed by drug company advertisements and whatever is new tends to be in vogue, like fashions, so quinidine and procainamide have fallen into disuse. The British and other Europeans, however, are now “rediscovering” quinidine, so the fad cycle may be expected to swing that way again (Fig. 12-15).
Causes of Atrial Fibrillation
The competent physician will always look for a cause and treat it. Overactivity of the thyroid gland can cause atrial fibrillation; so can stretching of the atria when diseased valves cause back pressure. When hypertension causes heart failure, the pressure in the atria will rise and this, again, can lead to fibrillation. When there is a specific cause, of course, it should always be corrected. Sometimes there is no cause that can be discovered; atrial fibrillation can appear in a heart that seems otherwise normal.
Blood Clots and Atrial Fibrillation
Whenever blood stagnates, it tends to clog—very much like gelatin hardening. In fibrillating atria, the blood isn’t being pumped cleanly and forcefully, and it tends to stagnate in the corners and recesses of the atria. Blood clots form. These clots are fragile: you could break them off by touching them. Pieces of these clots often do break off and float away in the bloodstream. They are dangerous—wherever clots lodge, they cut off the blood supply to the tissue downstream, and the tissue dies. If they lodge in the brain, clots cause a stroke. They can cause infarcts in the kidneys, the spleen, the adrenal glands, or, indeed, any organ of the body. Clots that lodge in the arms or legs can cause gangrene.
Anticoagulants, or drugs that keep blood from clotting, should be administered in practically all cases of atrial fibrillation. There’s been a great deal of study on the subject of which patients should be given anticoagulants and everyone’s now agreed on the guidelines.
First, when chronic atrial fibrillation is present, any patient with any kind of organic heart disease should be carried on Coumadin. “Heart disease” includes simple high blood pressure as well as coronary disease, valvular disease, diseases of heart muscle, and all forms of congenital disease except the type of atrial septal defect called ostium secundum (see Chap. 13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree