Chapter 20 Bradycardias and Tachycardias Review and Differential Diagnosis
Bradycardias (Bradyarrhythmias)
A number of arrhythmias and conduction disturbances associated with a slow heart rate have been described. The term bradycardia (or bradyarrhythmia) refers to arrhythmias and conduction abnormalities that produce a heart rate of less than 60 beats/min. Fortunately, the differential diagnosis of a slow pulse is relatively simple in that only a few causes must be considered. Bradyarrhythmias fall into five general classes (Box 20-1).
BOX 20-1 Bradycardias: Simplified Classification
Sinus Bradycardia and Related Rhythms
Sinus bradycardia is sinus rhythm with a rate less than 60 beats/min (Fig. 20-1). When 1:1 AV conduction is present, each QRS complex is preceded by a P wave; the P wave is negative in lead aVR and positive in lead II, indicating that the sinoatrial (SA) node is the pacemaker. Some individuals may have sinus bradycardia of 30 to 40 beats/min or less.
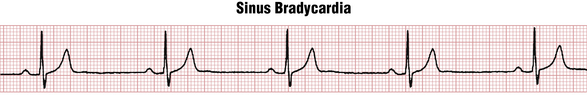
Figure 20-1 Marked sinus bradycardia at about 40/min. Sinus arrhythmia is also present. Sinus bradycardia (like sinus tachycardia) always needs to be interpreted in clinical context because it may be a normal variant (due to increased vagal tone in a resting athlete or in a healthy person during sleep) or may be due to drug effect/toxicity, sinus node dysfunction, etc., as discussed in Chapter 13. The PR interval here is also slightly prolonged (0.24 sec), also consistent with increased vagal tone or with certain drugs that depress activity in the SA and AV nodes (e.g., beta blockers).
Sinus bradycardia may be related to a decreased firing rate of the sinus node pacemaker cells or to actual SA block (see Chapter 13). The most extreme example of sinus node dysfunction is SA node arrest (see Chapters 13 and 19). Sinus bradycardia may also be associated with wandering atrial pacemaker (WAP).
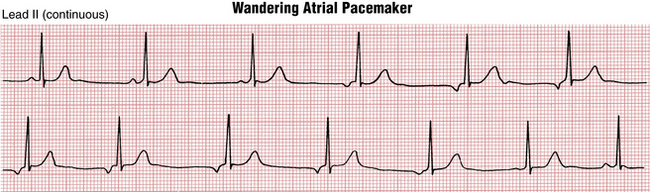
Wandering Atrial Pacemaker
Wandering atrial (supraventricular) pacemaker is an arrhythmia that is somewhat difficult to classify. As shown in Figure 20-2, this rhythm is characterized by multiple P waves of varying configuration with a relatively normal or slow heart rate. This pattern reflects shifting of the intrinsic pacemaker between the sinus node and different ectopic atrial sites, and sometimes the area around the AV junction (node).
Clinicians should be aware that WAP is quite distinct from multifocal atrial tachycardia (MAT), another arrhythmia with multiple different P waves. In WAP the rate is normal or slow. In MAT it is rapid. For rhythms that resemble MAT (see Chapter 14), but with rates between 60 to 100 beats/min, the more general term multifocal atrial rhythm can be used.
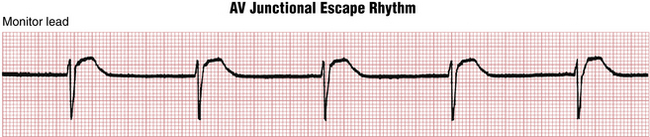
AV Junctional (Nodal) and Ectopic Atrial Rhythms
With a slow AV junctional escape rhythm (Fig. 20-3) either the P waves (seen immediately before or just after the QRS complexes) are retrograde (inverted in lead II and upright in lead aVR), or no P waves are apparent if the atria and ventricles are stimulated simultaneously. Slow heart rates may also be associated with ectopic atrial rhythms, including WAP (see previous discussion).
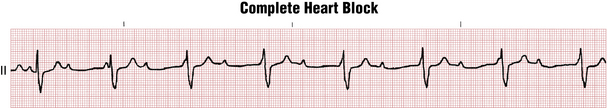
AV Heart Block (Second or Third Degree) or AV Dissociation
A slow ventricular rate of 60 beats/min or less (even as low as 20 beats/min) is the rule with complete heart block because of the slow intrinsic rate of the nodal (junctional) or idioventricular pacemaker (Fig. 20-4). In addition, patients with second-degree block (nodal or infranodal) often have a bradycardia because of the dropped (nonconducted) beats (see Chapter 17).
