Basic Thoracic Anatomy and Physiology
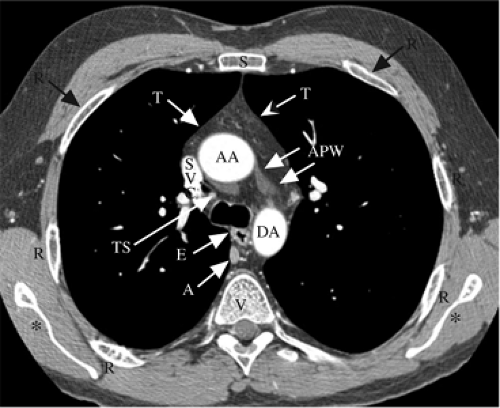
An understanding of thoracic imaging requires knowledge of the anatomy being imaged, as described in this chapter, as well as the imaging techniques applied to the thorax, covered in Chapter 2. Table 1.1 lists the major anatomic structures within the thorax that are discussed. The anatomic illustrations are presented as either line drawings or as computed tomography (CT) renderings of thoracic anatomy generated from 16-row multidetector CT examinations of the thorax at thin collimation.
Chest Wall
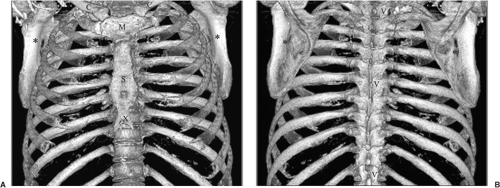
The thoracic contents are bounded by the chest wall, providing both the shape of the thorax and protection for the intrathoracic contents (Table 1.2). The skin, subcutaneous tissues, and muscles that surround the rib cage and shoulder girdle appear radiographically indistinguishable from each other, whereas on CT the skin, fat, and muscles are recognized by their difference in attenuation. The hard endoskeleton of the thorax is comprised primarily of the ribs, sternum, and spine anchored to the shoulder girdle by the clavicles, scapulae, and surrounding muscles (Fig. 1.1).
Ribs
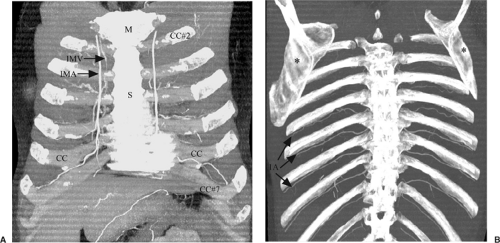
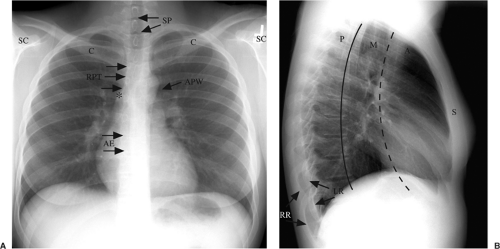
The obliquely oriented ribs are slanted anteriorly in a downward direction laterally to medially (Figs. 1.2A and 1.3A), whereas the posterior ribs are slanted in an upward direction from laterally to medially (Figs. 1.2B and 1.3B) (1). On the inferior inner surface is a costal groove, in which an intercostal artery, vein, and nerve run. Posteriorly, the ribs articulate with the spine, and anteriorly the costochondral cartilages (first to seventh) are attached to the sternum and a cartilaginous bridge (eighth to twelfth). Anteriorly, the costochondral cartilages are radiolucent in childhood through young adulthood, gradually calcifying with advancing age. There are gender-specific patterns by which this cartilage calcifies. In women the central portion calcifies first, whereas in men the upper and lower borders calcify first (2). The first costochondral cartilage is often particularly bulky and
can mimic an underlying pulmonary nodule, particularly when asymmetric. The right ribs can be differentiated from the left ribs on a lateral radiograph using the “big-rib sign” (Fig. 1.3B) (3). By convention, lateral images are taken with the left side against the radiographic plate; the right ribs are therefore further from the radiographic plate and appear to be magnified or bigger because of divergence of the x-ray beam. The most common supernumerary or accessory rib is a cervical rib arising from the seventh cervical vertebra as an enlarged costal element. They occur in approximately 0.5% to 1.5% of the population, are usually bilateral, are more common in women, and may be a cause of thoracic outlet syndrome (1,4,5). Occasionally, ribs may be congenitally fused or bifid in appearance.
Usually, the thorax is wider in transverse dimension than in the anteroposterior dimension. A “barrel-shaped” chest refers to a thorax that is equally wide in both dimensions and is a sequela of chronic obstructive lung disease, such as emphysema. Along the inferior border of the first and second ribs, 1 to 5 mm thick “companion shadows” are seen on radiographs in approximately one-third of individuals and are due to adjacent fat (6,7); they should not be mistaken for a pneumothorax (Chapter 17).
can mimic an underlying pulmonary nodule, particularly when asymmetric. The right ribs can be differentiated from the left ribs on a lateral radiograph using the “big-rib sign” (Fig. 1.3B) (3). By convention, lateral images are taken with the left side against the radiographic plate; the right ribs are therefore further from the radiographic plate and appear to be magnified or bigger because of divergence of the x-ray beam. The most common supernumerary or accessory rib is a cervical rib arising from the seventh cervical vertebra as an enlarged costal element. They occur in approximately 0.5% to 1.5% of the population, are usually bilateral, are more common in women, and may be a cause of thoracic outlet syndrome (1,4,5). Occasionally, ribs may be congenitally fused or bifid in appearance.
Usually, the thorax is wider in transverse dimension than in the anteroposterior dimension. A “barrel-shaped” chest refers to a thorax that is equally wide in both dimensions and is a sequela of chronic obstructive lung disease, such as emphysema. Along the inferior border of the first and second ribs, 1 to 5 mm thick “companion shadows” are seen on radiographs in approximately one-third of individuals and are due to adjacent fat (6,7); they should not be mistaken for a pneumothorax (Chapter 17).
Table 1.1: Thoracic Anatomy Overview | |
|---|---|
|
Table 1.2: The Chest Wall | ||||||||
|---|---|---|---|---|---|---|---|---|
|
In women the central portion of the costochondral cartilage calcifies first; in men the upper and lower borders calcify first.
The “big-rib sign” on a lateral radiograph is used to identify the right ribs.
On axial CT images, only a portion of each rib is seen because of their oblique orientation. Counting the ribs on CT can be done using three anatomic landmarks: clavicular heads (rib 1), sternal angle (rib 2), and xiphoid process (rib 7). The first rib can be found behind the medial third of the clavicle (8). This is the method we generally use, acknowledging this is tedious when counting down to the lower most ribs. The second costochondral cartilage anteriorly is located at the sternal angle; this method can also be used on a lateral radiograph. Finally, the seventh costochondral cartilage can be found at the xiphoid process (1); this landmark is less consistent (Fig. 1.2A).
Counting the ribs on CT can be done using three landmarks, from which successive ribs can be counted in the posterior direction.
Sternum
The sternum forms the midline anterior portion of the thoracic cage and is made up of the manubrium (the thickest portion; articulates with the clavicles), the sternal body, and the xiphoid process (Figs. 1.1A, 1.2A, and 1.4). The sternal notch, also known as the jugular notch, is at the upper manubrium border; palpating this area reveals the trachea. The sternal angle is formed by the manubrium and sternal body and is also known as the angle of Louis. On a chest radiograph it is at the T-4 vertebral body level.The xiphisternal articulation is at the T-9 vertebral body level. Seven costochondral cartilages articulate with the sternum. Deformities of the sternum occur in 1 in 300 people and are usually of little clinical consequence, other than being aesthetically unattractive; when severe, respiratory symptoms may occur (9). The most common is pectus excavatum, also known as “funnel chest”; it represents depression of the sternum from its normal location, easily recognizable on lateral radiographs. On a frontal radiograph it may cause blurring of the right heart border, mimicking a right middle lobe process, with displacement of the heart to the left, and exaggerated anterior angulation of the ribs. Pectus carinatum or “pigeon breast” represents abnormal protrusion of the sternum; the middle and lower sternum are most commonly involved (9,10). There may be an association with congenital heart disease in up to 10% of individuals. A sternal foramen is an incidental focal defect in ossification or failure
of union of embryonic elements that form the sternum, readily visible on CT as a hole in the sternum. Although the sternum is difficult to evaluate on chest radiographs, particularly on the frontal views, it can be evaluated in great detail with CT.
of union of embryonic elements that form the sternum, readily visible on CT as a hole in the sternum. Although the sternum is difficult to evaluate on chest radiographs, particularly on the frontal views, it can be evaluated in great detail with CT.
