Basic Principles in Clinical Electrophysiology
What is Normal and What is Not
A thorough understanding of normal cardiac electrophysiology is necessary to accurately identify abnormalities. This chapter will define what is normal and how to identify what is abnormal.
Abnormalities in the electrical function of the heart can be identified through measurement of baseline intervals as well as patterns of conduction.
The Sinus Node and Atrial Conduction
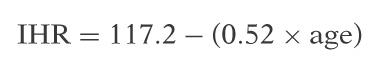
The sinus node spontaneously depolarizes between 60 and 100 beats per minute (bpm). It is markedly influenced by parasympathetic and sympathetic tone. At rest, the sinus node is largely influenced by vagal tone. Sinus arrhythmia represents the normal manifestation of respiratory variation in heart rate. This occurs through a withdrawal of vagal tone (increased heart rate) associated with inspiration. The initial increase in heart rate associated with the onset of exertion is also caused first by the withdrawal of vagal tone followed by a sustained heart rate increase due to sympathetic tone. Complete blockade of both parasympathetic and sympathetic inputs to the sinus node (atropine and β-blocker administration) allows the determination of the intrinsic heart
rate (IHR). The normal IHR is inversely related to the age of the patient and is calculated using the formula:
rate (IHR). The normal IHR is inversely related to the age of the patient and is calculated using the formula:
Testing sinus node function: The two tests used in the electrophysiology laboratory for assessment of sinus node function are called the sinus node recovery time (SNRT) and the sinoatrial conduction time (SACT).
Sinus Node Recovery Time
This is a measure of the recovery of sinus node automaticity following overdrive suppression. Unfortunately this test is not a pure assessment of automaticity alone, because conduction into and out of the sinus node is incorporated in its measurement. The test is performed by pacing the atrium for at least 1 minute at multiple cycle lengths above the intrinsic sinus rate. The sinus node is suppressed and once pacing is stopped the time required for sinus node automaticity to recover is measured. The corrected SNRT is used in clinical practice and is calculated by taking the longest interval from cessation of pacing to spontaneous sinus node activity (SNRT) and subtracting it from the baseline sinus cycle length (SCL). This is the most widely used electrophysiologic measure of sinus node function.
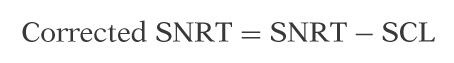
The normal corrected SNRT is 500 to 600 msec.
The SNRT may be falsely normal in patients with true sinus node dysfunction but slow sinus node cycle lengths.
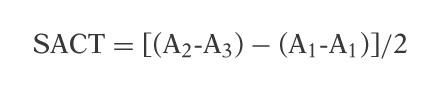
Sinoatrial Conduction Time
SACT is a test of sinus node function, which is performed with the introduction of premature atrial stimuli during sinus rhythm following an 8- to 10-beat stable drive train at a cycle length just shorter than sinus. This test assumes that the time required to enter the sinus node is equal to the conduction time out of the sinus node and back to the recording/stimulating catheter (may not be true). It is calculated by subtracting the baseline SCL or A1-A1 from the time it takes for the sinus node to recover from the premature stimulus (A2-A3) divided by two for the time in and out of the sinus node.
Influences on Sinus Node Function
Enhanced: Catecholamines and withdrawal of vagal tone; denervation.
Inhibited: Drugs, trauma, fibrosis, ischemia, and congenital dysfunction.
