Introduction
Hundreds of millions of premature tobacco deaths could be avoided if effective interventions could be widely applied in all countries. Numerous studies from high -income countries, and a growing number from low- and middle-income countries, provide robust evidence that tobacco tax increases, timely dissemination of information about the health risks from smoking, restrictions on smoking in public and work places, comprehensive bans on advertising and promotion, and increased access to cessation therapies are effective in reducing tobacco use and its consequences. Cessation by the 1.1 billion current smokers is central to meaningful reductions in tobacco deaths over the next five decades. Reduced uptake of smoking by children would yield the benefits chiefly after 2050. Price and non-price interventions are, for the most part, highly cost effective.
This chapter begins with an overview of smoking trends and tobacco’s health consequences, with a focus on cardiovascular disease mortality and morbidity from smoking. A review of the effectiveness of personal and population-level tobacco control interventions in reducing cardiovascular disease burden follows. Finally, the constraints to implementing tobacco control policies are discussed.
Tobacco use, in both smoked and non-smoked forms, is common worldwide. This chapter focuses on smoked tobacco because smoked tobacco is more common, accounting for about 65–85% of all tobacco produced worldwide,1 and causes more disease and more diverse types of disease than does oral tobacco use.
Prevalence
A systematic review of 139 studies on adult smoking prevalence2 found that over 1.1 billion people worldwide smoke, with about 82% of smokers residing in low-and middle-income countries. Table 9.1 provides an update of these estimates for the population in 2000. Globally, male smoking far exceeds female smoking, with a smaller gender difference in high-income countries. Smoking prevalence is highest in Eastern Europe and Central, Southern and Eastern Asia, where about 50% of all adults are smokers.
Table 9.1 Estimated smoking prevalence (by gender) and number of smokers, 15 years of age and over, by World Bank Region, 2000
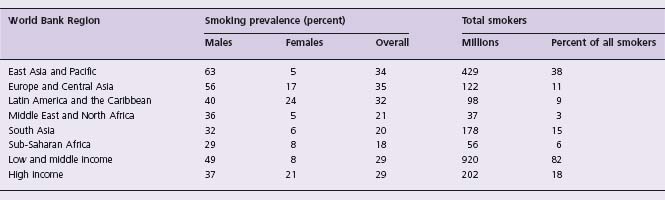
While overall smoking prevalence continues to increase in many low-and middle-income countries, many high-income countries have witnessed decreases, most clearly in men. A study in 36 mostly Western countries, from early 1980 to the mid-1990s, suggested that the decrease in smoking prevalence observed among men was due to the higher prevalence in younger age groups of those who have never smoked. Among women, there was little overall change in smoking prevalence because the increasing prevalence of smokers in younger age cohorts counterbalanced increasing cessation in older age groups.3
Cessation
Ex-smoking rates are a good measure of cessation at a population level. In some high-income countries, the prevalence rates of ex-smokers have increased over the past two to three decades. For example, in the United Kingdom, smoking prevalence among males over age 30 fell from 70% in the 1950s to 30% in 2000; female smoking prevalence fell from 40% to 20% over the same period. Much of the decrease arose from cessation. Today, there are twice as many ex-smokers as smokers among those currently aged 50 or over. Currently, 40% of the British male population is made up of former smokers.4 Polish male cessation rates have also increased, partly due to control programs. One out of every four adult Polish males described himself as an ex-smoker.5 In contrast, the prevalence of male ex-smokers in most developing countries is low: 10% in Vietnam, 5% in India, and 2% in China.2,6,7 Even these low figures may be falsely elevated because they include people who quit either because they are too ill to continue or because of early symptoms of tobacco-related illness.8
The health consequences of smoking
The health consequences of smoking are often assumed to be widely understood. In fact, there is wide ignorance of the magnitude of tobacco hazards, in terms of individual health and population policy. Thus, the salient aspects of tobacco epidemiology are outlined in this section.
Key messages for the individual smoker
Over 50 years of epidemiology on smoking-related diseases have led to three key messages for individual smokers worldwide.9,10
- The eventual risk of death from smoking is high, with about one-half of long-term smokers eventually being killed by their addiction.
- These deaths involve a substantial amount of life-years foregone. At least half of all tobacco deaths occur at ages 35-69, losing about 20-25 years of life, compared to the life expectancy of non-smokers.
- Cessation works. Those adults who quit before middle age avoid almost all the excess hazards of continued smoking.
Globally, an estimated 1.6 million cardiovascular deaths were attributable to smoking in the year 2000; that is, 11% of all global cardiovascular deaths over the age of 30.11 Detailed epidemiologic reviews of worldwide mortality from smoking are found elsewhere.7,12–16 The following discussion focuses on the consequences of smoking on adult cardiovascular mortality.