On a posteroanterior radiograph, the sternal angle is at the T-4 vertebral body level.
Pectus excavatum creates an ill-defined right heart border on a posteroanterior radiograph.
Shoulder Girdle
Together the clavicles and scapulae, otherwise know as collar bone and shoulder blades, form the shoulder girdle (Figs. 1.1, 1.2, and 1.3). The clavicle is a double-curved bone that medially articulates with the sternum and laterally with the acromion of the scapula; both are synovial joints. Numerous ligaments anchor the clavicle as well, including the costoclavicular and sternoclavicular ligaments medially and the acromioclavicular and coracoclavicular ligaments laterally. The rhomboid fossa is a notch that is occasionally seen radiographically on the undersurface of the medial clavicle 1 to 2 cm from the sternal articulation and is the location from which the costoclavicular ligament arises. The interspace between the first and second ribs anteriorly can be palpated immediately below the medial clavicle.
The scapulae are thin flat bones with a thick ridge or spine projecting posteriorly. The costal surface of the scapula faces the ribs and is concave, containing the subscapularis muscle, whereas the dorsal surface is convex and contains the supraspinatus and infraspinatus muscles above and below the spinal ridge, respectively. Laterally the spine continues into the acromion. The superolateral aspect of the scapula is concave, forming the glenoid fossa. Superiorly there is a small scapular notch. Sprengel’s deformity, or high-riding scapula, is an uncommon congenital abnormality (11).
Spine
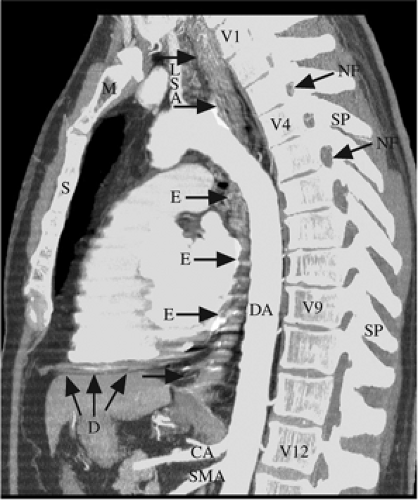
There are 12 thoracic vertebrae (Figs. 1.1B, 1.3B, and 1.4). There is less variation in the number of thoracic vertebral bodies than in the lumbosacral spine. Each vertebra is made up anteriorly of a body or corpus designed for weight-bearing, connected posteriorly to the vertebral arches that are made up of the pedicles and laminae. The cross-sectional anatomy of a thoracic vertebra is illustrated in Fig. 1.5. Progressively lower thoracic vertebrae are larger than the one above it. The bodies of adjacent vertebra articulate with each other through a cartilaginous joint containing a fibrocartilaginous intervertebral disc. The corpus and arches surround the vertebral foramen, which contains the spinal cord. The primary function of the arches is to protect the spinal cord. The spinous processes project posteriorly and inferiorly from the arches. The transverse processes project laterally from the arches. The superior and inferior articular processes project upwardly and downwardly from the laminae, respectively, to form the synovial facet joints. Spinous processes and lamina of adjacent vertebra articulate across fibrous joints. Each vertebra articulates with a pair of ribs; the rib head articulates with the upper aspect of vertebra of the same number, the tubercle with the inferior aspect. At many levels the rib head also articulates with the rib at the next lower segmental level. The space between the pedicles of two adjacent vertebra form the intervertebral foramen, through which the intercostal nerves exit the spinal canal (Fig. 1.4). The upper four thoracic vertebrae may have features of cervical vertebra, the middle four are typically thoracic, and the lower four may have features of lumbar vertebrae. There is normally kyphosis to the thoracic spine. A loss of thoracic kyphosis results in a straight thoracic spine. This “straight-spine” or “straight-back” syndrome may include thoracic scoliosis, pectus excavatum, and is associated with mitral valve prolapse (12,13).
