(1)
The Lindner Center for Research and Education The Christ Hospital, The Christ Hospital Physicians Ohio Heart and Vascular Center, Cincinnati, OH, USA
Keywords
Coronary calciumType Vb plaqueMESA studyMulti Ethnic Study of AtherosclerosisSt. Francis Heart StudyCalcium scoring techniqueQuantifying coronary calciumLesion ScoreVessel ScoreAgatston ScoreCalcium volumeCalcium massFramingham risk scorePROCAM scoreSCORESystemic Coronary Risk EvaluationCalcium scoreIntroduction
Coronary calcium is associated with abnormal coronary vascular function and with abnormal myocardial perfusion [1, 2]. In addition, the presence of coronary calcium portends a worse prognosis in the general population and in those that receive coronary revascularization [3, 4]. Similar mechanisms that influence bone formation and growth are responsible for the formation of coronary calcifications [5, 6]. That is, coronary calcification is an active and not passive process. There are two specific types of coronary calcification: atherosclerotic calcification and medial artery calcification. Atherosclerotic calcification mainly occurs in the intima and is caused by osteogenic differentiation of vascular smooth muscle cells induced by inflammatory mediators and elevated lipid content within the plaque [5]. Calcification in the media is associated with the elderly, diabetes and chronic kidney disease [6]. Medial calcification is also associated with decreased arterial compliance and worsened cardiovascular outcomes [2]. In other words, coronary calcification is not a part of the normal aging process and is wholly pathologic.
The amount of coronary calcification correlates with total coronary plaque burden where coronary calcium represents 20 % of the total coronary atherosclerotic plaque [7]. Furthermore, coronary calcium might promote plaque rupture but may also result from plaque healing [8–10]. Hypercalcemia and hyperphosphatemia promote the formation of coronary calcification by effecting the calcium and phosphate metabolism and by stimulating the transformation of vascular smooth muscle cells into osteoblasts [6, 11]. The ingestion of high levels of calcium has not been associated with coronary calcification [12].
Coronary artery calcification is associated with the process of atherosclerosis [13–15]. Calcified plaques are classified by the American Heart Association as type Vb [16]. While coronary calcification occurs in small amounts in early atherosclerotic plaques, it is more prevalent in advanced plaques and in older aged patients. There is only a weak correlation between the amount of plaque calcium and the degree of stenosis [16]. In fact, in cases of significant stenoses, the proportion of concentric, mixed or non calcified plaques were higher than those demonstrating eccentric and calcified plaques [17]. In addition, there is no known relationship between degree of coronary calcification and plaque rupture or vulnerability [18–20]. Furthermore, calcium does not deposit exclusively in areas of coronary plaque [21].
Calcification of the coronary arteries is more prevalent in men than women and is higher with advancing age [22]. Ethnic variation in the presence and amount of coronary calcification has also been demonstrated by the landmark MESA Study (The Multi-Ethnic Study of Atherosclerosis) [22, 23]. After adjusting for age, gender, lipids, education, body mass index, smoking, diabetes, hypertension, and statin therapy, whites had the most calcified coronary lesions followed by Hispanics, Chinese and then African Americans [22, 23]. The reasons for this finding are currently unknown.
Computed tomography (CT) is the only noninvasive imaging modality capable of accurately detecting and quantifying coronary calcium. In fact, the American College of Cardiology/American Heart Association Guidelines state that noninvasive coronary calcium scoring is “reasonable for cardiovascular risk assessment in asymptomatic patients at intermediate risk (10–20 % estimated 10 year coronary heart disease risk)” [24]. However, it should be recognized that the absence of calcium is not absolutely equivalent to the absence of coronary heart disease risk. Intermediate risk patients with calcium scores of 0 should still receive risk-reducing therapies as appropriately indicated by the National Cholesterol Education Program guidelines [24]. Calcium scoring has been deemed appropriate for intermediate risk patients and for low risk patients with a significant family history of premature coronary artery disease [25].
Technique
CT derived calcium scoring is an easy technique with relatively low radiation exposure. It is a noncontrast scan in which the power of the scanner is turned down to a minimum to reduce radiation exposure Unlike with contrasted cardiac CT angiography, nonoverlapping, thicker slices (2–3 mm) are used to further reduce radiation exposure. In addition, prospective triggering is always utilized to even further reduce the radiation dose. The total radiation dose is 1–2 mSv. While Electron Beam Computed Tomography was originally used for calcium scoring, multidetector CT is now the modality of choice. The exam is often performed prior to the contrasted scan but may also be performed individually and, alone, lasts only 5 min.
The landmarks for the scan field of view begin just above the carina and end just below the inferior portion of the heart (Fig. 6.1). Prospective imaging is used, where multiple axial slices are obtained during each beat without slice overlap (Fig. 6.2).
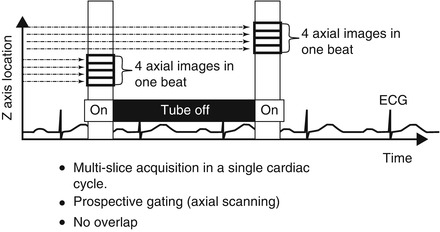
Figure 6.1
A computed tomographic scout image demonstrating the landmarks for the field of view for a calcium scoring scan
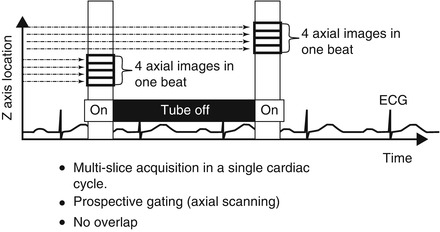
Figure 6.2
A cartoon depicting the scan protocol for a calcium score
Quantification
Coronary calcium is quantified using three methods. The first method called the Agatston score is the one that is used clinically. The second is measurement of the plaque volume and the third is measurement of the plaque mass. The Agatston score has the most robust set of data regarding prognosis and is the easiest to perform. Each lesion is given a score that equals the plaque area in pixels multiplied by a weighting factor. Lesion Score = Plaque area (pixel number) × weighting factor. The weighting factor is illustrated in Fig. 6.3 and is based on the Hounsfield unit of the calcium. Figure 6.4 demonstrates the practical calculation of a lesion score. Each lesion within a particular coronary artery is added to produce a vessel score. All vessel scores are summed to calculate the total Agatston score. The Agatston score is reproducible to ±15 %. This variance is related to the weighting score which is not linear but rather a step wise function. Thus, an insignificant difference in Hounsfield unit measurements may lead to a different weighting factor and thus, a significantly different Agatston score (Fig. 6.5).
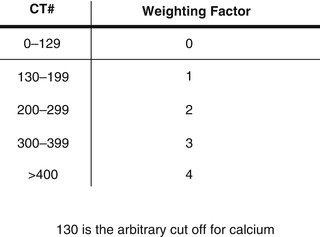
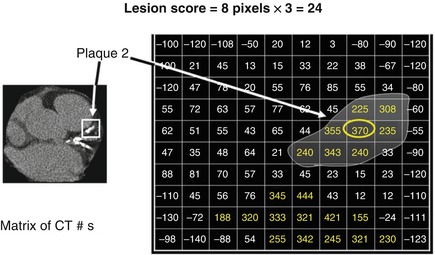
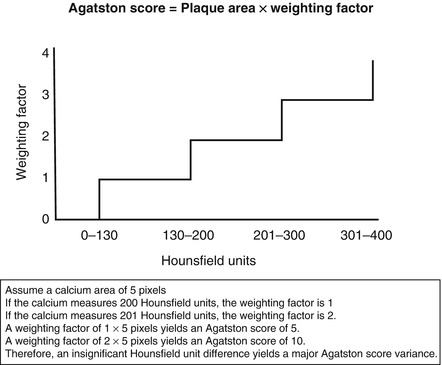
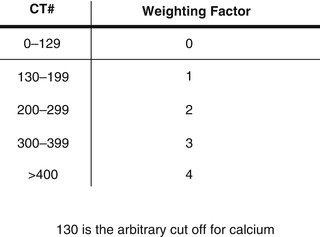
Figure 6.3
A graph depicting the weighting factors used to calculate an Agatston lesion score
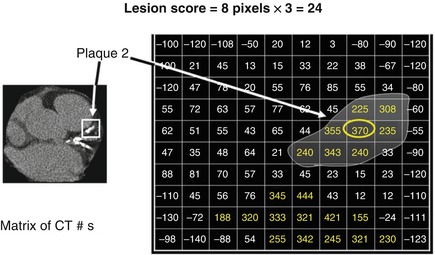
Figure 6.4
A cartoon depicting the calculation of a lesion score. In this example, there are 8 pixels in lesion 2 with a Hounsfield unit meeting the cut of for calcium (130). The highest Hounsfield unit within the lesion is 370 which corresponds to a weighting factor of 3. Lesion score = pixel number × weighting factor. Thus, 8 × 3 = 24. The lesion score is 24
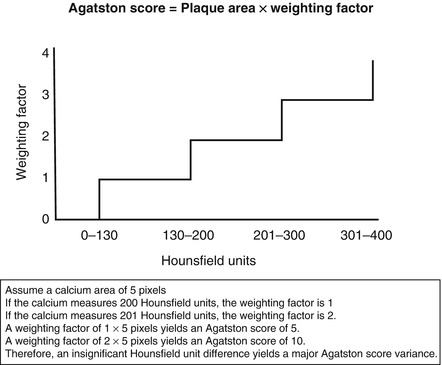
Figure 6.5
An illustration of the variance in Agatston score measurements
Plaque volume (Volume Score) is calculated by multiplying the number of pixels meeting the Hounsfield unit calcium threshold by the volume of a pixel (Fig. 6.6). The volume score is more reproducible than the Agatston score, but its accuracy is limited by the partial volume effect of calcium (blooming). Calcium mass, on the other hand, is very accurate and reproducible but has a small data base to validate its use. Furthermore, calcium mass is difficult to measure because it requires a phantom to be placed under the patient for scaling purposes. The calculation of the plaque mass is based on understanding the relationship between the CT number of the calcified plaque and it’s mass. It involves measuring a phantom that provides a calibration factor to convert calcium density to mass (milligrams, mg). Plaque Mass = Volume Score × Pixel Weighting (based on mg of calcium).
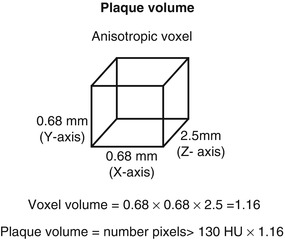
Figure 6.6
An illustration of the measuring of calcified plaque volume
Applications of Calcium Scoring
The two main applications of calcium scoring include risk assessment and prognosis and progression of disease.
Risk Assessment and Prognosis
Risk assessment is regarded as the first step in the clinical management of patients with cardiovascular risk factors. Traditionally, the Framingham Risk Score, the PROCAM score in Germany and the SCORE (Systemic Coronary Risk Evaluation) in Europe are most commonly used and most widely available. These risk assessment algorithms are often used to project short term and intermediate term risk, but not lifetime risk. In addition, these projections are used to determine appropriate candidates for risk reduction therapy. Treatment intensity is often linked to severity of risk. However, a significant accumulation of data support the premise that calcium scoring may further refine risk and reclassify those in the intermediate risk category into either low risk or high risk categories. In other words, calcium scoring has incremental prognostic value [26–32]. Shaw et al. [26] demonstrated that coronary calcium scores of over 1,000 posed a 12 times relative risk for all cause mortality versus traditional Framingham risk factors which posed a two times relative risk. This finding held true for both diabetics and non-diabetics. These findings have been confirmed by a multitude of studies including Budoff et al. [30] who observed a 10 year survival rate of 99.4 % in patients with a calcium score of 0 versus an 88.7 % survival rate for those with a score of > 100. The MESA (Multi Ethnic Study of Atherosclerosis) [32] was one of the latest land mark studies demonstrating the incremental risk prediction of coronary calcium. This study was a prospective study of 6,722 patients in six cities in the United States. The MESA study demonstrated a 3.5–10 times incremental risk of hard cardiovascular events based on coronary calcium burden, where those with a calcium score of >300 had a 10-fold higher risk compared to a 3.5-fold higher risk for a score of ≤100. In fact, the most recent guidelines for stable ischemic heart disease indicate that a calcium score of 100 portends a relatively low cardiovascular risk while that of >400 represents high risk (Fig. 6.7) [33].
Figure 6.7
All cause mortality in patients based on Framingham risk factors and coronary calcium (Adapted from Shaw et al. [26])
It has also been shown that coronary calcium scoring is able to more effectively and specifically classify patients into high or low risk groups than risk factor algorithms alone [32, 34–36]. Calcium scoring performs best when applied to the intermediate risk population and serves to reclassify these individuals into high or low risk strata. In other words, coronary calcium scoring places more patients in the most extreme risk categories than traditional risk factor based scoring systems alone. The yield of coronary calcium scoring in very low risk individuals is very low [37]. In addition, a subset of the MESA study proposes an arterial age calculator to assess the arterial age of a patient as related to their chronological age [38]. Furthermore, the degree of coronary calcification has also been shown to be predictive of the frequency and type of coronary revascularization [39]. The 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk indicate that a calcium score of ≥300 or ≥75th percentile support revising a patients cardiovascular risk upward from their pre-calcium score risk category [40].
While the absence of coronary calcium portends a favorable risk prediction [41–44], it does not preclude the presence of a clinically significant atherosclerotic plaque. The absence of coronary calcification does not absolutely exclude obstructive coronary disease or the need for revascularization [45]. Gottlieb et al. [45] demonstrated that 19 % of patients without detectable coronary calcium who were referred for conventional angiography had >50 % coronary stenoses. It should be noted that these patients prompted enough clinical suspicion to be referred for invasive coronary angiography in the first place. Sarwar et al. [42] demonstrated a negative predictive value for obstructive coronary stenoses of 93–98 % when no coronary calcium was detected. But the negative predictive value for obstructive coronary artery disease was not zero. Thus, while in the asymptomatic patient with a zero calcium score no further treatment is necessary, in the symptomatic patient with high clinical suspicion, the absence of coronary calcification should not discourage the clinician from more aggressive testing to exclude obstructive coronary artery disease. It should also be noted that calcium scoring is less predictive in those less than 45 years of age.
Disease Progression
Calcium scoring may be used to assess atherosclerotic disease progression over time. Progression of coronary calcification is often observed over periods of 3–7 years to a degree related to the extent and severity of the baseline coronary calcification [46, 47]. Progression of coronary calcification over time has been shown to portend a worse prognosis and predict future cardiac events [48–51]. The degree of baseline calcification and its progression have been associated with the greater prescription and adherence to aspirin and statin therapy and to better risk factor control without greater downstream medical testing [52–54]. However, serial coronary calcium scoring scans are not routinely recommended since improvement in outcomes based on such a practice has not yet been definitively established.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