Key messages for heart health
The wealth of evidence linking smoking and cardiovascular disease points to three key messages pertaining to cardiovascular health.
- Heart attacks and strokes can strike suddenly and can be fatal if treatment is not sought immediately.
- Heart attacks and strokes are made more common by smoking.
- Quitting tobacco use reduces the chance of a heart attack or stroke, with benefits seen shortly after quitting.
Risks of cardiovascular disease from smoking
The relative risks of fatal and non-fatal heart disease associated with smoking from selected studies7,15,17-20 are depicted in Table 9.2. Overall, the relative risk of non-fatal myocar-dial infarction is higher than that of fatal disease, and risks are higher for males and at younger ages.
Table 9.2 Tobacco use and cardiovascular disease risks in selected studies
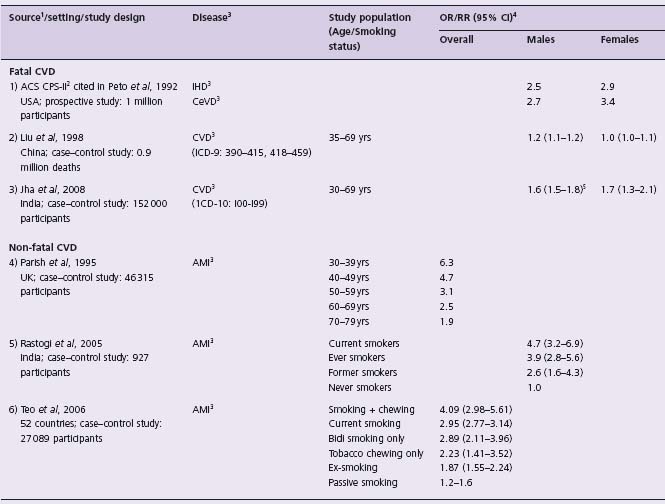
1 References: 7, 15, 17–20
2 American Cancer Society–Second Cancer Prevention Study
3 IHD, ischemic heart disease; CeVD, cerebral vascular disease; CVD, cardiovascular disease; AMI, acute myocardial infarction;
4 OR/RR (95% CI), odds ratio/ relative risk (95% confidence interval)
5 99% confidence interval
Current mortality and disability from smoking
A recent update of indirect estimates of global tobacco mortality21 estimated that in 2000 there were 5 million premature deaths caused by tobacco. About half (2.6 million) of these deaths were in low-income countries. Males accounted for 3.7 million deaths, or 72% of all tobacco deaths. About 60% of male and 40% of female tobacco deaths were of middle-aged persons (ages 35-69).
In high-income countries and former socialist economies, the 1 million middle-aged male tobacco deaths were largely composed of cardiovascular disease (0.45 million) and lung cancer (0.21 million). In contrast, in low-income countries, the leading causes of death among the 1.3 million male tobacco deaths were cardiovascular disease (0.4 million), chronic obstructive pulmonary disease (0.2 million), other respiratory disease (chiefly tuberculosis, 0.2 million) and lung cancer (0.18 million). The specific numbers of deaths from tobacco and of total disability-adjusted life-years (DALYs) by gender are shown in Table 9.3.21,22 Disability estimates are not discussed here; however, disability is highly correlated with mortality in most settings.
Table 9.3 Tobacco mortality and total disability-adjusted life years by gender and World Bank Region, 2000
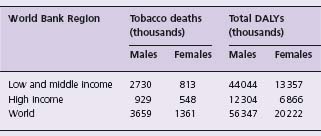
DALYs, disability-adjusted life years
References: 21,22
Cardiovascular mortality from smoking
Cardiovascular disease (CVD), which includes heart diseases and stroke, is the leading cause of death worldwide. Long a problem in high-income countries, CVD is now recognized as a global problem. CVD accounted for more than one-quarter of all deaths worldwide in 2001, with four-fifths of those deaths occurring in low-and middle-income countries.
Of the 1.6 million cardiovascular deaths worldwide in the year 2000, 1.2 million were among men and 0.4 million among women. There were 0.9 million deaths in industrialized regions and 0.7 million deaths in the developing world. The proportion of adult cardiovascular deaths attributable to smoking was 17% for men and 5% for women.11
The estimated numbers of cardiovascular deaths attributable to smoking, disaggregated by region and sex, are depicted in Table 9.4. The proportions of total adult cardiovascular deaths attributable to smoking were generally highest in industrialized regions (12–22%), where smoking has been common for several decades. At the same time, the increase in smoking over the last quarter of the 20th century in a number of developing regions, including parts of Southeast Asia, Latin America and the Eastern Mediterranean, has resulted in ≥ 10% of all current adult cardiovascular deaths being attributable to smoking, the number being higher among men.11
Table 9.4 Estimated cardiovascular mortality attributable to smoking in 14 epidemiologic subregions of the world, 2000
Source: 11
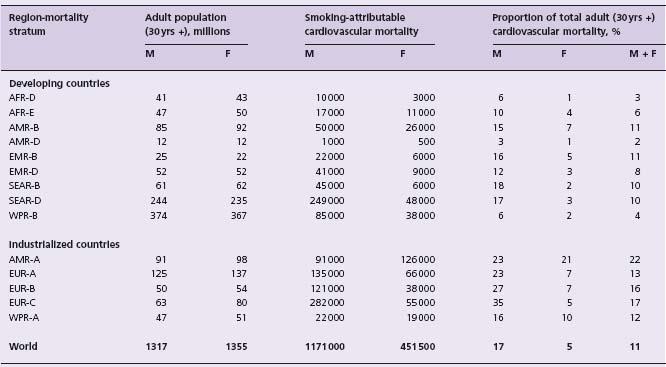
Mortality stratum: A indicates very low child mortality and very low adult mortality; B, low child mortality and low adult mortality; C, low child mortality and high adult mortality; D, high child mortality and high adult mortality; E, very high child mortality and very high adult mortality
Regions: AFR-Africa; AMR-America; EUR-Europe; EMR-Eastern Mediterranean; SEAR-South East Asian; WPR-Western Pacific
Countries: AFR-D: Algeria, Angola, Benin, Burkina Faso, Cameroon, Cape Verde, Chad, Comoros, Equitorial Guinea, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Madagascar, Mali, Mauritania, Niger, Nigeria, Sao Tome & Principe, Senegal, Seychelles, Sierra Leone, Togo. AFR-E: Botswana, Burundi, Central African Republic, Congo, Cote d’Ivoire, Congo, Eritrea, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Swaziland, Uganda, Tanzania, Zambia, Zimbabwe. AMR-A: Canada, Cuba, United States. AMR-B: Antigua, Argentina, Bahamas, Barbados, Belize, Brazil, Chile, Colombia, Costa Rica, Dominica, Dominican Republic, El Salvador, Grenada, Guyana, Honduras, Jamaica, Mexico, Panama, Paraguay, St. Kitts, St. Lucia, St. Vincent, Suriname, Trinidad & Tobago, Uruguay, Venezuela. AMR-D: Bolivia, Ecuador, Guatemala, Haiti, Nicaragua, Peru. EMR-B: Bahrain, Cyprus, Iran, Jordan, Kuwait, Lebanon, Libya, Oman, Qatar, Saudi Arabia, Syria, Tunisia, United Arab Emirates. EMR-D: Afghanistan, Djibouti, Egypt, Iraq, Morocco, Pakistan, Somalia, Sudan, Yemen. EUR-A: Andorra, Austria, Belgium, Croatia, Czech Republic, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Israel, Italy, Luxembourg, Malta, Monaco, Netherlands, Norway, Portugal, San Marino, Slovenia, Spain, Sweden, Switzerland, United Kingdom. EUR-B: Albania, Armenia, Azerbaijan, Bosnia, Bulgaria, Georgia, Kyrghyzstan, Poland, Romania, Slovakia, Tajikistan, Macedonia, Turkey, Turkmenistan, Uzbekistan, Yugoslavia. EUR-C: Belarus, Estonia, Hungary, Kazakhstan, Latvia, Lithuania, Moldova, Russia, Ukraine. SEAR-B: Indonesia, Sri Lanka, Thailand. SEAR-D: Bangladesh, Bhutan, North Korea, India, Maldives, Myanmar, Nepal. WPR-A: Australia, Brunei, Japan, New Zealand, Singapore. WPR-B: Cambodia, China, Cook Islands, Fiji, Kiribati, Laos, Malaysia, Marshall Islands, Micronesia, Mongolia, Nauru, Niue, Palau, Papua New Guinea, Philippines, South Korea, Samoa, Solomon Islands, Tongo, Tuvalu, Vanuatu, Vietnam.
Disease-specific patterns
Ezzati et al11 have estimated the total cardiovascular mortality attributable to smoking for all adults aged 30 years and over by three clusters of cardiovascular diseases (CVD): ischemic heart disease (IHD), cerebrovascular disease (CeVD), and a cluster of “other cardiovascular diseases including heart failure”. IHD accounted for the largest number of cardiovascular deaths attributable to smoking (870 000 deaths; 54% of all smoking-attributable cardiovascular deaths) globally. This was similar in both developing and industrialized regions. The difference between the two regions, however, was that cerebrovascular disease was the second most common cause of deaths (30%) in developing countries while it was least common (22%) in industrialized countries.
Past and future trends in mortality
Future increases in tobacco deaths worldwide are expected to arise from increased smoking by males in developing countries, and by women worldwide. Such increases are a product of population growth and increased age-specific tobacco mortality rates, the latter relating to both smoking duration and the amount of tobacco smoked. Peto et al23 have made the following calculation: if the proportion of young people taking up smoking continues to be about half of men and one-tenth of women, then there will be about 30 million new long-term smokers each year. As noted above, epidemiologic studies in developed and developing countries suggest that half of these smokers will eventually die from smoking. However, conservatively assuming that “only” about one-third of smokers die as a result of smoking, then smoking will eventually kill about 10 million people a year. Thus, for the 25-year period from 2000–2025, there would be about 150 million tobacco deaths or about 6 million deaths per year on average; from 2025–2050, there would be about 300 million tobacco deaths, or about 12 million deaths per year.
Further estimations are more uncertain but based upon current smoking trends and projected population growth, from 2050–2100 there would be an additional 500 million tobacco deaths. These projections for the next three to four decades are comparable to retrospective and early prospective epidemiologic studies in China,6,15,16 which suggest that annual tobacco deaths will rise to 1 million before 2010 and 2 million by 2025, when the young adult smokers of today reach old age. Similarly, results from a large retrospective study in India indicate that the annual number of deaths from smoking will be about 1 million during the 2010s, with about 70% (600 000 among men and 100 000 among women) occurring in middle age, rather than old age.7 With other populations in Asia, Eastern Europe, Latin America, the Middle East and, less certainly, sub-Saharan Africa showing similar growth in population and age-specific tobacco death rates, the estimate of some 450 million tobacco deaths over the next five decades appears to be plausible. Almost all of these deaths will be among current smokers.
Benefits of tobacco cessation
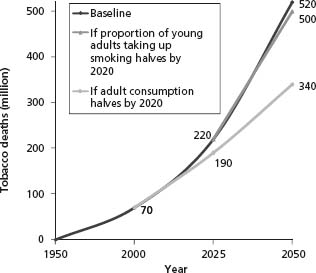
Current tobacco mortality statistics reflect past smoking behavior, given the long delay between the onset of smoking and the development of disease. The prevention of a substantial proportion of these tobacco deaths before 2050 requires adult cessation. For example, halving the per capita adult consumption of tobacco by 2020 (akin to the declines in adult smoking in the United Kingdom) would avert about 180 million tobacco deaths. Continuing to reduce the percentage of children who start to smoke will prevent many deaths, but its main effect will be on mortality rates in 2050 and beyond (Fig. 9.1).6,24–26
Figure 9.1 Tobacco deaths in the next 50 years under current smoking patterns. Note: Peto and others (1994) estimate 60 million tobacco deaths between 1950 and 2000 in industrial countries. This figure estimates an additional 10 million between 1990 and 2000 in developing countries. The figure also assumes no tobacco deaths before 1990 in developing countries and minimal tobacco deaths worldwide before 1950. Projections for deaths from 2000 to 2050 are based on Peto and Lopez, 200024,26.
There is substantial evidence that smoking cessation reduces the risk of death from tobacco-related diseases. Among doctors in the United Kingdom, those who quit smoking before the onset of major disease avoided most of the excess hazards of smoking.10 The benefits of quitting were largest in those who quit before middle age (between ages 25 and 34 years), but were still significant in those who quit later (between ages 45 and 54 years).
Benefits of cessation on cardiovascular disease burden
Smoking cessation interventions have been identified to be effective in the general population of smokers for primary prevention of heart disease. In a pooled cohort study of over 19 000 normal adults with a mean duration of follow-up of 13.8 years, it was noticed that people who stopped smoking had a decreased risk of myocardial infarction (hazard ratio (HR) 0.71, 95% confidence interval (CI) 0.59–0.85), after adjustment for other risk factors.27
Quitting smoking has also been found to be effective in patients with cardiovascular disease in the prevention of recurrence of further fatal and non-fatal cardiovascular events. Patients who quit smoking after successful percutaneous coronary intervention were at lower risk for rein-farction and death than those who continued to smoke.28 In those who had undergone coronary artery bypass grafting, it was associated with reduced long-term mortality (relative risk (RR) 0.4–0.6) and need for repeat interventions (RR 0.6–0.7).29,30 Efficacy of tobacco cessation strategies in reducing subsequent cardiovascular mortality up to 50% has been shown in both hospital-based and clinic-based settings for smokers with coronary heart disease.31–34
Interventions to reduce demand for tobacco
Numerous studies, mostly from high-income countries, have examined the impact of interventions aimed at reducing the demand for tobacco products on smoking and other kinds of tobacco use. The small but growing number of studies from low-and middle-income countries provide useful lessons about differences in the impact of these interventions between these countries and high-income countries. The following is a review of the impact of price and non-price interventions to reduce demand for smoking, including a discussion of each intervention’s impact on initiation and cessation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


