SEVERITY OF ATRIOVENTRICULAR BLOCK
First-Degree Atrioventricular Block
The “normal” PR interval has a duration of 0.12 to 0.20 second. First-degree AV block is generally defined as a prolongation of AV conduction time (PR interval) to >0.20 second. In analyses of records from normal young persons, the incidence of first-degree block by this definition ranged from 0.5%1 to 2%.2 In healthy middle-aged men, a prolonged PR interval in the presence of a normal QRS complex was found not to affect prognosis and to be unrelated to ischemic heart disease.3 Figure 22.2 illustrates two examples of first-degree AV block. The first of these (see Fig. 22.2A) is minor, with a PR interval of 0.24 second, and the second (see Fig. 22.2B) shows extreme PR lengthening. Note that in Figure 22.2B, the P wave is superimposed on the T wave of the preceding cycle.
Second-Degree Atrioventricular Block
By definition, second-degree AV block is present when one or more, but not all, atrial impulses fail to reach the ventricles. Examples of atrial premature beats that are not conducted because they occur early were presented in Chapter 15 (see Figs. 15.7 and 15.8). This situation is not considered AV block because it is normal. Figure 22.3 presents an example of both first- and second-degree AV block in which on-time P waves either have delayed AV conduction (first and second cycles of the series) or no AV conduction (third cycle).
A second-degree AV block may be intermittent (Fig. 22.4A) or continuous (see Fig. 22.4B). Note that in Figure 22.4A, the second-degree block occurs only after a sequence of six conducted beats, of which the first shows no AV block and the latter five show first-degree block (7:6 block). In Figure 22.4B, there is continually alternating first- and second-degree AV block with a 2:1 AV ratio. This is termed 2:1 (AV) block.
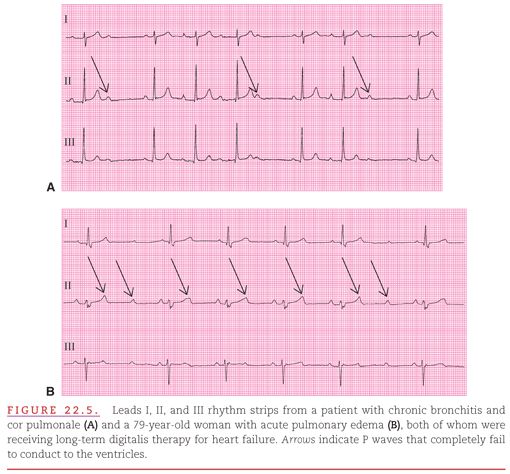
Second-degree AV block may have any ratio of P waves to QRS complexes (Fig. 22.5). In Figure 22.5A, there are the commonly appearing 3:2 and 4:3 AV conduction ratios. However, in Figure 22.5B the sinus rate is in the tachycardia range, and the more rapid “bombardment” of the AV node causes the 2:1 ratio to be intermittently increased to 3:1.
When determining the clinical significance of second-degree AV block, the atrial rate should be considered. As discussed in Chapter 17, conduction of some, but not all, atrial impulses is essential for clinical stability in the presence of atrial flutter/fibrillation. Chapter 16 (see Fig. 16.6) indicates that second-degree AV block commonly occurs along with atrial tachycardia, particularly when there is digitalis toxicity. When “AV block” occurs in the presence of an atrial tachyarrhythmia, the block itself is considered a normal occurrence and not an additional arrhythmia (Fig. 22.6A) unless the ventricular rate is reduced into the bradycardic range (see Fig. 22.6B).
When both second-degree AV block and sinus pauses are present (see Chapter 21), the cause is most likely not within the heart itself but rather in its autonomic nervous control. Second-degree AV block usually occurs in the AV node4,5 and is associated with reversible conditions such as the acute phase of an inferior myocardial infarction or treatment with digitalis, a β-adrenergic blocker, or a calcium channel–blocking drug. Because second-degree AV block is generally a transient disturbance in rhythm, it seldom progresses to complete AV block. However, in one study of 16 children manifesting second-degree AV block, 7 developed complete block.6 Chronic second-degree AV block may occasionally occur in many conditions, including aortic valve disease, atrial septal defect, amyloidosis, Reiter syndrome, and mesothelioma of the AV node.
Third-Degree Atrioventricular Block
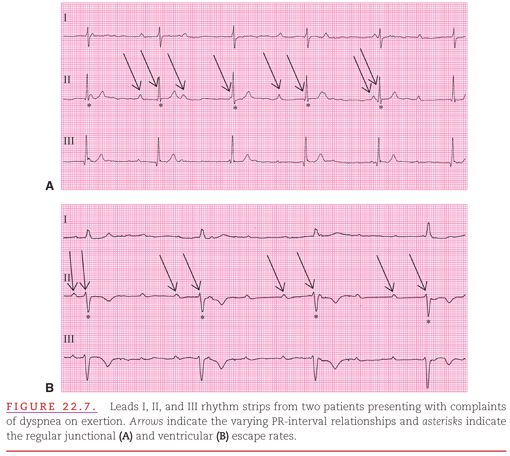
When no atrial impulses are conducted to the ventricles, the cardiac rhythm is termed “third-degree AV block,” and the clinical condition is determined by the escape capability of the more distal Purkinje cells. The junctional or ventricular escape rhythm in the presence of third-degree AV block is almost always precisely regular because these sites are not as influenced by the sympathetic/parasympathetic balance as is the sinus node. Figure 22.7A shows junctional escape in a case of third-degree AV block, but Figure 22.7B shows ventricular escape, which occurs at a slower rate.
In most clinical instances, complete AV block is at least partly compensated by an escape rhythm originating from an area distal to the site of the block. However, complete AV block of sudden onset may cause syncope with catastrophic results, or even sudden death, when there is no escape rhythm (Fig. 22.8). As seen in the figure, P waves occur immediately after the T waves, and the first two P waves are conducted without even first-degree block, but the third and all subsequent P waves are not conducted at all. Thus, third-degree AV block need not be preceded by first- or second-degree AV block.
Third-degree AV block always produces AV dissociation with its independent atrial and ventricular rhythms; however, AV dissociation may result from other sources than third-degree AV block. Decreased sinus automaticity (see Chapter 21), increased junctional and ventricular automaticity (see Chapter 16), and reentrant ventricular tachycardia (see Chapter 19) can all produce AV dissociation by creating the condition in which anterograde impulses fail to traverse the AV node. They encounter the refractoriness that follows AV nodal activation by retrograde impulses. Therefore, AV dissociation caused solely by impaired function of the AV conduction system should actually be termed “AV dissociation due to AV block” (see Fig. 22.7A, B) and AV dissociation caused solely by an accelerated distal pacing site should be termed “AV dissociation due to refractoriness” (Fig. 22.9A). Both causes can coexist, producing “AV dissociation due to a combination of AV block and refractoriness,” when there are P waves that are obviously not conducted to the ventricles but the ventricular rate is slightly above the upper limit of the bradycardic range of 60 beats per minute (see Fig. 22.9B). The term “interference” is often used to describe the condition of refractoriness that either causes or contributes to the two types of AV dissociation described here.
Often, the AV dissociation produced by third-degree AV block is “isoarrhythmic,” with similar atrial and ventricular rates and with P waves and QRS complexes occurring almost simultaneously. Insight into the presence or absence of AV block can be attained only when a P wave appears at a time sufficiently remote from a QRS complex that the ventricular refractory period would be expected to have been completed. In Figure 22.10, there is AV dissociation during the first three cycles, in which the independent sinus and ventricular rhythms are similar. Then, when variation in rate caused by respiration (sinus arrhythmia) accelerates the sinus rate but does not affect the ventricular escape focus during the fourth cycle, atrial capture occurs. This event proves AV conduction to be possible and eliminates complete AV block as a contributor to the AV dissociation.
Block in both the RBB and LBB (level C in Fig. 22.1), rather than block at the AV node or in the His bundle, is usually the cause of chronic complete AV block.7–10 Idiopathic fibrosis, called either Lev disease or Lenègre disease, is the most common cause of chronic complete AV block.7,11 Acute complete AV block within the AV node results from inferior myocardial infarction, digitalis intoxication, and rheumatic fever.12 Acute complete AV block within the bundle branches results from extensive septal myocardial infarction.13,14 Complete AV block may also be congenital, as when it results from maternal anti-Ro antibodies affecting the AV node.15
In the presence of chronic LBB or RBB block, the individual is at some risk of suddenly developing complete AV block. After this occurs, the ventricles either remain inactive (ventricular asystole; see Fig. 22.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


