In the following pages, in alphabetical order, we provide examples of the most common appearances of the most common lung diseases encountered in reading high-resolution CT. In addition, appearances of some uncommon diseases with typical features are illustrated. It is our hope that this will serve as a quick reference and an illustrated index to the detailed descriptions of findings found elsewhere in this book.
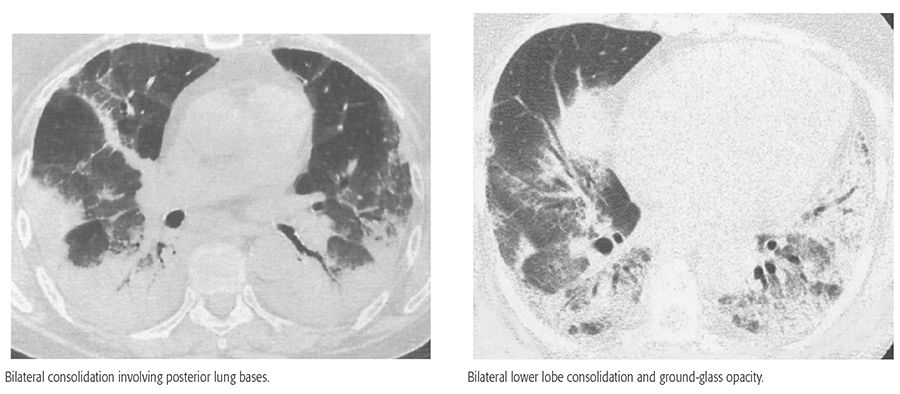
ACUTE INTERSTITIAL PNEUMONIA
(See pages 239–242 and 485–490.)
Acute interstitial pneumonia is one of the idiopathic interstitial pneumonias. It is a fulminant disease of unknown cause associated with the histologic pattern termed diffuse alveolar damage. It typically presents with symptoms and findings of acute respiratory distress syndrome.
HRCT Findings
Extensive bilateral ground-glass opacities and airspace consolidation
Architectural distortion
Abnormalities predominantly basilar and dependent
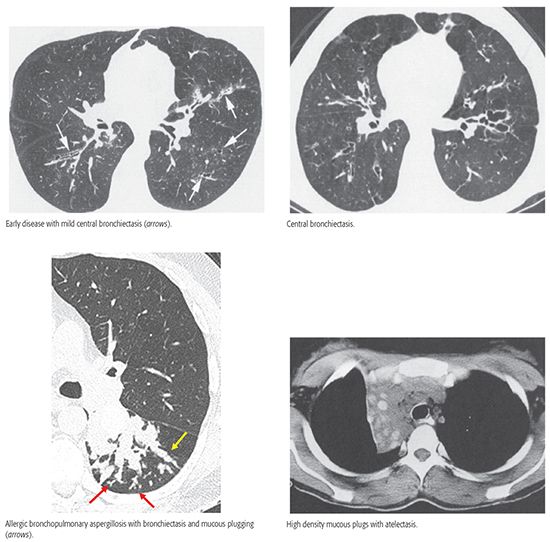
ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS
(See pages 584–586.)
Allergic bronchopulmonary aspergillosis is a syndrome characterized by a hypersensitivity reaction to endobronchial growth of Aspergillus fumigatus and is characterized by eosinophilia, symptoms of asthma, and central or proximal bronchiectasis with mucous impaction and sometimes atelectasis or air trapping. High-attenuation mucous plugs suggest this diagnosis.
