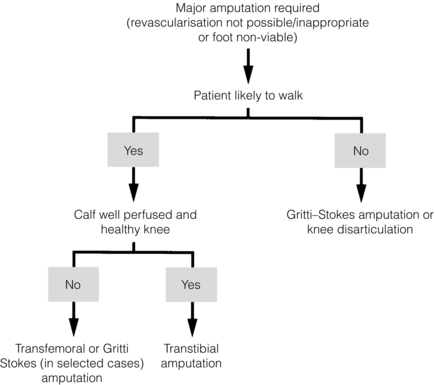
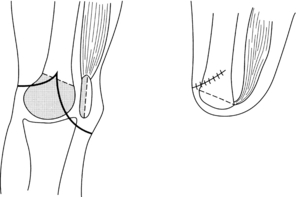
6 Peripheral arterial occlusive disease accounts for the vast majority of lower limb amputations in westernised societies. More than 80% of all amputations carried out in the UK are due to vascular disease but an increasing proportion have diabetes mellitus.1 The overall risk of amputation is six times higher in insulin-dependent people with diabetes compared with non-insulin-dependent people with diabetes. A global study group also reported a marked difference in the incidence of amputation between 10 centres in six different countries. Rates were highest in the North American and northern European centres and lowest in Spain, Taiwan and Japan. In the Navajo population, a very high prevalence of diabetes was thought to be the explanation for their high amputation rates.2 The National Amputee Statistical Database for the UK reported that dysvascularity is the most common reason for referral to prosthetic services centres following a lower limb amputation, accounting for 70% of all lower limb referrals in 2006–7.3 In this group referred to the prosthetic centres in the UK, 53% were transtibial and 39% were transfemoral amputees. In this 1-year period there were a total of 4957 referrals to Prosthetic Services in the UK, of which 4574 were following lower limb amputation (92% of the total).3 There is some evidence that the impact of modern vascular surgery may reduce the incidence of amputation.4 The Danish National Amputation Register has demonstrated a 27% fall in the number of major amputations due to peripheral vascular disease in the decade 1980–90. This decline was attributed to the increased use of infrainguinal bypass operations.5 A paper from Finland also reported that it was possible to reduce amputation rates with an aggressive reconstruction policy in critical limb ischaemia.6 However, the West Coast Vascular Surgeons Study Group in Sweden failed to demonstrate a negative correlation between amputation and revascularisation rates.7 Survival rates after an amputation depend upon the cause of the amputation rather than the amputation itself. Those who have amputations following trauma tend to have good long-term survival, but those from vascular disease (including diabetes) face a 30-day mortality rate reported to be between 9% and 15% and a long-term survival rate of 60% at 1 year, 42% at 3 years and 35–45% at 5 years.8 Of people with diabetes who have lower limb amputation, up to 55% will require amputation of the second leg within 2–3 years.9 The decision to perform amputation seems straightforward where there is extensive tissue loss or no reasonable prospect of revascularisation. However, the precise role of amputation in the management of critical limb ischaemia remains controversial. If it is predicted that vascular reconstruction is likely to be unsuccessful, then primary amputation perhaps offers the best outcome in terms of quality of life and cost benefit.10 Chapter 3 discusses the treatment of chronic lower limb ischaemia and covers these issues of economics and quality of life in more detail. Where patients with critical limb ischaemia also have coexisting disabilities or other medical conditions that would render them unable to make use of a salvageable limb, then primary amputation with appropriate rehabilitation offers the best option. Examples of such patients include those with severe dementia, dense hemiplegia or spinal paralysis, severe arthritis and severe cardiorespiratory disease. In general terms, the more proximal the level of amputation, the more difficult it will be for the patient to achieve independent walking. Therefore, the more distal the amputation site, the better the rehabilitation potential for walking, as this preserves more joints and hence more control of the prosthesis. Figure 6.1 is an algorithm dealing with level selection. Except in people with diabetes with good foot pulses (see Chapter 7), local amputation of single or multiple toes generally does not heal unless the foot can be revascularised. Transmetatarsal or ray amputation, if technically feasible, produces excellent functional results. Chopart’s mid-tarsal amputation and Symes’ through-ankle amputation are rare in chronic limb ischaemia and are not recommended because of the risks of developing an equinus deformity (in Chopart’s), movement of the distal flap (in Symes’), poor long-term flap viability and considerable technical difficulties in prosthetic fitting. Thus, the commonest major levels of amputation in limb ischaemia are transtibial, knee disarticulation, Gritti–Stokes and transfemoral. Hip disarticulation and hindquarter amputation are rare and in 2006–7 accounted for just over 1% of all cases of lower limb amputations referred to the prosthetic centres in the UK. Dysvascularity was given as the cause for this level of amputation in only 19% of cases.3 In our experience this level of amputation is mainly considered for people with neoplasia (usually sarcoma) or intravenous drug users (IVDUs). Preservation of the knee joint has enormous advantages in terms of mobility. In one study, 80% of transtibial amputees achieved unlimited household mobility or better, compared with 40% of above-knee amputees.11 In a Sheffield study, only 26% of transfemoral vascular amputees achieved community ambulation, compared with 50% of transtibial vascular amputees at 1-year follow-up of a group of amputees who underwent prosthetic rehabilitation. In this study group, the figures for household mobility were 48% and 63%, respectively, for transfemoral and transtibial vascular amputees at 1-year follow-up.12 Transcutaneous oximetry (tcPO2),13 photoplethysmography,14 laser Doppler velocimetry,15 thermography16 and isotope clearance rates17 have all been shown to correlate with subsequent stump healing. However, while all these methods seem superior to Doppler ankle pressures,18 a review concluded that sensitivities and specificities were inadequate to recommend their clinical use.19 The energy cost of walking with prostheses for vascular amputees is increased by 63% and 117%, respectively, in unilateral transtibial and transfemoral amputees compared with non-amputees. In bilateral transfemoral amputees, it is calculated that energy cost is 280% higher.20 Therefore, it should not seem surprising that even in a selected group of bilateral transfemoral amputees who were successfully trained to walk with prostheses in an inpatient rehabilitation facility, the majority of them abandoned walking when they returned home and preferred to be wheelchair-dependent.21 • Preserve the knee joint whenever possible if it is anticipated that the patient has the potential to achieve prosthetic walking or has the potential to use a prosthetic limb for assisting transfers from chair, bed, etc. • In patients likely to remain chair- or bed-bound following amputation, a transtibial amputation risks non-healing and may become a hindrance to transfers if flexion contractures of the knee and hip joints develop. In such patients, knee disarticulation or Gritti–Stokes amputation seems a better option. • Where there is a fixed knee flexion deformity of 25% or more and/or severe arthropathy, satisfactory fitting of a transtibial prosthesis for walking may not be possible. In such cases, a more proximal amputation should be undertaken. • For patients likely to remain wheelchair- or bed-bound, including bilateral amputees, knee disarticulation or Gritti–Stokes amputation is preferable to transfemoral or transtibial as the longer lever lengths and larger surface areas are more conducive to transferring and provide a much better seating balance. • In patients where a transtibial amputation is not possible but the patient has the potential to walk, most amputee rehabilitation units prefer a transfemoral rather than knee disarticulation or Gritti–Stokes amputation. This is because of problems of prosthetic fitting, which may compromise cosmetic appearance and function. Conversely some studies have demonstrated better functional outcomes in patients with a through knee amputation. • tissues must be handled with care with good haemostasis; • flaps should be oversized initially and then shaped and trimmed as required; • good-quality sensate skin coverage of stump without any tension; • bone edges should be smoothed off and bevelled; • skin and muscle flaps should be trimmed and shaped to prevent dog ears, redundant tissue or a bulbous stump; • creating the correct shape of the stump is the responsibility of the surgeon at the time of surgery; • the use of a thigh tourniquet can reduce blood loss significantly during fashioning of muscle flaps. Ensure adequate muscle (myoplastic) cover over the cut end of femur to prevent pain and discomfort and allow balanced action of flexors and extensors.22 The technique of myodesis, where drill holes are made in the bone to fix muscles, may not be applicable in ischaemic limbs due to poor tissue quality. However, this minimises the risk of the muscles slipping off the end of the femur. The myoplasty and myodesis need to be performed with the hip joint in the neutral and naturally adducted position. Historically, this level of amputation was considered in those patients who were deemed incapable of walking. The longer stump assists transfers, sitting balance and maintains muscle attachment and proprioception. However, recent research articles including a systematic review and meta-analysis suggest that the primary outcome measure of Physical Component Score (PCS) of the short-form-36 measure of quality of life (SF-36) are much higher for through- knee amputation than transfemoral amputation. A significantly greater proportion of patients with through-knee amputation were able to walk 500 metres than those with transfemoral amputation. However, patients with a through-knee amputation wore their prosthesis significantly less and had significantly more pain than those with a transfemoral amputation.23 Another study24 has concluded that the through-knee amputation is associated with an acceptable primary healing rate and satisfactory functional outcome in patients with peripheral arterial disease. This study concluded that the advantages of through-knee amputation over transfemoral amputation make it the preferred alternative for patients with vascular disease who are candidates for prosthetic rehabilitation. The conventional through-knee amputation is associated with problems caused by the bulbous femoral condyles and leakage of synovial fluid. The modified Gritti–Stokes amputation avoids these problems and has fewer problems with wound healing than the alternative Mazet technique (Fig. 6.2). Limitations in prosthetic fitting due to a lowered knee centre, and limited availability of stance and swing phase control mechanisms in the prosthetic knee joint at this level, make the through-knee level unpopular with prosthetists, and further research is needed to develop suitable prosthetic devices. This may be prompted by the increasing use of the through-knee level for soldiers and civilians with extensive lower leg injuries caused by antipersonnel mines or improvised explosive devices (IEDs). Many surgeons now favour the skew flap technique25 rather than the traditional Burgess long posterior flap.26 The skewed skin flaps are based on the arteries that run with the long and short saphenous veins, which provide the main blood supply to the skin. In a small study of posterior flap and skew flap techniques, evaluation of flap hypoxia demonstrated that the posterior flap was associated with greater and more persistent reduction in tcPO2.27 The Burgess amputation still seems useful when skew flaps might be compromised by the medial skin incision of a failed femorodistal bypass graft or following fasciotomies (Fig. 6.4).
Amputation, rehabilitation and prosthetic developments
Epidemiology
Indications for amputation
Level selection
Surgical considerations
Transfemoral amputation
Through-knee amputation
Transtibial amputation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree