Assessment of Systolic Function and Quantification of Cardiac Chambers
Quantification of cardiac chambers and assessment of ventricular systolic function are essential parts of all echocardiography examinations. New ultrasound technologies such as tissue Doppler imaging, strain imaging, and three-dimensional (3D) echocardiography have been introduced to make echocardiographic evaluation of cardiac function more quantitative and precise, but two-dimensional (2D) echocardiography is still the primary tool for chamber quantification and evaluation of left ventricular (LV) systolic function. Also, 2D echocardiography allows visualization of the endocardial border and thickening of the ventricular walls, by which global and regional ventricular systolic functions are assessed. A quantitative assessment of global systolic function is usually based on changes in ventricular size and volume. Regional (or segmental) wall motion analysis is fundamental in evaluating coronary artery disease and in performing stress echocardiography. Mechanical synchrony of regional myocardial contraction has an important role in maintaining optimal systolic function, and this can be assessed with tissue Doppler and strain imaging. Both systolic function and diastolic function change as a disease process progresses or regresses (by natural history or treatment). The treatment strategy (medications, device therapy, and surgery) for a patient’s condition is frequently guided by systolic function. Therefore, the evaluation of systolic function is a basic echocardiographic assessment in all patients because it provides the initial clues or information necessary for diagnosis, treatment, and prognosis of almost all cardiac conditions. The quantification of cardiac chambers and determination of LV volumes are essential components in clinical trials of heart failure and LV remodeling (1).
This chapter discusses the traditional and newer echocardiographic approaches to the quantification of cardiac dimensions, area, volume, mass, and systolic function. A report on recommendations for chamber quantification has been published recently by the American Society of Echocardiography (2). Normal values from the report are listed in the Appendix.
Left Ventricular and Right Ventricular Dimensions
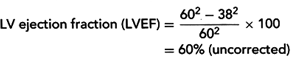
In our laboratory, LV dimensions usually are measured from 2D-guided M-mode echocardiograms of the LV at the papillary muscle level (Fig. 7-1), using the parasternal short-axis view (from the trailing edge of the septum to the leading edge of the posterior wall). When there are no regional wall motion abnormalities, the LV dimensions measured from the level of the papillary muscle of the LV can be used to calculate the LV ejection fraction
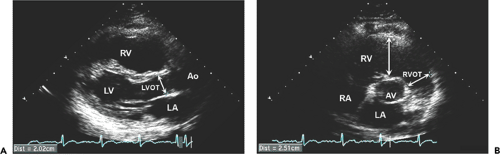
(LVEF) (Fig. 7-1). The thickness of the ventricular posterior wall and that of the ventricular septum are measured from the same M-mode echocardiogram. These values are used to calculate LV mass. The long-axis and short-axis dimensions of the ventricle can also be obtained directly from the systolic and diastolic frames of 2D parasternal long-axis and apical views (Fig. 7-2), as recommended by the American Society of Echocardiography (2). The LV end-diastolic and end-systolic dimensions are measured at the level of the mitral leaflet tips as the largest and smallest LV dimension, respectively (Fig. 7-3). Satisfactory delineation of the endocardial border is critical for reliable chamber quantification, and it can be enhanced with the administration of a perfluorocarbon contrast agent. The normal values are listed in the Appendix. These values were obtained with fundamental imaging. Harmonic imaging generally produces higher values for wall thickness (hence mass) and smaller values for dimensions and volumes.
(LVEF) (Fig. 7-1). The thickness of the ventricular posterior wall and that of the ventricular septum are measured from the same M-mode echocardiogram. These values are used to calculate LV mass. The long-axis and short-axis dimensions of the ventricle can also be obtained directly from the systolic and diastolic frames of 2D parasternal long-axis and apical views (Fig. 7-2), as recommended by the American Society of Echocardiography (2). The LV end-diastolic and end-systolic dimensions are measured at the level of the mitral leaflet tips as the largest and smallest LV dimension, respectively (Fig. 7-3). Satisfactory delineation of the endocardial border is critical for reliable chamber quantification, and it can be enhanced with the administration of a perfluorocarbon contrast agent. The normal values are listed in the Appendix. These values were obtained with fundamental imaging. Harmonic imaging generally produces higher values for wall thickness (hence mass) and smaller values for dimensions and volumes.
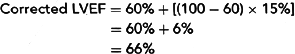
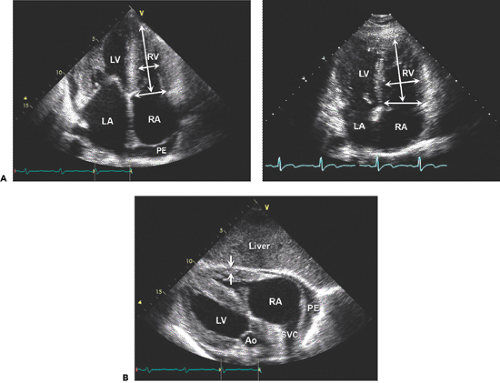
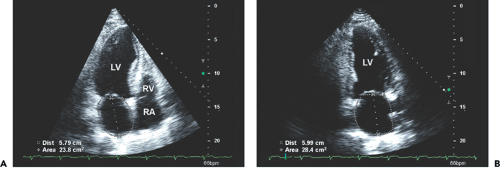
Measurements of LV dimensions are used to calculate the LVEF and are clinically useful for detecting LV dilatation and for following up patients who have valvular regurgitation, cardiomyopathy, or acute myocardial infarction. The detection of right ventricular (RV) dilatation may be the first clue to RV pressure or volume overload (Fig. 7-4) and 7-5). Chronic RV pressure overload is also accompanied by an increase in RV wall thickness in addition to dilatation, whereas RV dysplasia is associated with a thin RV wall. The thickness of the RV wall is normally less than 5 mm and is best measured from the subcostal view at the peak of the R wave (Fig. 7-4). The RV wall needs to be distinguished carefully from the trabeculations and epicardial fat. The size of the RV is best measured from the apical four-chamber view. An example of measuring the RV short axis and long axis is shown in Figures 7-2 and 7-4. The dimension of the LV outflow tract (LVOT) is measured from the parasternal long-axis view and that of the RV outflow tract is measured from the parasternal short-axis view (Fig. 7-5).
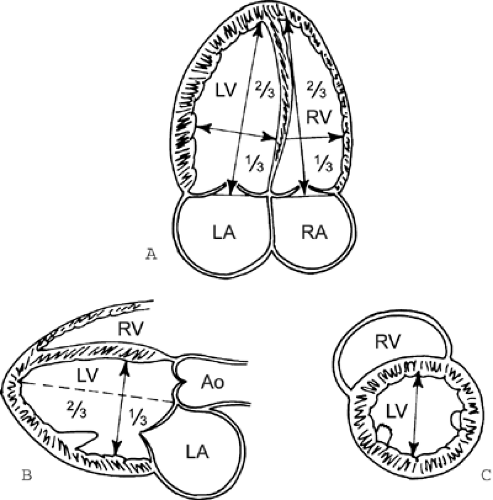 Figure 7-2 Measurement of ventricular dimensions. A: The major long axis is measured in the apical four-chamber view from the apical endocardium to the plane of the mitral valve. The minor short axis is measured from one-third the length of the long axis from the base and orthogonal to it. B: With the use of these same criteria, the long and short axes can be measured from the parasternal long-axis view, but this view rarely shows the true apex of the left ventricle (LV). C: The short axis is measured in the parasternal short-axis view at the level of the tip of the papillary muscle. Ao, aorta; LA, left atrium; RA, right atrium; RV, right ventricle. (From Schiller et al [20]. Used with permission.) |
Atrial Size and Volume
By convention, the size of the left atrium (LA) is determined from the parasternal long-axis view at end-systole (Fig. 7-3). The convention for M-mode measurements is to measure from the leading edge of the posterior aortic wall to the leading edge of the posterior LA wall (see Figure 2-17 D). However, to avoid the variable extent of space between the LA and aortic root, the trailing edge of the posterior aortic wall is recommended. The size of the LA may be
underestimated from the parasternal view because this chamber may enlarge longitudinally. Therefore, the size of the LA should also be measured from apical views (from the tip of the mitral valve to the posterior wall of the LA). The area and volume of the LA are best measured from two apical orthogonal views (2,3) (Fig. 7-6). Four different methods are used to determine LA volume: 1) prolate ellipse method, 2) biplane area-length method, 3) biplane Simpson method, and 4) 3D echocardiography.
underestimated from the parasternal view because this chamber may enlarge longitudinally. Therefore, the size of the LA should also be measured from apical views (from the tip of the mitral valve to the posterior wall of the LA). The area and volume of the LA are best measured from two apical orthogonal views (2,3) (Fig. 7-6). Four different methods are used to determine LA volume: 1) prolate ellipse method, 2) biplane area-length method, 3) biplane Simpson method, and 4) 3D echocardiography.
The prolate ellipse method requires measuring LA dimensions from the parasternal long-axis view (D1) and apical four-chamber view (D2 and D3), from which LA volume is calculated as D1 × D2 × D3 × 0.523 (Fig. 7-6). The biplane area-length method requires measuring LA area from two orthogonal apical views (A1 and A2) and LA length (L), from which LA volume is calculated as (0.85 × A1 × A2)/L (Fig. 7-6 and 7-7). When LA length is measured from two apical views, the shorter value is used to calculate LA volume. LA volume measured with the prolate ellipse method is usually 5 to 10 mL smaller than that obtained with the area-length method. Although LA volume can be measured with the biplane Simpson or 3D volumetric method, the area-length method is the method that our laboratory uses and the American Society of Echocardiography recommends. The influence of body surface area on LA volume is corrected with the use of an indexed value by dividing LA volume by body surface area. The normal value for the LA volume index is 22 ± 6 mL/m2 for all age groups. The size or volume of the LA is an important determinant of LA pressure, diastolic function, and
prognosis (4,5). The size of the RA is quantified most commonly from the apical four-chamber view. The normal RA minor dimension ranges from 2.9 to 4.5 cm.
prognosis (4,5). The size of the RA is quantified most commonly from the apical four-chamber view. The normal RA minor dimension ranges from 2.9 to 4.5 cm.
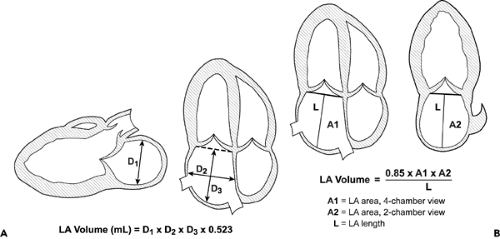 Figure 7-6 Diagrams showing left atrial (LA) volume calculations by the prolate ellipse (A) and biplane area-length (B) methods. |
Left Ventricular Mass
The two methods for calculating LV mass from 2D echocardiography are the area-length method and the truncated ellipsoid method (6,7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree