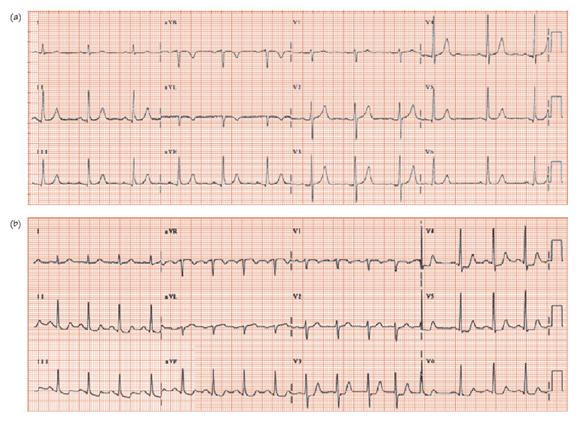
Fig. 29.2 ECG in acute coronary syndromes (ACSs). A patient admitted with acute chest pain, initially pain free (a); later in pain (b). Admission ECG virtually normal; there is a dominant (i.e. upright) T wave in lead V1 (sometimes this indicates an acute circumflex lesion). The ECG during chest pain shows widespread ST depression, downsloping in the inferior leads, planar in the antero-lateral leads. In ACS, ST depression of 1 or 2 mm increases 1-year mortality respectively by six and 10-fold. The ST depression here is 1 mm, is extensive and involves the anterior chest leads (another independent predictor of poor outcome). With such ECG changes, regardless of other risk factors, early angiography with a view to revascularization is appropriate.
Acute coronary syndromes (ACSs) are due to thrombus within a coronary artery that: (i) transiently or permanently occludes the vessel; and (ii) can break up, so embolizing fragments to the distal myocardium. Vessel occlusion and distal embolization account for the cardinal clinical feature, ischaemic chest pain at rest. Though the thrombus can resolve spontaneously without harm, the clot has the potential to abruptly close the vessel, leading to infarction and death. Some ACSs have a high mortality, others only a small increase; the ECG is one factor that can be used: (i) to diagnose the presence of an ACS; and (ii) to differentiate risk. A basic scheme of ACS, depending on the presentation ECG and troponin levels, is as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


