The cause of acute aortic dissection continues to be debated. One school of thought suggests that underlying aortic medial cystic necrosis is the common denominator. The purpose of the present study was to determine if there was loss and, if so, how much loss of medial elastic fibers in the ascending aorta in patients with acute aortic dissection with the entrance tear in the ascending aorta. We examined operatively excised ascending aortas in 69 patients having acute dissection with tears in the ascending aorta. Patients with previous aortotomy, healed dissection, and connective tissue disorders were excluded. The 69 patients’ ages ranged from 31 to 88 years (mean 56); 49 were men and 20 were women. Loss of aortic medial elastic fibers was graded as 0 (no loss), 1+ (trace), 2+ (mild), 3+ (moderate), and 4+ (full thickness loss). Of these 69 patients, 56 (82%) had 0 or 1+ elastic fiber loss; 13 patients (18%), 2+ to 4+ loss including 4 with 2+, 6 with 3+, and 2 with 4+. Nearly all patients (97%) had a history of systemic hypertension and/or had received antihypertensive drug therapy. In conclusion, most patients (82% in this study) having acute aortic dissection with entrance tears in the ascending aorta have normal numbers or only trace loss of aortic medial elastic fibers. Thus, underlying abnormal ascending aortic structure uncommonly precedes acute dissection.
Numerous publications have appeared in the last 50 years describing operative procedures and their results in patients having operative therapy for acute dissection involving the ascending aorta. Far fewer studies have been published on results of examination of the operatively resected portion of the ascending aorta. The present report focuses on aortic medial elastic-fiber structure in 69 patients having portions of the ascending aorta operatively resected because of acute dissection involving the ascending aorta with or without involvement of other portions of the aorta.
Methods
Surgical pathology files of the cardiovascular laboratory—a part of the pathology department of Baylor University Medical Center at Dallas—were searched for patients having operatively resected portions of the ascending aorta with or without excision or repair of the aortic valve for acute dissection involving the ascending aorta with or without involvement of other portions of aorta. From May 1994 through June 2010, a period of 194 months (16.2 years), 119 specimens labeled as aortic dissection were received in the surgical pathology section and each was examined and described by 1 of us (W.C.R.). After the examination and description of the submitted specimen, histologic sections of all aortas were prepared: ≥1 paraffin section was stained by the Movat method. All histologic sections were examined initially by W.C.R. to prepare the surgical pathology report and later, all together, as part of the present report. Total lengths (centimeters) of the sections of the aorta on each Movat-stained slide were measured and recorded.
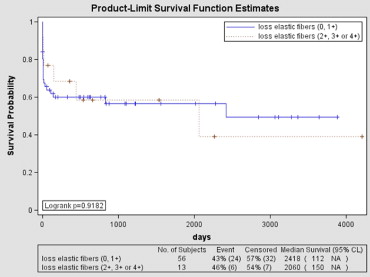
Degree of loss of elastic fibers in the aortic media from examination of the Movat-stained slides was graded 0 to 4+; grade 0 or 1+ represented no loss or minimal loss or mild fragmentation of elastic fibers; grade 4 represented complete loss of elastic fibers in some full-thickness portions of media; grades 2 and 3 were intermediate ( Figure 1 ) .
Ascending aortas in 19 necropsy cases were selected to serve as controls for this study. None had cardiac valve disease or dilated ascending aortas. The 19 ranged in age from 28 to 82 years (mean 61); 10 were women and 9 were men. Twelve had died from cardiac causes (coronary artery disease events in 10, amyloidosis in 1, and lymphocytic myocarditis in 1) and 7 from noncardiac and nonvascular causes. Sections of ascending aorta perpendicular and parallel to the long axis were prepared from each control subject. In each of the 19 cases, 1 section was stained by hematoxylin and eosin, another by Movat stain, and another by elastic-van Gieson methods. Lengths of the aorta examined histologically were measured in centimeters.