The 12 thoracic vertebral bodies form the normal kyphosis of the posterior chest wall.
Diaphragm
The diaphragm is a dome-shaped convex-upward musculotendinous structure that separates the thoracic and abdominal cavities; it is divided into three portions. The sternal portion is the smallest and arises
from the xiphoid process. The costal portion is the largest, arising from the seventh through twelfth ribs. The vertebral (a.k.a. lumbar) portion arises from the lateral aspects of the L1-4 vertebrae in the form of two crura; the right crus is thicker and longer than the left. The fibrous component of each portion extends centrally to form the central tendon. The right hemidiaphragm is usually half an interspace higher than the left, with its upper border at the fifth anterior rib through the sixth to seventh anterior rib interspace level on the posteroanterior radiograph (4,14). There are two possible explanations: The liver below the hemidiaphragm on the right elevates it or the heart above the left hemidiaphragm pushes it down.
from the xiphoid process. The costal portion is the largest, arising from the seventh through twelfth ribs. The vertebral (a.k.a. lumbar) portion arises from the lateral aspects of the L1-4 vertebrae in the form of two crura; the right crus is thicker and longer than the left. The fibrous component of each portion extends centrally to form the central tendon. The right hemidiaphragm is usually half an interspace higher than the left, with its upper border at the fifth anterior rib through the sixth to seventh anterior rib interspace level on the posteroanterior radiograph (4,14). There are two possible explanations: The liver below the hemidiaphragm on the right elevates it or the heart above the left hemidiaphragm pushes it down.
The muscular diaphragm plays a major role in inspiration by moving caudally, generating negative intrathoracic pressure and therefore airflow into the lungs.
Three openings in the diaphragm allow passage of structures between the thorax and abdomen. The foramen for the inferior vena cava is located in the central tendon at the T8-9 intervertebral disc level to the right of midline. The midline esophageal hiatus arises within fibers of the right crus, contains the esophagus and vagus nerve, and is located at the T-10 vertebral body level. The aortic hiatus is located at the T12-L1 intervertebral disc level just to the left of midline and contains the aorta, azygos and hemiazygos veins, and thoracic duct. It actually lies behind the crura of the diaphragm where they join. A tendinous arch joins the crura together anterior to the hiatus, known as the median arcuate ligament. Where the diaphragm overlies the psoas muscles and quadratus lumborum, there is a thickening in the fascia that forms the medial and lateral arcuate ligaments, respectively. In attaching to the diaphragm, they seal the abdominal contents below the diaphragm. The diaphragm is inseparable from the abdominal structures on radiographs. On CT it is visible as a soft tissue attenuation band-like structure (Fig. 1.4).
The common congenital hernias of the diaphragm arise from failure of portions of the diaphragm to fuse. Ninety percent of these are Bochdalek hernias, which arise posterolaterally due to failure of the costal and vertebral portions of the diaphragm to fuse; these are more common on the left than the right because of the protective effect of the liver posteriorly and are usually diagnosed in neonates and young children. Although an acute hernia can be life threatening in adults because of bowel strangulation, small incidental Bochdalek hernias are common on CT, particularly in patients with long-standing obstructive lung disease (15). Morgagni hernias arise anteromedially from failure of the sternal and costal portions to fuse; these are more common on the right.
Mediastinum
The mediastinum is bounded laterally by the mediastinal pleura, inferiorly by the diaphragm, and superiorly by the thoracic inlet. It is divided into compartments. Anatomists, surgeons, and radiologists often use different definitions of these compartments. The definitions used here are based on the classification of Dr. Benjamin Felson. Many have said that the specification of “compartment” is artificial today, because the use of cross-sectional imaging makes discrete localization of abnormalities possible. However, the compartments convey information on anatomic localization, imply differential diagnoses, and are very applicable when interpreting chest radiographs. The easiest way to describe these compartments is by drawing two vertical lines on a lateral radiograph (Fig. 1.3B). The anterior mediastinum is everything anterior to the line drawn along the anterior aspect of the trachea, continuing inferiorly along the posterior heart border. The posterior mediastinum is everything posterior to the line drawn one-third of the vertebral body width behind the anterior border of the spine. Everything between these two lines is the middle mediastinum. Many classifications (but not this one) place the heart in the middle mediastinum. The aortopulmonary window is that part of the mediastinum that is between the main pulmonary artery and the aortic arch and is normally concave to flat on the posteroanterior radiograph (Figs. 1.3A and 1.5). The left recurrent laryngeal nerve runs in the aortopulmonary window; hence, masses in this location may be associated with left vocal cord paralysis and hoarseness. The contents of the mediastinal compartments are listed in Table 1.3. The borders of the cardiopericardial silhouette and mediastinum are described in Chapter 3.
The left recurrent laryngeal nerve runs in the aortopulmonary window; new hoarseness or vocal cord paralysis may be due to a mass in this location.
Esophagus
The esophagus is a vertically oriented structure that runs the length of the middle mediastinum, anterior to the spine, just to the left of midline, posterior to the airway, and to the right of the descending thoracic aorta (Figs. 1.4 and 1.5). The esophagus is divided into thirds. The proximal 5 cm long cervical esophagus begins at the cricoid cartilage at the C-6 vertebral body level and ends at the thoracic inlet. The middle third of the esophagus begins at the thoracic inlet and ends at the tracheal carina, whereas the lower third extends from the carina to the gastric fundus at the gastroesophageal junction, located at the T-11 vertebral body level (16). The reflection of the right mediastinal pleura against the vertically oriented esophagus and azygos vein forms the azygoesophageal recess below the level of the azygos arch (Fig. 1.3A). Smooth indentations are noted on the esophagus at the level of the aortic arch and the left main bronchus during an esophagram. The esophagus is a muscular organ made up of striated muscle proximally and smooth muscle distally, the primary function of which is the propulsion of food. The resting state of the esophagus is collapsed, becoming distended transiently when liquid or solid material is swallowed. The esophageal wall has mucosal, submucosal, and muscular layers, but unlike the stomach and intestines does not possess an adventitia or covering serosal layer. This permits the spread of esophageal malignancy directly into the mediastinum.
Displacement of the azygoesophageal recess to the right in the subcarinal region indicates a subcarinal mass, such as a bronchogenic cyst or lymph node mass. Displacement just above the diaphragm is most commonly due to a hiatal hernia.
Unlike the rest of the gastrointestinal tract, the esophagus has no outer adventitial layer to impede the spread of malignancy.
Table 1.3: Mediastinal Compartments and Their Contents | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Thymus
The thymus is a bilobed gland located in the superior portion of the anterior mediastinum behind the manubrium, anterior to the trachea, aortic arch, great vessels, and the brachiocephalic veins, extending caudally onto the surface of the pericardium (Fig. 1.5). It is comprised predominantly of lymphocytes and has a connective tissue capsule. T-lymphocytes are produced in the thymus gland and migrate to other lymphoid organs in the body for maturation. This quadrilateral shaped structure is readily visible on the chest radiographs of children, reaching its largest size at age 2 (16). Over time the thymus involutes and becomes replaced with fat; more than one-half of individuals over 40 years of age have a completely fatty thymus on CT (17). On CT, the soft tissue attenuation of the thymus can be located in all individuals under 30 years of age, but in only 17% of adults over 49 years of age. By 60 years of age the thymus gland weighs less than 50% of what it weighed before 19 years of age (18). With thymic hyperplasia the thymus may be abnormally enlarged. Rebound thymic hyperplasia often occurs in children and young adults after chemotherapy or corticosteroid treatment. In contrast, follicular or lymphoid thymic hyperplasia occurs with conditions such as myasthenia gravis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree