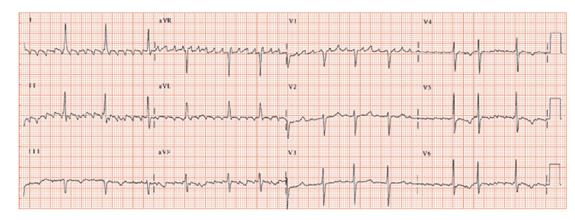
Fig. 44.2 Atrial tachycardia. This can be a challenging ECG to read. Start from first principles. Look at leads II and V1 to determine the rhythm. Lead II shows movement artefact, and in this ECG it is better to use lead I and V1. There are very frequent abnormally shaped P waves – a little less than a square separates them, so their rate is just over 300 b/min. Note: (i) the absence of an inferior lead sawtooth appearance; (ii) that in all leads there is at least some flat iso-electric lines between each beat. This cannot be atrial flutter, but is an atrial tachycardia. A variable number of P waves are conducted through to fire the ventricles, usually around 7 to 1. This is physiological, not pathological atrioventricular block. The underlying QRS complex appears unremarkable; the inferior and lateral lead T waves are flat. This ECG came from an elderly man not known to have heart disease other than atrial tachycardia.
Atrial flutter is a common arrhythmia, especially in men (perhaps as they have larger hearts) (Table 44.1). It is due to a macro re-entrant circuit in the right atrium (Fig. 44.1a–d) and results in a highly characteristic ECG appearance, with continual electrical activity best seen in the inferior leads. The ‘sawtooth’ baseline typically has a slow downstroke and a rapid upstroke. P wave activity is often reasonably well seen in lead V1, when it is predominantly positive. Occasionally the P waves in lead V1 are not well developed.
The right atrial circuit is usually of such a length that 300 circuits occur per minute. This is too fast for the atrioventricular (AV) physiologically to allow for 1 to 1 conduction down to the ventricles, and usually a fixed proportion of beats get through, often one in two, giving a QRS (and hence heart) rate of 150 b/min. This has led to an aphorism in arrhythmology; whenever a tachycardia is seen with a heart rate of exactly 150 b/min, the rhythm disturbance is atrial flutter until proved otherwise. Sometimes the conduction is 1 in 3 or 4, giving a QRS rate respectively of 100 and 75 b/min. If the rate of transmission is (in the absence of anti-arrhythmic drugs) less than this, say 1 in 5 or 1 in 6, then there is a high probability that there is also intrinsic conducting tissue disease.
Sometimes anti-arrhythmic drugs (such as propafenone) can slow the atrial rate, say to 250 b/min, sufficient for the AV node to allow 1 to 1 conduction. Thus paradoxically, some drugs used to slow the heart rate may in fact end up increasing it! This can have dangerous consequences.
Atypical atrial flutter (Table 44.1) is a rare rhythm disturbance, recognized when the deflections in the inferior leads are positive (probably as the circuit proceeds in a clockwise rotation, rather than the anti-clockwise motion of typical atrial flutter). The P wave in lead V1 is usually negative. The rate can be 300 b/min, less or more (the latter in truly atypical atrial flutter).
Prognosis of atrial flutter
Prognosis is usually that of any associated disease (chronic obstructive pulmonary disease [COPD], ischaemic heart disease [IDD], mitral/tricuspid valve disease). A high proportion of patients go on to develop atrial fibrillation. If the heart rate remains too high in untreated atrial flutter, a ‘rate-related’ cardiomyopathy can develop (with decreased left ventricular systolic function) usually reversible on rigorously controlling the heart rate.
Treatment of atrial flutter
Treatment should slow the heart rate from the usual 150 b/min to a more physiological level (beta-blockers, rate slowing Ca2+ blockers, amiodarone), possibly anticoagulation, DC cardioversion. If troublesome, atrial flutter circuit ablation is a reasonably successful procedure.
Atrial tachycardia
Atrial tachycardia is due to a rapid firing ectopic focus in the atria, either due to automaticity or due to a micro-re-entrant circuit. It is recognized by there being an iso-electric line in all the leads between each P wave, which itself has an abnormal morphology (Fig. 44.2). Like atrial flutter, the AV node cannot physiologically transmit all the impulses, and a degree of physiological block occurs, often 2 or 3 to 1. Treatment involves drugs to increase the degree of AV block to slow the QRS heart rate, cardioversion (with anticoagulant cover) and, occasionally, ablation of the abnormal focus.
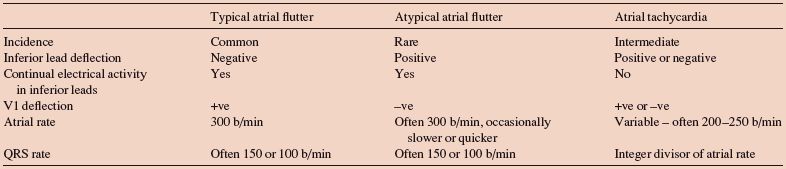
Table 44.1 Characteristics and ECG findings in regular atrial arrhythmias. Atrial fibriallation is distinguished from these arrhythmias by finding an irregular QRS rate, while these arrhythmias usually have a regular QRS rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