Clinical records including admission note and/or discharge summary, echocardiographic and cardiac catheterization reports, and operative records were sought from all patients’ medical charts and/or from the Baylor University Medical Center Apollo cardiovascular database (Apollo Advance C/S 4.2.13, LUMEDX Corp., Oakland, California).
Included in the present study were 69 patients who had resection of portions of the ascending aorta and initiating tears in the ascending aorta. Excluded from this study were 50 patients: 5 who had an acute aortic dissection in the operating room at the time of coronary artery bypass grafting or aortic valve replacement; 4 patients who had acute dissection involving the ascending aorta late postoperatively after coronary artery bypass grafting and/or aortic valve replacement; 6 patients who had a tear in the descending thoracic aorta (isthmic area) and acute retrograde dissection of the ascending aorta; and 35 patients who had healed (chronic) aortic dissection irrespective of the location of the initial aortic entrance site, including 20 patients who had a previous aortotomy of the ascending aorta. Also excluded were patients with genetically mediated conditions such as Marfan syndrome and Loeys-Dietz syndrome. None of the 69 patients included in the present study had a previous aortotomy, and all had dissection entrance sites in the ascending aorta and dissection afterward with operative resection of portions of the ascending aorta.
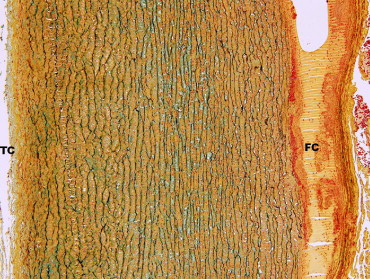
Descriptive statistics (percentage, mean ± SD) were used to describe patients included in the study. A Cox proportional hazards model (without covariates) was used to assess the unadjusted association of loss of medial elastic fibers (2+, 3+, or 4+) and mortality. Unadjusted survival curves and survival estimates were computed using the Kaplan–Meier method.
This study was approved by the institutional review board at Baylor University Medical Center.
Results
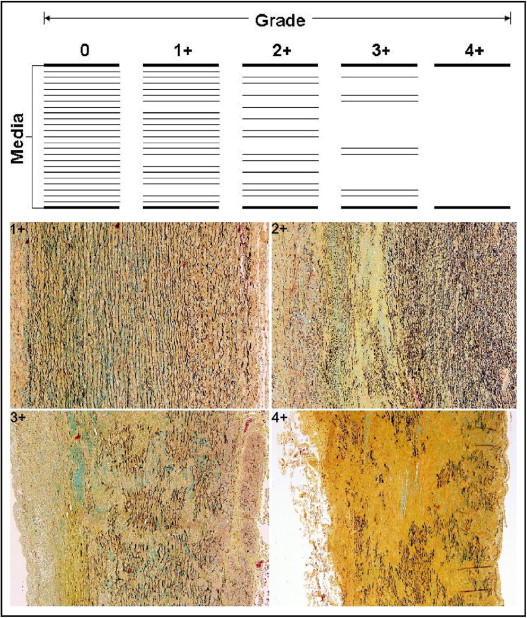
Findings in the 69 patients are presented in Table 1 . Qualitative comparison of degree of loss of medial elastic fibers at the initial examination of the Movat-stained sections to the re-examination of the Movat-stained sections showed only minimal discrepancies: some cases called normal at the initial examination were occasionally called 1+ on re-examination or vice-versa; sections classified as 2+ or 3+ or 4+ initially were classified similarly on re-examination. Photomicrographs of typical acute dissection are shown in Figure 2 .