Isorhythmic AV dissociation and related arrhythmias, which may be confused with complete AV heart block, is also frequently associated with a heart rate of less than 60 beats/min (see Chapter 17).
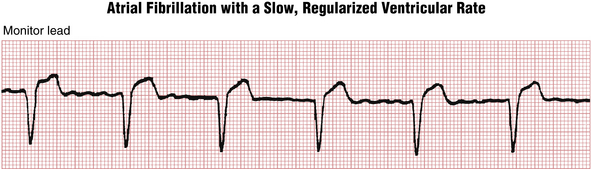
Atrial Fibrillation or Flutter with a Slow Ventricular Rate
Paroxysmal atrial fibrillation (AF), prior to treatment, is generally associated with a rapid ventricular rate. However, the rate may become excessively slow (less than 50 to 60 beats/min) because of drug effects or toxicity (e.g., beta blockers, calcium channel blockers, digoxin) or because of underlying disease of the AV junction (Fig. 20-5). In such cases the ECG shows the characteristic atrial fibrillatory (f) waves with a slow, sometimes regularized ventricular (QRS) rate. The f waves may be very fine and easily overlooked. A very slow, regularized ventricular response in AF suggests the presence of underlying complete AV heart block (see Chapters 15 and 17).
Idioventricular Escape Rhythm
When the SA nodal and AV junctional escape pacemakers fail to function, a very slow pacemaker in the ventricular conduction (His-Purkinje) system may take over. This rhythm is referred to as an idioventricular escape rhythm (see Fig. 13-10). The rate is usually very slow (often less than 45 beats/min), and the QRS complexes are wide without any preceding P waves. In such cases of “pure” idioventricular rhythm, hyperkalemia should always be excluded. In some cases of complete heart block, you may see sinus rhythm with an idioventricular escape rhythm, as described here. Idioventricular rhythm may be a terminal finding in irreversible cardiac arrest (also see Chapter 19).
Tachycardias (Tachyarrhythmias)
From a clinician’s perspective, the tachyarrhythmias can be most usefully divided into two general groups: those with a “narrow” (normal) QRS duration and those with a “wide” QRS duration (Table 20-1).
TABLE 20-1 Major Tachyarrhythmias: Simplified Classification
| Narrow QRS Complexes | Wide QRS Complexes |
|---|---|
| Sinus tachycardia | Ventricular tachycardia |
| Paroxysmal supraventricular tachycardias (PSVTs)∗ | Supraventricular tachycardia with aberration caused by a bundle branch block or Wolff-Parkinson-White preexcitation with (antegrade) conduction down the bypass tract |
| Atrial flutter | |
| Atrial fibrillation |
∗ The three most common types of PSVTs are AV nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT) involving a bypass tract, and atrial tachycardia (AT) including unifocal and multifocal atrial tachycardia, as discussed in Chapter 14. Other nonparoxysmal supraventricular tachycardias also may occur, including types of so-called incessant atrial, junctional, and bypass tract tachycardias. (For further details of this advanced topic, see selected references cited in the Bibliography.)
Narrow complex tachycardias are almost invariably supraventricular (i.e., the focus of stimulation is within or above the AV junction). Wide complex tachycardias, by contrast, are either ventricular or supraventricular with aberrant ventricular conduction (i.e., supraventricular tachycardia [SVT] with aberrancy).
The four major classes of supraventricular tachyarrhythmia∗ are sinus tachycardia, paroxysmal supraventricular tachycardia (PSVT), atrial flutter, and AF. With each class, cardiac activation occurs at one or more sites in the atria or AV junction (node), above the ventricles (hence supraventricular). This activation sequence is in contrast to ventricular tachycardia (VT) in which the depolarization impulses originate in the ventricles. VT is simply a run of three or more consecutive premature ventricular depolarizations (see Chapter 16). The QRS complexes are always wide because the ventricles are not being stimulated simultaneously. The rate of VT is usually between 100 and 200 beats/min. By contrast, with supraventricular arrhythmias the ventricles are stimulated normally (simultaneously), and the QRS complexes are therefore narrow (unless a bundle branch block is also present).
Differential Diagnosis of Narrow Complex Tachyarrhythmias
PSVT and AF can generally be distinguished on the basis of their regularity. PSVT resulting from AV nodal reentry or a concealed bypass tract is usually an almost perfectly regular tachycardia with a ventricular rate between 140 and 250 beats/min (see Chapter 14). AF, on the other hand, is distinguished by its irregularity. Remember that with rapid AF (Fig. 20-6) the f waves may not be clearly visible, but the diagnosis can be made in almost every case by noting the absence of true P waves and the haphazardly irregular QRS complexes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree