Fig. 7.1
A diagrammatic representation of the AR murmur
An early ejection sound is present along with an early diastolic murmur.
Normal S2.
Grade 2/4, low pitch murmur at the mid right sternal border.
S4 gallop.
Test Results
Normal ejection fraction with left ventricular enlargement:
End diastolic dimension: 56 mm.
End systolic dimension 35 mm.
AV: trileaflet (appeared functional bicuspid) with calcified anterior leaflet, and limited mobility.
Severe AR by color flow imaging (Fig. 7.2).
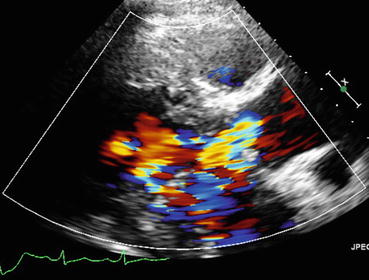
Fig. 7.2
Echocardiogram of the described patient case demonstrating retrograde blood flow across the valve in AR
Eccentric jet onto anterior mitral valve leaflet.
Compressed mitral valve- limited diastolic excursion with anterior mitral valve leaflet fluttering.
Pressure half time ~300 ms (moderate to severe).
Holodiastolic aortic flow reversal.
Clinical Basics
Normal Anatomy
The normal aortic valve is composed of three leaflets with approximately 2 % of the population having two leaflets (“bicuspid valve”).
The AV controls flow from the LV to the aorta and is open during systole. It contributes to the S2 heart sound.
Definition
Aortic regurgitation refers to abnormal retrograde blood flow through the aortic valve during diastole. The abnormal blood flow through the valve causes an increase in LV end-diastolic volume. See Fig. 7.3.
Fig. 7.3
Area in heart producing early diastolic aortic regurgitation murmurs
Etiology
Aortic regurgitation is considered to be a result of aortic root dilation (35 %), congenital defects (20 %), or valvular pathology. Bicuspid aortic valve is the most common congenital cause.
Signs and Symptoms
Most patients are asymptomatic early in the disease and aortic regurgitation is most commonly discovered incidentally. Late stage or progressive symptoms can include angina, dyspnea, and fatigue that signify left ventricular dysfunction and pulmonary venous congestion.
Prevalence
Aortic regurgitation has been found in approximately 0.75 % of patients in the United States [1].
Key Auscultation Features (Fig. 7.4)
Fig. 7.4
Key features of AR auscultation
Diastolic decrescendo murmur at the left upper sternal border which can be accentuated by maneuvers that increase afterload. Auscultation of this murmur at the right upper sternal border is suggestive of aortic root enlargement or displacement. A left lower sternal border location is suggestive of a valvular abnormality.
S1 is soft due to increased left ventricular filling pressure decreasing the force of MV closure.
The presence of an ejection click suggests an etiology of bicuspid valve.
Brief early systolic murmurs can be auscultated due to flow disturbances.
An S3 signifies LV dysfunction, but does not indicate the severity of aortic regurgitation.
Auscultation examples of aortic regurgitation.
Click here to listen to an example of an AR murmur and see an image of the phonocardiogram (Video 7.1).
Click here to listen to an example of mixed AS with AR and see and image of the phonocardiogram (Video 7.2).
Click here to listen to examples of several patients with AR, as described by Dr. W. Proctor Harvey (Video 7.3).
Auscultation Differential Diagnosis
Mitral regurgitation: distinguished by a right ventricular heave and a pansystolic murmur at apex radiating to axilla.
Mitral stenosis: distinguished by a loud S1 with an opening snap and rumbling mid-diastolic murmur.
Aortic stenosis: distinguished by patient presentation of dyspnea, dizziness, syncope, and congestive cardiac failure. Auscultation reveals an ejection systolic murmur that radiates towards carotids with an ejection click.
Pulmonary regurgitation: distinguished by a crescendo-decrescendo diastolic murmur heard at the left upper sternal border which is increased with inspiration.
Arterial-venous fistula- can widen pulse pressure, and can create murmurs in the setting of high venous flow.
Clinical Clues to the Detection of the Lesion
Widened pulse pressure is frequently seen in aortic regurgitation due to the increased LV ejection volume (thereby increasing systolic pressure) and reduced diastolic pressure from the regurgitant volume and the low peripheral resistance.
Potential false positive: Older patients may have increased pulse pressure as a function of reduced arterial compliance.
Potential false negative: Young patients with highly compliant vessels may not show early changes of widened pulse pressure.
Key physical signs that may contribute to accuracy (Table 7.1) include [2]:
Table 7.1
Physical diagnosis signs associated with more accurate detection of AR
Sign< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
