Atrioventricular Septal Defect
This anatomic complex has been referred to as an atrioventricular canal. The septal defect includes the inferior segment of the atrial septum and the superior segment or the inflow portion of the interventricular septum. The atrioventricular valves are developed in an abnormal, but varied manner.
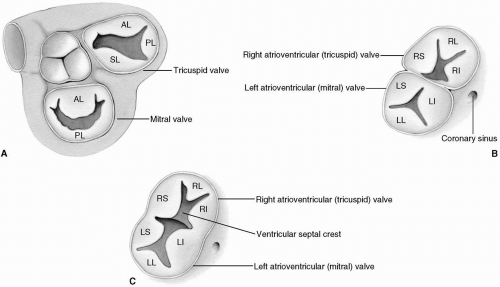
In all but the mildest forms, there is a common atrioventricular valve, which is made up of six leaflets of variable size and shape attached to normally or abnormally located papillary muscles by chordae tendineae. This common atrioventricular valve can be subdivided into mitral and tricuspid components or segments, each with three leaflets. The leaflets constituting the tricuspid valve are designated right superior, right inferior, and right lateral, and those comprising the mitral valve are designated left superior, left inferior, and left lateral (Fig. 22-1).
It is of clinical and anatomic significance that in normal hearts, the anterior mitral leaflet contributes to one-third, and the posterior leaflet contributes to two-thirds of the annulus of the mitral valve. In an atrioventricular septal defect, this ratio is reversed; the posterior (left lateral) leaflet contributes to one-third and the bileaflet anterior cusp (the left superior and inferior leaflets together) contributes to two-thirds of the mitral valve annulus (Fig. 22-2).
From the clinical point of view, however, there are partial, intermediate, and complete forms of atrioventricular septal defects. In the partial form, there exists an ostium primum type of interatrial septal defect. Here the atrioventricular valves are attached to the crest of the interventricular septum, and there is usually no interventricular communication below the valves. The anterior leaflet of the mitral valve, which has a cleft of varying degree, is considered to form part of a trileaflet mitral valve (Fig. 22-1B). In most patients, the mitral valve is competent.
The intermediate form is similar to the partial form of atrioventricular septal defect. The main distinguishing feature is the incomplete attachment of the atrioventricular valves to the ventricular septum. This results in usually multiple small interventricular communications. Varying degrees of underdevelopment of the leaflet tissues may also be present.
The complete form of atrioventricular septal defect, as its name implies, is a defect in both the lower atrial and upper ventricular septum. The configuration and details of the attachment of the atrioventricular leaflets to the ventricular septum are quite variable.
Rastelli reviewed atrioventricular canal specimens obtained at autopsy at the Mayo Clinic and proposed a classification of atrioventricular septal defects that essentially focuses on the shape, size, location, and details of the attachments of the left superior leaflet. In type A, which is commonly seen, the left superior leaflet is over the left ventricle and its chordal attachment is to the crest of the ventricular septal defect (Fig. 22-3A).
In type B, which is rare, the chordal attachment of the left superior leaflet is to an abnormally located papillary muscle on the right ventricular aspect of the interventricular septum (Fig. 22-3B). In type C, which is seen quite often, the left superior leaflet is large and bridges the ventricular septal defect and right ventricle. Its chordal attachments are variable (Fig. 22-3C). It is a matter of the degree of overriding of the left superior leaflet on the ventricular septum that determines the type of defect.
Approximately 10% of patients have unbalanced atrioventricular septal defects. If the common atrioventricular valve is located more over the right ventricle, the left ventricle and other left-sided structures may be underdeveloped. When the common atrioventricular valve sits predominately over the left ventricle, a hypoplastic right ventricle with or without pulmonary outflow tract obstruction is usual.
Ostium Primum Atrial Septal Defect
The ostium primum type of atrial septal defect is part of the atrioventricular septal defect complex, sometimes referred to as a partial form of the atrioventricular canal. Clinically, a large ostium primum that is usually nonrestrictive is seen, but there is also always a cleft in the anterior leaflet of the mitral valve (Fig. 22-4). The mitral valve in these cases should be considered a trileaflet structure, and this should be kept in mind whenever a repair is attempted.
Incision
This form of atrial septal defect is usually approached through a median sternotomy. A right submammary thoracotomy incision can also be used (see Chapter 1).
Cannulation
The ascending aorta is cannulated in the usual manner (see Chapter 2). The superior vena cava is cannulated directly, and the inferior vena cava is cannulated through the atrial wall just above the origin of the inferior vena cava. Tapes are then passed around both cavae. A vent is placed through the right superior pulmonary vein and positioned in the left atrium proximal to the mitral valve. (The correct position can be obtained after the heart is opened.)
Myocardial Preservation
Cold cardioplegic arrest of the heart is achieved and maintained by intermittent infusion of cold blood cardioplegic solution into the aortic root (see Chapter 3).
Technique
A generous atriotomy is made from the base of the right atrial appendage to near the site of the inferior vena cava cannulation, parallel with the atrioventricular groove. The atriotomy edges are retracted with fine sutures that are sometimes pledgeted. The presence and severity of mitral regurgitation must be carefully assessed. This may be carried out by simply injecting saline forcefully through the mitral valve. The cleft on the anterior leaflet of the mitral valve should probably always be closed even if there is no valve incompetence at the time of surgery because these valves often become insufficient over time. This can be accomplished by approximating the “kissing” edges of the cleft starting at the annulus with three or four interrupted 6-0 Prolene sutures (Fig. 22-4).
Care must be taken to approximate only the kissing edges of the leaflet tissue, which are not the same as the free edges of the cleft (Fig. 22-4C, D). Incorporation of an additional extent of the leaflet to secure a better repair usually results in valvular insufficiency. The
edges of the cleft are strong and quite fibrotic in older patients and consequently hold sutures well. In infants, the valve tissue may be somewhat friable. In these cases, horizontal mattress sutures reinforced with pericardial pledgets can be used to close the cleft.
edges of the cleft are strong and quite fibrotic in older patients and consequently hold sutures well. In infants, the valve tissue may be somewhat friable. In these cases, horizontal mattress sutures reinforced with pericardial pledgets can be used to close the cleft.
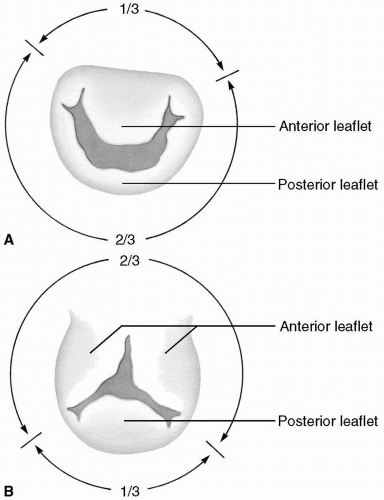 FIG 22-2. A: Normal mitral valve annular configuration. B: Mitral valve annular configuration in an atrioventricular septal defect. |
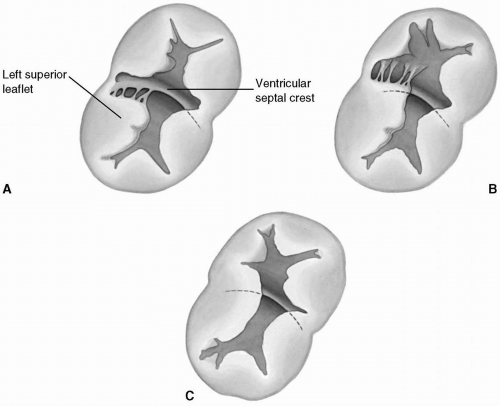 FIG 22-3. Rastelli classification of atrioventricular septal defects. A: Type A. B: Type B. C: Type C. |
It is unusual to have significant valvular incompetence in the ostium primum type of defect. When it does occur, aggressive reconstruction should be undertaken (see Mitral Valve Reconstruction section in Chapter 6). If the ostium primum defect is small and does not allow full visualization of the mitral valve, the atrial septal defect should be enlarged toward or into the fossa ovalis.
In most patients, it is not necessary to close the cleft completely. In fact, reapproximating the central portion of the cleft may distort the anterior leaflet, pulling it down into the left ventricle, causing mitral valve insufficiency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree