Anatomy of Electrophysiology: Introduction
Rapid advances have been made in electrophysiologic mapping, imaging, use of catheter ablations for drug refractory arrhythmias, and transcatheter implantation of pacing leads. A better understanding of cardiac anatomy is essential to make further progress, especially in fine-tuning interventional techniques and in developing computer models of arrhythmias. To this end, describing cardiac structures in attitudinal perspective1 is much more useful to the clinical electrophysiologist than the conventional approach2 of describing the heart as if it is standing on its apex and rotated with right and left heart chambers side by side. This chapter on cardiac anatomy highlights features of particular relevance to electrophysiologists.
The Heart in the Chest
For the clinician the heart must be viewed in the context of its location and relationship to surrounding structures. The frontal silhouette of the heart is nearly trapezoidal. The right border of the heart is more or less a vertical line just to the right of the sternum. It is formed exclusively by the right atrium, with the superior and inferior caval veins joining at its upper and lower margins. The inferior border lying horizontally on the diaphragm is marked by the right ventricle. The sloping left border is made up of the left ventricle and, as it merges with the upper border, the silhouette is formed by the pulmonary trunk. The upper border of the silhouette is made by the arterial trunks with the pulmonary valve leftward and superiorly situated relative to the aortic valve. On the frontal silhouette, the left atrium is barely seen; only its appendage curling round the edge of the pulmonary trunk is visible. Thus, the left atrium is the most posteriorly situated cardiac chamber. When viewed in situ, the proximity of the esophagus to the posterior wall of the left atrium is clear (Fig. 37–1). This spatial relationship is crucial to ablationists in order to reduce the risk of the post-procedural complication of atrioesophageal fistula.3,4
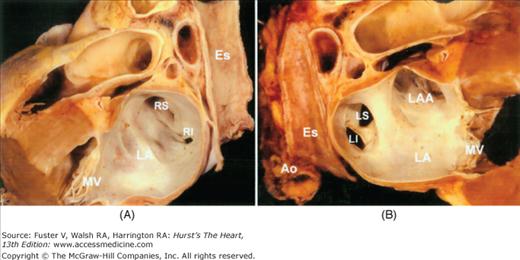
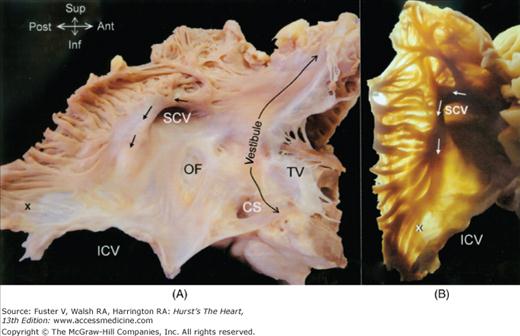
Figure 37–1
Two halves of the same specimen bisected longitudinally to show the relationship between the posterior wall of the left atrium and the esophagus. Ao, aorta; Es, esophagus; LA, left atrium; LAA, left atrial appendage; LI, left inferior pulmonary vein; LS, left superior pulmonary vein; MV, mitral valve; RI, right inferior pulmonary vein; RS, right superior pulmonary vein.
The heart is enclosed in a fibrous sac, the pericardium, which separates the surface of the heart from adjacent structures. The mediastinal pleura is the outermost lining of the fibrous pericardium. Within the fibrous pericardium there is a thinner double-layered membrane, the serous pericardium. One layer of the serous pericardium is fused to the inner surface of the fibrous pericardium while the other layer lines the outer surface of the heart as the epicardium. The pericardial cavity then is the space between the layers of the serous pericardium. Two recesses are found within the pericardial cavity. One is the transverse sinus lying between the back of the arterial trunks and the front of the atrial chambers. Another is the oblique sinus lying behind the left atrium and is limited by the right pulmonary veins and the inferior caval vein to the right side and by the left pulmonary veins to the left side.5,6 Understanding the topography of surrounding structures is important also for those using intra-pericardial catheter techniques. For instance, the descending aorta close to the left inferior pulmonary vein is at risk of damage.