Atrioventricular Node Function
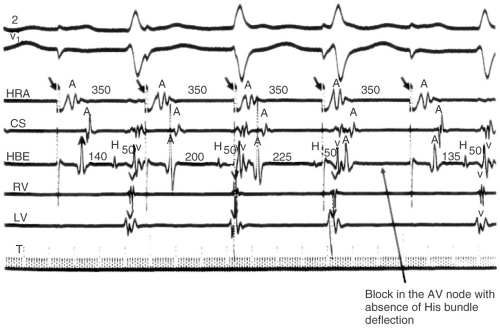
As noted, the atrioventricular (AV) node exhibits slower or decremental conduction in response to rapid atrial pacing or the introduction of premature stimuli to the AV node. Progressively rapid fixed cycle length pacing (A1-A1) is used to determine the AV Wenckebach (WB) cycle length. This critical cycle length is reached when there is atrial capture without capture of the His bundle or ventricle (see Fig. 5-1). The AV nodal WB cycle length is markedly influenced by the autonomic state. In general, antegrade AV nodal function is considered normal if there is conduction below a cycle length of 500 msec
(heart rate >120 bpm). AV nodal WB generally occurs below 500 msec and above 300 msec. If 1:1 conduction persists below 300 msec, this is considered enhanced AV nodal conduction. Conversely, AV nodal WB that occurs at rates slower than 600 msec (100 bpm) is considered abnormal. In patients with high vagal tone or on AV nodal blocking drugs, WB may occur at long cycle lengths. It is common and normal for well-trained athletes to exhibit WB while sleeping, particularly if during exercise AV conduction is normal.
(heart rate >120 bpm). AV nodal WB generally occurs below 500 msec and above 300 msec. If 1:1 conduction persists below 300 msec, this is considered enhanced AV nodal conduction. Conversely, AV nodal WB that occurs at rates slower than 600 msec (100 bpm) is considered abnormal. In patients with high vagal tone or on AV nodal blocking drugs, WB may occur at long cycle lengths. It is common and normal for well-trained athletes to exhibit WB while sleeping, particularly if during exercise AV conduction is normal.
The introduction of progressively premature stimuli is used to determine the refractory period of AV node. The atrioventricular nodal effective refractory period (AVNERP) is identified by a premature atrial stimuli, which captures the atrium without conduction to the His bundle or ventricle. It is measured in the His bundle electrogram. This must be distinguished from the atrial effective refractory period (AERP) that is reached by the longest A1-A2 interval, which fails to capture the atrium (see Chapter 4).
The physiological response to premature atrial stimuli is a progressive increase in A2-H2 interval as the A1-A2 interval becomes progressively shorter. This prolongation in the A2-H2 interval continues with progressively premature atrial stimuli until the refractory period of the atrium (AERP) or the AV node is reached (AVNERP).
In some patients, the introduction of progressively premature atrial stimuli will be associated with an abrupt (rather than the usual gradual) prolongation in the AH interval. This phenomenon is commonly referred to as dual AV nodal pathways. In this paradigm, there is conduction over two or, in some cases, multiple pathways. It is likely that these pathways represent different functional properties of the cells in the AV nodal region as opposed to distinct anatomic routes.
Dual Atrioventricular Nodal Pathways
Dual or multiple AV nodal pathways are present in 7% of the population representing a normal variation in human physiology. Most commonly there is a rapidly conducting (fast) and a slowly conducting (slow) pathway. Conduction over the fast pathway is associated with rapid (short AH interval) conduction and a long refractory period. In contrast, conduction over the slow pathway is associated with a long AH interval and a shorter refractory period. In patients with dual AV nodal pathways, conduction occurs over the fast pathway in most circumstances (short or normal PR interval). Conduction switches to the slow pathway when the refractory period of the fast pathway is reached and a “jump” to the slow pathway results (see Fig. 5-2). With the introduction of premature atrial stimuli a jump from the fast to the slow pathway is defined by a ≥50 msec increase in the A2-H2 interval in response to a 10 msec decrease in the A1-A2 coupling interval. This jump is most often elicited with the introduction of atrial premature stimuli but can occasionally be identified with straight fixed cycle length pacing.
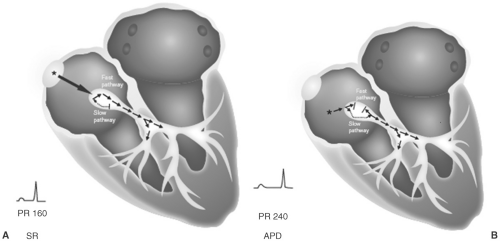 FIGURE 5-2. Schema of dual atrioventricular (AV) nodal pathways. A: Demonstrates conduction down both the fast and slow pathways with a normal PR interval of 160 msec. B: Demonstrates an atrial premature depolarization (APD) with block in the fast pathway and conduction down the slow pathway yielding a longer PR interval of 240 msec. SR, sinus rhythm. (See color insert.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|