HRCT Findings
Central bronchiectasis
Mucous plugging
High-attenuation mucous plugs
Tree-in-bud
Atelectasis
Mosaic perfusion
Air trapping on expiratory scans
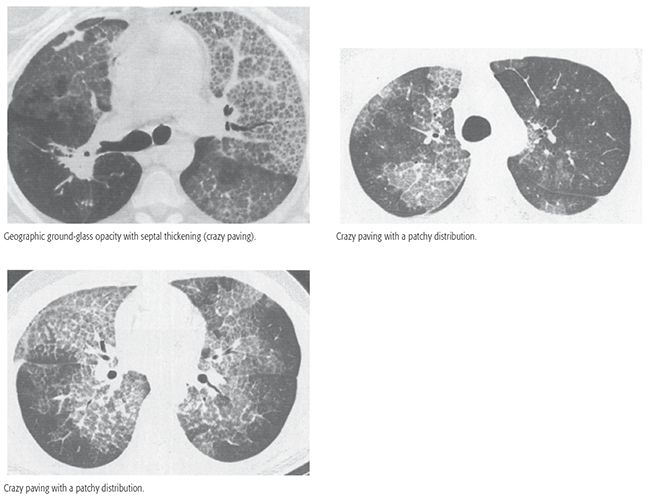
ALVEOLAR PROTEINOSIS (PULMONARY ALVEOLAR PROTEINOSIS)
(See pages 411–416.)
A rare disease associated with the intra-alveolar accumulation of large, foamy macrophages, along with elevated levels of surfactant proteins. It may be congenital, secondary or associated with other diseases, or acquired, also termed idiopathic or autoimmune pulmonary alveolar proteinosis. The acquired form is most common. It is treated using bronchoalveolar lavage. Crazy paving is typical.
HRCT Findings
Patchy ground-glass opacity
Smooth septal thickening in abnormal areas
Crazy paving
Consolidation
Patchy or geographic distribution
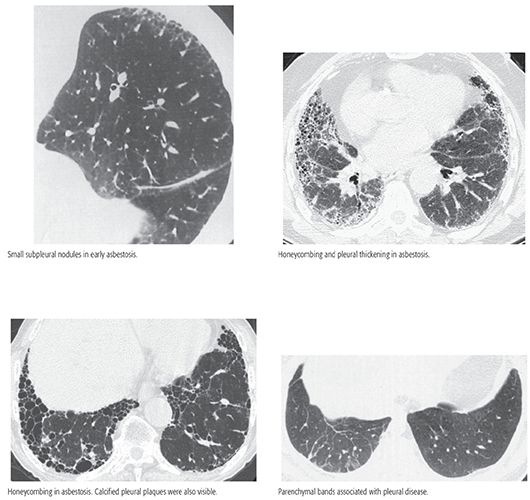
ASBESTOSIS AND ASBESTOS-RELATED DISEASE
(See pages 342–358.)
Asbestosis is pulmonary fibrosis associated with asbestos exposure and asbestos bodies in lung parenchyma. It is typically associated with a usual interstitial pneumonia pattern. Pleural plaques are associated in 90%. Pleural disease may be associated with parenchymal bands or rounded atelectasis.
HRCT Findings
Pleural thickening and plaques
Subpleural dot-like opacities in early disease
Findings of fibrosis
Honeycombing in advanced disease
Subpleural lines
Parenchymal bands in association with pleural thickening
Earliest abnormalities posterior and basal
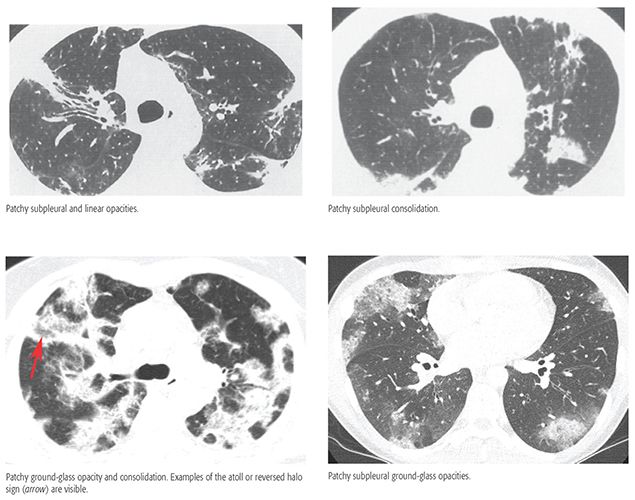
CHRONIC EOSINOPHILIC PNEUMONIA
(See pages 389–391.)