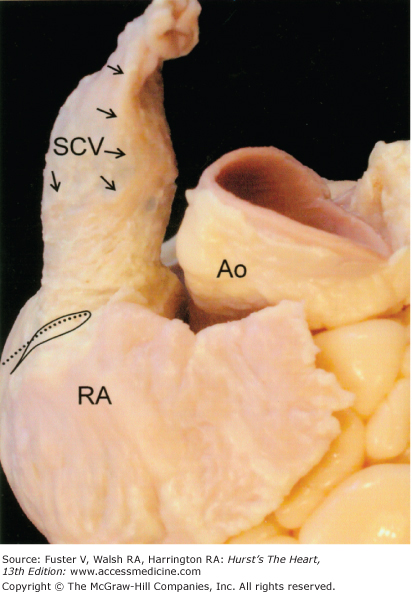
On the surface of the pericardial sac descends the phrenic nerves and their accompanying pericardiophrenic arteries which are branches from the internal mammary artery. The right phrenic nerve descends vertically along the right anterolateral surface of the superior caval vein to be related to the right aspect of the intercaval atrial wall, and in front of the root of the lung, to reach the diaphragm adjacent to the lateral border of the entrance of the inferior caval vein.7 Along the way, the right phrenic nerve can be less than 2 mm from the anterior wall of the right superior pulmonary vein (Fig. 37–2A).7 The left phrenic nerve descends on the left side close to the aortic arch and onto the pericardium over the left atrial appendage and the left ventricle. It takes one of two courses over the left ventricle that takes it either over the anterior surface or leftward over the obtuse margin. The latter course is close to the lateral vein or left obtuse marginal vein (Fig. 37–2B).7,8
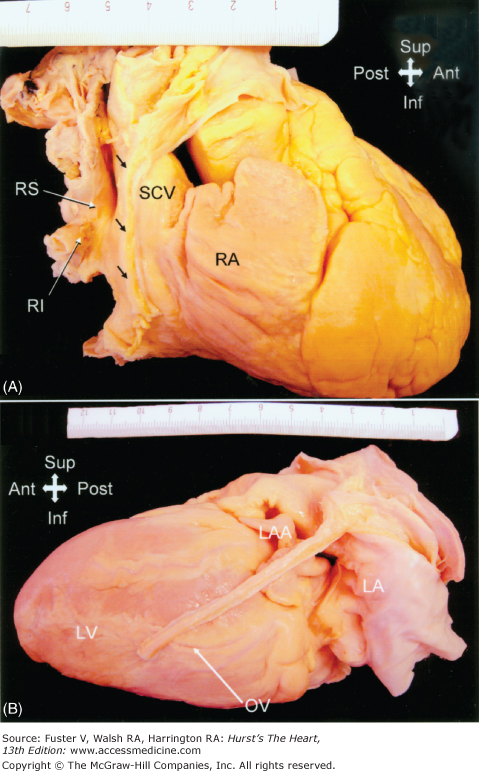
Figure 37–2
A. The right phrenic nerve (arrows) descends along the pericardium, in close proximity to the right pulmonary veins as they enter the left atrium. B. The descent of the left phrenic nerve is either related to the great cardiac vein and anterior descending coronary artery or, as in this specimen, over the course of the obtuse marginal vein. Abbreviations as before, and OV, obtuse vein; RA, right atrium; SCV, superior caval vein.
Location of Atriums
Viewed from the front, the cavity of the right atrium is right and anterior, while the left atrium is situated to the left and mainly posteriorly. The anterior wall of the left atrium lies just behind the transverse pericardial sinus, while its posterior wall is just in front of the tracheal bifurcation and the esophagus. In man, the right superior pulmonary vein passes posterior to the superior caval vein, with the right inferior vein posterior to the venous sinus of the right atrium (Fig. 37–3A).
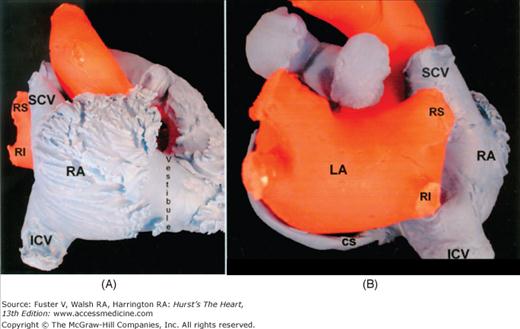
Figure 37–3
A. A view of the endocast from the right shows the characteristically extensive pectinate muscles of the right atrial wall contrasting with the smooth vestibule. The right superior pulmonary vein is posterior to the superior caval vein. B. The endocast viewed from the back shows the right pulmonary veins passing behind the superior caval vein and the intercaval area. The coronary sinus is inferior to the left atrium. Abbreviations as before, and, CS, coronary sinus; ICV, inferior caval vein.
The atrial septum, best appreciated in transverse section, runs obliquely from the front extending backwards and to the right. The posterior part of the left atrium receives the pulmonary veins. The orifices of the left pulmonary veins are more superiorly located than those of the right pulmonary veins. In human it is most common to find two orifices on each side. Sometimes two veins of one, or both, sides are united prior to their entry to the atrium.9 In others, an additional vein is found, more frequently on the right side. Related posteriorly and inferiorly to the left atrium is the coronary sinus, which is the continuation of the great cardiac vein (Fig. 37–3B). The oblique vein (of Marshall) passes from superiorly, between the left atrial appendage and the left superior pulmonary vein, along the posteroinferior atrial wall to join the coronary sinus. This vein is obliterated in the majority of individuals.
The right atrium is best considered in terms of three components: the appendage, the venous part, the vestibule.10 A fourth component, the septum, is shared by the two atriums and will be discussed in a separate section. (see The Atrial Septum and Interatrial Connections) From the epicardial aspect, the right atrium is dominated by its large, triangular-shaped appendage, which is extends anteriorly and laterally. Usually, a fat-filled groove (sulcus terminalis) corresponding internally to the terminal crest (crista terminalis) can be seen along the lateral wall demarcating the junction between appendage and venous components. The sinus node is located subepicardially in this groove, close to the superior cavoatrial junction.11,12 Right atrial musculature often extends a short distance onto the adventitial/epicardial side of the wall of the superior caval vein (Fig. 37–4), but muscular extension surrounding the entrance of the inferior caval vein is less common.
Arising from the terminal crest, pectinate muscles spread throughout the entire wall of the appendage, reaching to the lateral and inferior walls of the atrium (Fig. 37–5). In between the ridges of pectinate muscles, the atrial wall is very thin, almost parchment-like in cases. On the endocardial aspect, the branching and overlapping arrangement of the pectinate muscles is clearly visible. This arrangement may play a role in initiating intra-atrial reentry.13 Although extensively arranged, the pectinate muscles never reach the orifice of the tricuspid valve. Always, a smooth muscular rim, the vestibule, surrounds the valvar orifice, with the musculature inserting into the valvar leaflets (see Fig. 37–5).
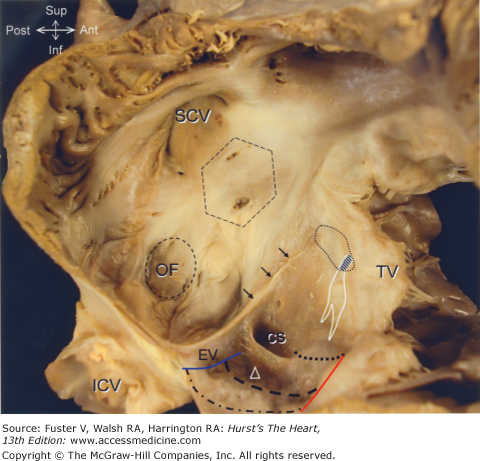
Figure 37–5
A. The parietal wall of the right atrium has been cut and deflected posteriorly to show the terminal crest (arrows). X indicates the distal ramifications of the terminal crest that lead into the flutter (cavotricuspid) isthmus. B. A similar display with transillumination reveals the thin areas in between the pectinate muscles, at the inferior isthmus, and the posteroinferior part of the intercaval atrial wall. Abbreviations as before, and, TV, tricuspid valve.