| Variable | Elastic Fiber Loss | p Value ⁎ | |
|---|---|---|---|
| 0–1+ | 2+–4+ | ||
| (n = 56) | (n = 13) | ||
| Ages (years), range (mean ± SD) [median] | 31–88 (59 ± 14) [60] | 34–66 (45 ± 10) [45] | 0.003 |
| Men | 38 (68%) | 11 (85%) | 0.234 † |
| 31–77 (56 ± 13) [56] | 34–66 (44 ± 9) [44] | ||
| Women | 18 (32%) | 2 (15%) | |
| 43–88 (65 ± 13) [68] | 46, 63 | ||
| Race | 0.381 | ||
| White | 34 (61%) | 10 (77%) | |
| Black | 14 (25%) | 3 (23%) | |
| Hispanic | 4 (7%) | 0 | |
| Other or unclear | 4 (7%) | 0 | |
| Systemic hypertension by history or antihypertension therapy | 51 (91%) | 13 (100%) | 0.268 |
| Previous resection, abdominal aortic aneurysm | 3 (5%) | 0 | 0.397 |
| Body mass index (kg/m 2 ) (n = 65) | 18.9–46.4 (28.9 ± 6.8) [27.7] | 20.9–42.1 (29.5 ± 6.9) [28.1] | 0.947 |
| Men | 19.8–46.4 (29.8 ± 7.0) [28.3] | 20.9–42.1 (30.7 ± 7.0) [29.6] | |
| ≤25 | 9 (26%) | 3 (30%) | |
| 26–30 | 14 (40%) | 3 (30%) | |
| >30 | 12 (34%) | 4 (40%) | |
| Women | 18.9–44.7 (27.1 ± 6.4) [26.8] | 21, 26.6 | |
| ≤25 | 7 (41%) | 1 (50%) | |
| 26–30 | 6 (35%) | 1 (50%) | |
| >30 | 4 (24%) | 0 | |
| Aortic valve (n = 49) | 0.797 | ||
| Replaced | 20 (54%) | 7 (58%) | |
| “Repaired” | 17 (45%) | 5 (41%) | |
| Number aortic valve cusps (n = 56) | 0.3559 | ||
| 2 | 3 (7%) | 2 (15%) | |
| 3 | 40 (93%) | 11 (85%) | |
| Weight (g) of excised aortic valves (n = 17) | 0.38–1.75 (0.77 ± 0.43) [0.67] | 0.39–0.93 (0.68 ± 0.20) [0.69] | 0.675 |
| Bicuspid | 0.53, 1.52, 1.75 | 0.77 | — |
| Tricuspid | 0.38–0.81 (0.60 ± 0.15) [0.66] | 0.39–0.93 (0.66 ± 0.22) [0.66] | 0.587 |
| Coronary bypass | 7 ‡ (13%) | 0 | 0.181 |
| Weight of excised ascending aorta (g) (n = 66) | 0.4–59.5 (16.59 ± 11.52) [13.4] | 6.14–30 (17.37 ± 9.73) [14.9] | 0.834 |
| With bicuspid valve | 27.5–51 (35.50 ± 7.75) [28] | 25.05 | — |
| With tricuspid valve | 0.4–59.5 (15.42 ± 11.30) [13.2] | 6.14–30 (16.60 ± 9.73) [14.6] | 0.764 |
| Lengths (cm) of ascending aorta examined | 4–19 (10 ± 4) [10.5] | 4–21 (14 ± 5) [14] | 0.063 |
| Men | 4–19 (10 ± 4) [10.5] | 4–21 (14 ± 5) [14] | 0.057 |
| Women | 6–16 (11 ± 3) [12] | 8, 17 | 0.824 |
| Intimal plaque, ascending aorta | 7 (13%) | 2 (15%) | 0.785 |
| Died: days after operation (n = 30) | 0.115 | ||
| ≤30 | 19 (79%) | 3 (50%) | |
| 0–28 (5 ± 7) [3] | 2, 8, 13 | ||
| >30 | 5 (21%) | 3 (50%) | |
| 58–2,418 (712 ± 1,004) [141] | 150, 445, 2,060 | ||
| Days in hospital postoperatively in patients living >30days | 4–48 (14 ± 11) [10] | 5–63 (16 ± 18) [10] | 0.548 |
⁎ The p values accounted for multiple comparisons.
† The p value accounts for gender versus elastic fiber loss comparison.
‡ One of the 7 patients had bypass because of coronary artery disease; the other 6 had bypass because the dissection or tear involved the left and/or right coronary ostia.
Examination of Movat-stained and elastic-van Gieson–stained sections of aorta in the 19 control subjects disclosed no discrepancies in degree of medial elastic fiber loss or lack thereof between the 2 stains in any subject. Degree of elastic fiber loss in all 19 control subjects was zero or 1+. Specifically, no subject had 2+, 3+, or 4+ elastic fiber loss. Lengths of ascending aorta examined from the Movat-stained sections ranged from 4 to 16 cm (mean 10).
At the time of the operation the mean age of the 49 men was 53 years and that of the 20 women was 64 years ( Table 1 ). Nearly 2/3 were white. Thirty of the 69 patients (43%) have died: 22 (32%) within 30 days of the operative procedure and 8 (12%) >30 days later. Of the 47 surviving >30 days, stay in the hospital after operation ranged from 4 to 63 days (mean 15, median 10). By history, 92% of patients (59 of 64) had systemic hypertension, 70% (40/57) were on antihypertensive therapy, and 97% (64/66) had a history of hypertension or were on antihypertensive therapy. Body mass indexes (BMIs; kilograms per square meter) ranged from 18.9 to 46.4 (mean 29.0, median 27.7) and 20 of 64 patients (31%) had BMI <25 kg/m 2 . Only 1 of the 69 patients was documented to have atherosclerotic coronary artery narrowing. Seven patients, however, had coronary bypass, 6 because of dissection or tears involving the origin of the right (5 patients) or left main (1 patient) coronary artery. The aortic valve was replaced in 27 patients (39%) and “repaired” in another 22 patients (32%). At least 5 patients were described at operation or by the surgical pathologist (W.C.R.) as having congenitally bicuspid aortic valves. The operatively excised 3-cuspid valves (13 patients) weighed 0.38 to 0.93 g (mean 0.62), and the congenitally bicuspid valves (4 patients) weighed from 0.53 to 1.75 g (mean 1.14). The aortic valve was replaced with a bioprosthesis in 3 patients, a mechanical prosthesis in 19, and a homograft in 5 patients ( Table 2 ).
| Died Postoperatively | Concomitant AVR Using | ||||||
|---|---|---|---|---|---|---|---|
| Mechanical Prosthesis | Bioprosthesis | Homograft | Any Type of Substitute Valve | Concomitant AV Repair | Without AVR or Repair | Total | |
| (n = 19) | (n = 3) | (n = 5) | (n = 27) | (n = 22) | (n = 20) | (n = 69) | |
| ≤30 days | 5 | 2 | 3 | 10 | 5 | 7 | 22 (32%) |
| >30 days | 3 | 0 | 1 | 4 | 2 | 2 | 8 (12%) |
| Total | 8 (42%) | 2 (67%) | 4 (80%) | 14 (52%) | 7 (32%) | 9 (45%) | 30 (44%) |
Operatively excised aortas ranged in weight from 0.4 to 59 g (mean 17, median 14) and in 50 patients (76%) weighed >10 g. Lengths of ascending aorta examined in the Movat-stained slides (those stained for elastic fibers) ranged from 4 to 21 cm (mean 11, median 12). Losses of elastic fibers in the media of sections of ascending aorta were 0 (24 patients, 35%), 1+ (32 patients, 46%), 2+ (5 patients, 7%), 3+ (6 patients, 9%), and 4+ (2 patients, 3%). Atherosclerotic plaques were present in the ascending aorta in 9 patients (13%). Of the 5 patients with bicuspid aortic valves, aortic medial elastic fiber loss was 0 in 1, 1+ in 2, and 3+ in 2. A typical example of aortic dissection is shown in Figure 2 .
Unadjusted association between loss of medial elastic fibers and mortality was not significant (hazard ratio 0.95, 95% confidence interval 0.39 to 2.34, log-rank p = 0.91). Survival curves are shown in Figure 3 . Survival was assessed by the Social Security Death Index.