Chronic eosinophilic pneumonia is an idiopathic condition characterized by extensive filling of alveoli by a mixed inflammatory infiltrate consisting primarily of eosinophils. Approximately 50% of patients have a history of asthma. Symptoms are usually present for at least 1 month prior to diagnosis and include dry cough; shortness of breath; and, frequently, fever, weight loss, and malaise. It responds promptly to steroids.
HRCT Findings
Patchy unilateral or bilateral airspace consolidation
Patchy ground-glass opacity
Peripheral and peribronchial distribution
Mid-lung and upper lung predominance
Subpleural lines
Atoll or reversed halo sign in some
Appearance similar to OP
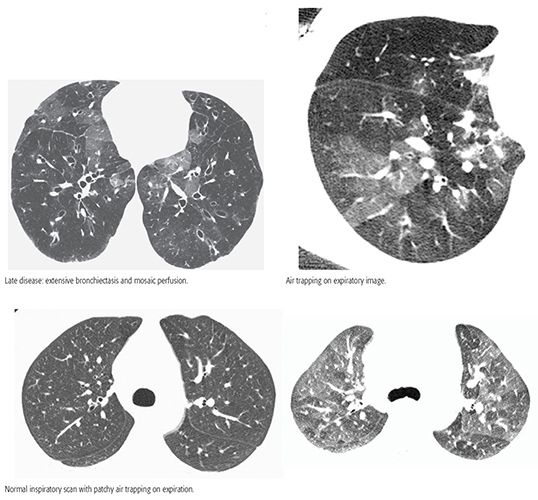
CONSTRICTIVE BRONCHIOLITIS (BRONCHIOLITIS OBLITERANS)
(See page 594, 606–613.)
Constrictive bronchiolitis is defined by the presence of concentric bronchiolar fibrosis, resulting in marked narrowing or obliteration of bronchioles, in the absence of intraluminal granulation tissue polyps or surrounding parenchymal inflammation. Clinically, constrictive bronchiolitis is associated with marked airflow obstruction that is usually not responsive to steroid therapy. It has a variety of causes.
HRCT Findings
Bronchiectasis
Mosaic perfusion, usually patchy on inspiratory scan
Air trapping on expiration, usually patchy
Air trapping on expiration despite normal inspiratory scans
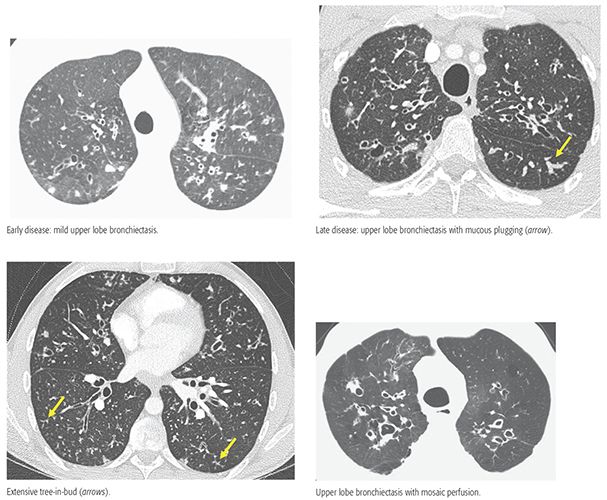
CYSTIC FIBROSIS
(See pages 574–582.)
Cystic fibrosis (CF) results from an autosomal-recessive genetic defect in the structure of the CF transmembrane regulator protein, which leads to abnormal chloride transport across epithelial membranes, decreased mucous clearance and chronic airway infection with bronchiectasis and mucous plugging, and progressive respiratory failure.
HRCT Findings
Bronchiectasis, central bronchi and upper lobes involved in all cases
Bronchial wall thickening, right upper lobe first involved
Mucous plugging
Tree-in-bud
Large lung volumes
Areas of atelectasis
Mosaic perfusion
Air trapping on expiration
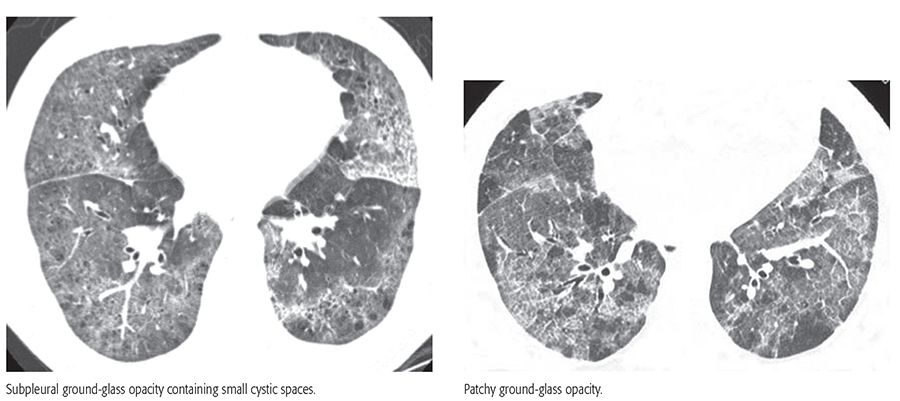
DESQUAMATIVE INTERSTITIAL PNEUMONIA
(See pages 245–248.)
Desquamative interstitial pneumonia (DIP) is an uncommon condition, characterized histologically by the presence of numerous macrophages filling distal airspaces, mild inflammation of the alveolar walls, and minimal fibrosis. It involves the lung in a uniform fashion, but often predominates in the lower lobes. Although listed among the idiopathic interstitial pneumonias, the large majority of patients with DIP are cigarette smokers. DIP is similar to respiratory bronchiolitis-interstitial lung disease, which predominates in relation to bronchioles, and often has an upper lobe predominance.
HRCT Findings
Bilateral, patchy ground-glass opacity
Subpleural and basal predominance in many
Minimal findings of fibrosis (reticulation)
Small cysts in abnormal areas
Air trapping in some patients on expiration
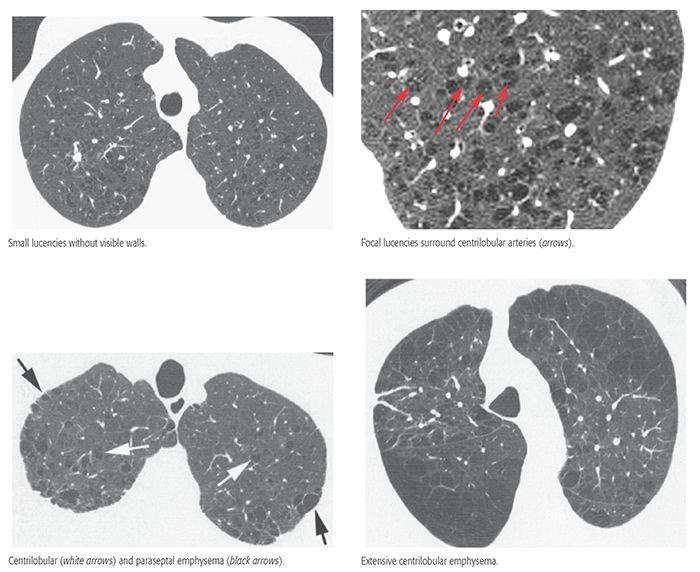
EMPHYSEMA (CENTRILOBULAR)
(See page 518–521.)
Centrilobular emphysema (CLE) is characterized by preferential destruction of alveolar walls in the centers of pulmonary lobules and enlargement of respiratory bronchioles. The process affects the upper lungs more than the lower lungs. Cigarette smoking is the most common cause. CLE may be associated with bullae and paraseptal emphysema.
HRCT Findings
Multiple small, spotty, or centrilobular lucencies
Upper lobe predominance
Lucencies usually lack visible walls in most
Lucencies may be seen to surround centrilobular artery
May be associated with paraseptal emphysema or bullae
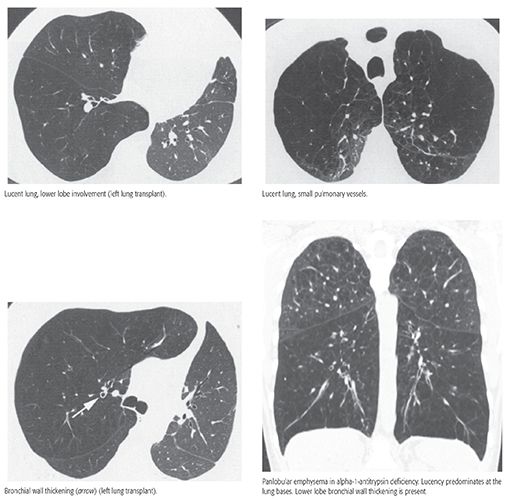
EMPHYSEMA (PANLOBULAR)
(See pages 519–523.)
Panlobular emphysema (PLE) is defined by uniform loss of alveolar septa throughout secondary lobules. Alpha-1-antitrypsin deficiency is the most common cause of PLE, but it also occurs with intravenous injection of crushed methylphenidate (Ritalin) tablets, Swyer-James syndrome, old age, and rarely from cigarette smoking.
HRCT Findings
Lucent lung containing small pulmonary vessels
Diffuse or lower lobe predominance
Focal lucencies and bullae less common than with centrilobular emphysema
Bronchiectasis or bronchial wall thickening in some
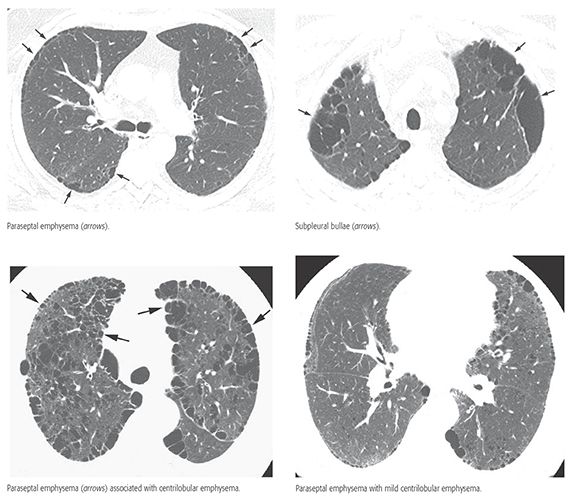
EMPHYSEMA (PARASEPTAL)
(See pages 523–526.)
Paraseptal emphysema results in the presence of subpleural lucencies, which often have very thin walls. Paraseptal emphysema can be seen as an isolated abnormality but is often associated with centrilobular emphysema. Bullae commonly are associated and pneumothorax may result.
HRCT Findings
Multiple, subpleural lucencies in a single layer, usually smaller than 1 cm
Upper lobe predominance
Thin walls are commonly visible
May be associated with centrilobular emphysema or bullae
Associated with pneumothorax
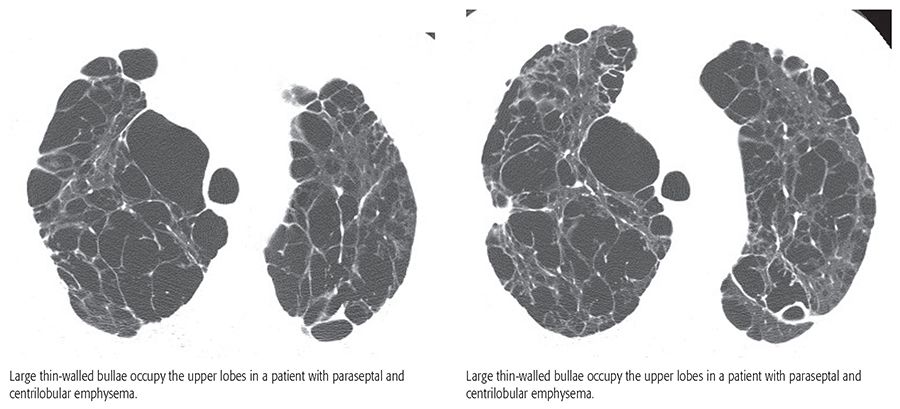
EMPHYSEMA (BULLOUS)
(See pages 526–529.)
Bullous emphysema is characterized primarily by large bullae, defined as sharply demarcated areas of emphysema, measuring 1 cm or more in diameter and possessing a wall less than 1 mm in thickness. Bullous emphysema is typically associated with centrilobular emphysema or paraseptal emphysema.
HRCT Findings
Thin-walled air-filled cysts greater than 1 cm (i.e., bullae)
Cysts share walls
Associated centrilobular or paraseptal emphysema
Upper lobe predominance
Often asymmetrical
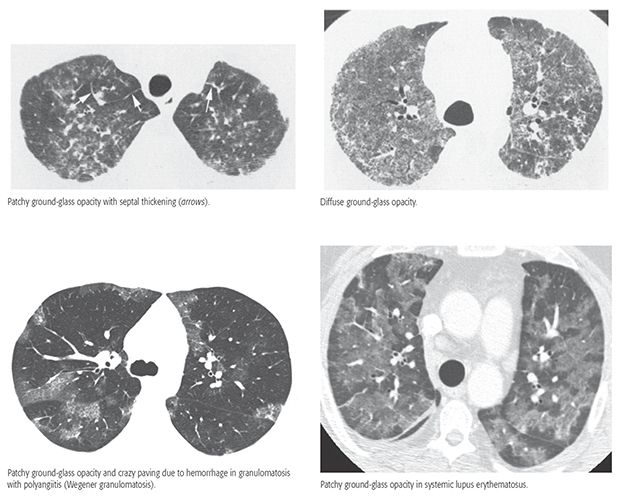
HEMORRHAGE
(See pages 649–654.)
Pulmonary hemorrhage may be diffuse (i.e., diffuse alveolar hemorrhage) or localized, and may be associated with a variety of diseases and syndromes and vasculidities. HRCT findings are usually nonspecific.
HRCT Findings
Ground-glass opacity
Bilateral, patchy, or diffuse
Centrilobular ground-glass opacities
Interlobular septal thickening in some
Crazy paving in some
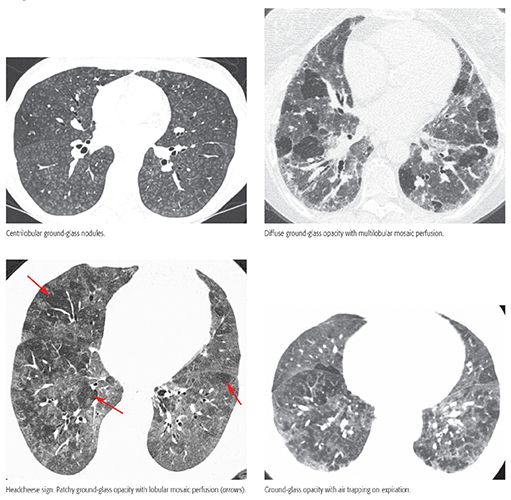
HYPERSENSITIVITY PNEUMONITIS (SUBACUTE)
(See pages 378–383.)
Hypersensitivity pneumonitis is a disease resulting from exposure to a variety of organic antigens, usually presenting in the subacute stage with cough and progressive dyspnea. Histologic findings in the subacute state include an alveolitis, poorly-defined peribronchiolar granulomas, and air trapping related to bronchiolar obstruction. Treatment involves removing the offending antigen or steroid treatment.
HRCT Findings
Patchy or diffuse ground-glass opacity
Small centrilobular ground-glass opacity nodules
Lobular areas of decreased attenuation (mosaic perfusion)
Headcheese sign (combination of ground-glass opacity and patchy mosaic perfusion)
Lobular areas of air trapping on expiratory scans
Diffuse, mid-lung, or upper lung predominance
Findings of fibrosis may be superimposed
HYPERSENSITIVITY PNEUMONITIS (CHRONIC)
(See pages 383–386.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