The venous component is also characterized by smooth walls. The division between venous and rough zones is marked by the terminal crest. This muscular bundle begins on the upper part of the medial wall, turns laterally in front of the orifice of the superior caval vein to descend obliquely along the lateral wall. Its terminal portion is indistinct, as it divides into a variable number of smaller bundles that continue toward the vestibule and the orifice of the inferior caval vein, feeding into the area of the “flutter” (cavotricuspid) isthmus.14 The eustachian valve which guards the entrance of the inferior caval vein is also variably developed. Usually it is a triangular flap of fibrous or fibromuscular tissue that inserts medially to the eustachian ridge, or sinus septum, which is the border between the oval fossa and the coronary sinus (Fig. 37–6). In some cases, the valve is particular large and muscular, posing an obstacle to passage of catheters from the inferior caval vein to the inferior part of the right atrium. Occasionally, the valve is perforated, or takes the form of a delicate filigree, sometimes described as a Chiari network. The free border of the eustachian valve continues as a tendon that runs in the musculature of the sinus septum (eustachian ridge).15 It is one of the borders of the triangle (of Koch) that is the right atrial landmark for determining the location of the atrioventricular node (see Fig. 37–6).12,16,17 The anterior border of Koch triangle is marked by the hinge of the septal leaflet of the tricuspid valve. Superiorly, marking the apex of the triangle, is the central fibrous body through which the conduction system penetrates as the bundle of His. The inferior border of the triangle is the orifice of the coronary sinus together with the vestibule immediately anterior to it. This vestibular portion between the coronary sinus os and tricuspid valve, also known as the paraseptal isthmus (see Fig. 37–6), is the area often targeted for ablation of the slow pathway in atrioventricular nodal reentrant tachycardia. Inferior extensions of the atrioventricular node have been observed in this area (see Fig. 37–6). The so-called fast pathway corresponds to the area of musculature close to the apex of the triangle of Koch.18,19
Figure 37–6
Simulating a right anterior oblique projection, the right atrium is opened to show the septal aspect that appears extensive but the area marked by the hexagon is not septal. Termed the aortic mound, it is the anterior wall of the right atrium that abuts the non- and right coronary aortic sinuses. The true septum is limited to the valve of the oval foramen (OF) and its immediate muscular rim
The triangle of Koch is delineated posteriorly by the tendon of Todaro (arrows) running in the eustachian ridge, anteriorly by the hinge line of the septal leaflet of the tricuspid valve, and inferiorly by the coronary sinus. The apex of the triangle is marked by the central fibrous body (dotted shape) through which the atrioventricular conduction bundle penetrates (hatched). The atrioventricular node and its inferior extensions are depicted by the white shape. The cavotricuspid isthmus is bordered posteriorly by the eustachian valve (blue line) and anteriorly by the tricuspid valve (red line). Within this area are marked three isthmuses: paraseptal isthmus (dots), inferior or central flutter isthmus (dashes), and inferolateral isthmus (dots and dashes). The inferior isthmus passes through the sinus of Keith (triangle). The coronary sinus is guarded by a crescentic thebesian valve. Abbreviations as before, and ER, eustachian ridge; EV, eustachian valve.
A small crescentic flap, the thebesian valve, usually guards the orifice of the coronary sinus.20 Frequently, the crescentic valve is fenestrated. Occasionally, the orifice is totally covered by a fenestrated valve but an imperforate valve is very rare.21 The atrial wall inferior to the orifice of the coronary sinus is usually pouch-like, and is often described as the sinus of Keith, or the sub-eustachian sinus. The area between the inferior caval vein and the tricuspid valve (see Fig. 37–6) corresponds to the isthmus of slow conduction in the circuit of common (typical) atrial flutter and is also described as the cavotricuspid isthmus.13,22 The quadrilateral-shaped isthmus has three morphologic components bordered anteriorly by the hinge of the tricuspid valve and posteriorly by the eustachian valve.14 The posterior component is mainly fibrous whereas the anterior component is the musculature of the atrial vestibule and has a smooth endocardial surface. In the middle is a zone of muscular trabeculations representing the distal ramifications of the terminal crest which are separated by variable extents of thin atrial wall composed mainly of fibrous tissue (see Fig. 37–5). Compared to the inferolateral and paraseptal isthmuses (see Fig. 37–6), the inferior isthmus (also termed the central isthmus) appears most appropriate for ablationists to target on account of it being further from the compact atrioventricular node and is shorter than the inferolateral isthmus.23
Accessing the left atrium from the right requires an appreciation of the extent of the true atrial septum (see Fig. 37–6). Although a right anterior oblique view of the septal aspect as seen from the right atrium suggests an extensive area to be septal, this is not the case if the septum is defined as a partition that separates one cardiac chamber from another and crossing it will not go outside the heart. The musculature that gives the impression of an extensive anterior septal wall is the anteromedial wall of the atrium lying behind the aorta through the transverse pericardial sinus (see Fig. 37–6). The superior rim as demonstrated in a “four-chamber” section is then the infolded wall between the superior caval vein and the right pulmonary veins (Fig. 37–7). Significantly, the folded rim is not a septal area. Enclosed within the fold is epicardial fat. The left aspect of the atrial septum lacks the crater-like feature of the right side. The valve itself is usually fibromuscular. From the right atrium, the leftward part of the muscular fold apposing the valve continues into the musculature of the left atrial wall (see Fig. 37–7).
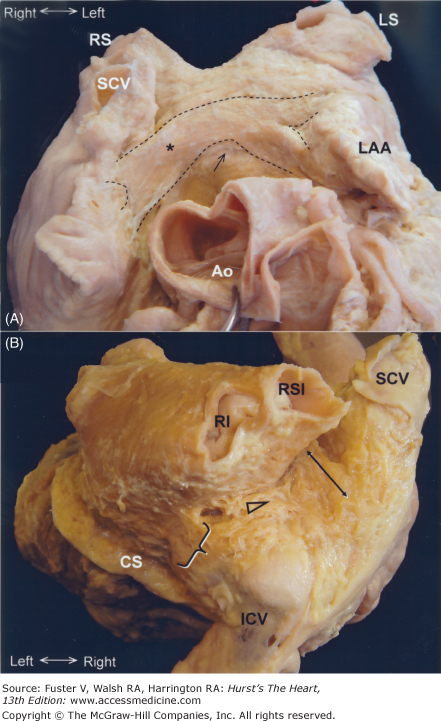
Figure 37–7
A long axis section through the heart profiles the cardiac septum to show the thin valve of the oval foramen (open arrow) on the left atrial side and the muscular rim on the right atrial side. The cut reveals the infolding of the right atrial wall at the superior rim that is filled with epicardial fat (asterisk) to form the interatrial groove. At the ventricular septum, the leaflets of the tricuspid and mitral valves are hinged at different levels (small arrows) producing offset between the right and left atrioventricular junctions. Thus, the vestibule of the right atrium overlies the ventricular septum. Abbreviations as before.
The true septum that interventionalists can cross safely is limited to the flap valve of the oval fossa and the immediate muscular rim that surrounds it on the right atrial aspect (see Fig. 37–7). The valve of the oval foramen can be perforated or crossed without risk of exiting the heart or damaging the arterial supply to the sinus node. Most hearts have well defined muscular rim on the right atrial aspect allowing the operator to “feel” the “jump” from firm muscular rim to tenting of the thin valve with the catheter for safe transseptal puncture. Importantly, nearly one-fifth of hearts have little change in contour and the valve is thicker making it difficult to identify the fossa.24
In approximately one-fourth of normal hearts, there is probe patency of the oval fossa, even though on the left atrial side the valve is large enough to overlap the rim. This is because the adhesion of the valve to the rim is incomplete, leaving a gap usually in the anterosuperior margin corresponding to a C-shaped mark in the left atrial side just behind the anterior atrial wall (Fig. 37–8). The gap in adhesion allows a probe, or catheter, in the right atrium to slip between the rim and the valve into the left atrial chamber. A catheter lodged in this crevice will have its tip directed toward the anterior wall of the left atrium. This part of the wall, just inferior to Bachmann bundle, can be very thin (Fig. 37–9; see also Fig. 37–8). Exiting the heart here leads to the transverse pericardial sinus and, anteriorly, the aortic root.
Figure 37–8
A. Displayed in right anterior oblique view, the anterocephalad margin (open arrow) of this oval foramen will allow a probe to pass into the left atrium behind. B. The left atrial view of the same heart shows the crevice through which the probe will exit and its proximity to the thin part of the left atrial wall anteriorly (open arrow). Abbreviations as before.
Figure 37–9
A. The aortic root is retracted forward to show the anterior wall of the atriums. Bachmann bundle (between broken lines) is displayed crossing the anterior aspect of the interatrial groove (asterisk). The arrow indicates a thin area of the anterior left atrial wall that is frequently found inferior to Bachmann bundle. This site corresponds to the thin area indicated on Fig. 37–8B. Abbreviations as before. B. A heart tilted forward and viewed from the back shows muscle bridges in addition to Bachmann bundle. A muscle bundle (double-headed arrow) connects the anterior wall of the left atrium with the posterior right atrial wall inferior to the superior caval vein. Further bridges are present posteriorly and inferiorly (triangle and brace). Abbreviations as before.
Muscular continuity between atriums peripheral to the septum is frequently found as bridges in the subepicardium.9,10 The most prominent interatrial bridge is Bachmann bundle (see Fig. 37–9). This is a broad muscular band that runs in the subepicardium connecting the anterior right atrial wall of the superior cavoatrial junction with the anterior wall of the left atrium. The muscular fibres in Bachmann bundle, as in the terminal crest, are well-aligned. Multiple smaller interatrial bridges are frequently present, giving the potential for macroreentry. Some connect the muscular sleeves of the right pulmonary veins and the superior caval vein to the left atrium.9,10 Posterior and inferior bridges joining the left atrium to the intercaval area on the right provide the potential for posterior break through of sinus impulse (see Fig. 38–9).25 Inferiorly, further muscular bridges from the left atrial wall often overlie and run into the wall of the coronary sinus.9 Fine bridges connecting the remnant of the vein of Marshall to the left atrium have also been demonstrated.26
As with the right atrium, the left atrium has three components and shares its septum. The atrial appendage is characteristically a small fingerlike cul-de-sac in human hearts where thrombi may form.27 Owing to its tubular shape, its junction with the left atrium is narrow and fairly well defined. Virtually all the pectinate muscles in the left atrium are confined within the appendage. The lumen of the appendage is lined by a complicated network of muscular ridges and intervening membranes that form its wall. Its tip can be directed anteriorly overlying the pulmonary trunk, superiorly behind the arterial pedicle, or posteriorly. When its tip is directed anteriorly, the body of the appendage usually also overlies the main stem of the left coronary artery. The remnant of the vein of Marshall runs on the lateral epicardial aspect of the neck of the appendage, anterior to the left pulmonary veins (Fig. 37–10), in a fold of the atrial wall known as the left atrial ridge. The course of the coronary sinus is related to the inferior aspect of the left atrial wall but it is not immediately adjacent to the hinge line of the leaflets of the mitral valve. In the adult heart, it courses some 6 to 10 mm or more proximally.
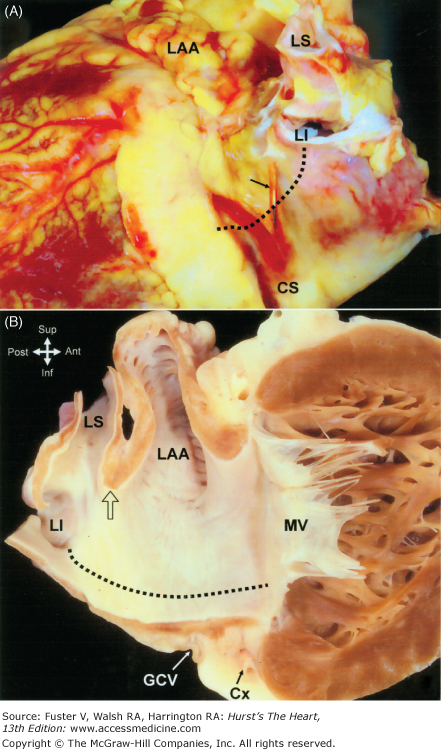
Figure 37–10
A. The heart viewed from the left and inferior aspect shows a small remnant of the vein of Marshall (arrow) descending along the atrial wall in between the left atrial appendage and the left pulmonary veins to enter the coronary sinus. The left atrial isthmus between the left inferior pulmonary vein and the mitral valve is indicated by the dotted line.
B. The long axis cut through the left atrium and left ventricle shows the orifices of the left pulmonary veins and the left atrial isthmus (dotted line). Note the narrow fold (arrow) between the os of the left atrial appendage and the orifice of the left superior pulmonary vein in the heart. It may be challenging to keep the ablation catheter stable along this narrow fold without dropping inadvertently into the vein or the appendage. Abbreviations as before, and GCV, great cardiac vein.
The venous component receives the pulmonary veins and the vestibular component leads to the mitral valve. There are no surface anatomical landmarks to separate the vestibule from the pulmonary venous component although frequently a few pits or crevices are seen in the inferior wall at the border zone. These have very thin walls and may be encountered when constructing ablation lines along the so-called left atrial isthmus (see Fig. 37–10) to link the orifice of the left inferior pulmonary vein to the mitral annulus.28,29 Seemingly uniform, the left atrial walls are composed of one to three or more overlapping “layers” of differently aligned myocardial strands, with marked regional variations in thickness.9,30,31 The area of the anterior wall just behind the aorta is usually thin, whereas the superior wall, or dome, and the inter pulmonary wall are thicker but tends to become thinner toward the left pulmonary veins.
The orifices of the right pulmonary veins are directly adjacent to the plane of the atrial septum (see Fig. 37–7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree