Fig. 18.2 Risk classification in patients presenting to the emergency room with acute chest pain considered due to ishaemic heart disease (IHD). Myocardial infarction (MI) was suspected if the ECG showed ST-segment elevation of ≥ 1 mm or pathological Q waves in ≥ 2 leads, findings not known to be old. Ischaemia was suspected if the ECG showed ST-segment depression of ≥ 1 mm T-wave inversion in ≥ 2 leads and if these findings were not known to be old. Risk factors included systolic blood pressure ≤ 110 mmHg, bilateral rales heard above the bases, and known unstable IHD (defined as worsening of previously stable angina, new onset of angina after infarction or after a coronary revascularization procedure, or pain the same as that associated with a prior MI). Basic clinical data is surprisingly good at predicting prognosis.
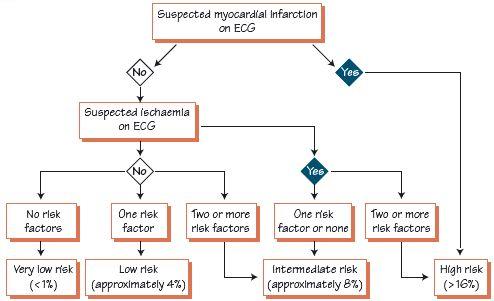
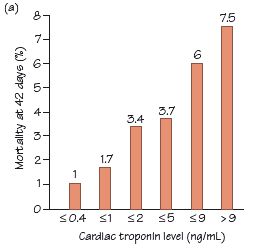
Fig. 18.3 (a) Troponin level and outcome. There is a strong graded relationship between troponin rise and adverse events. Note: (i) not all patients with a raised troponin are at high risk; and (ii) not all ‘troponin-negative’ are at low risk. Troponin-negative patients need further risk stratification by pre-discharge exercise stress testing. (b) Age and ECG changes relate to risk in unstable angina, i.e. there should be a lower threshold to admit/invasively investigate the elderly. (c) Interaction between ECG changes, risk and benefit from an invasive policy (i.e. early coronary angiography and percutaneous coronary intervention [PCI]/coronary artery bypass graft [CABG]).
In managing chest pain one aims to establish the diagnosis and start treatment as soon as possible. The working diagnosis should be based on the clinical features (demographics, history, examination) rather than on tests (unless they are categorically diagnostic).
Prognosis in chest pain
Conditions with a high risk of death/serious injury include high-risk acute coronary syndrome (ACS) (non-ST segment elevation myocardial infarctions [NSTEMIs; Fig. 18.1] and ST segment elevation myocardial infarctions [STEMIs]), acute aortic syndromes, pulmonary emboli, chest infection with pleurisy and pneumothorax. Each has specific demographics, histories, physical examination and ‘typical’ ECGs (see Chapters 20, 29, 30 and 31), which may establish the diagnosis. If not, form a working diagnosis from the clinical features and prove this using advanced tests, while excluding other conditions if they are dangerous and possible. If it is still not possible to reach a clear-cut diagnosis, proceed on the basis of the probability of dangerous chest pain. The ECG can help risk stratification, and the predictors of prognosis in acute chest pain are:
- Normal ECG, associated with a good (not perfect) long-term outcome, as most dangerous chest pain is due to ishaemic heart disease (IHD) and most dangerous manifestations of this are associated with an abnormal resting ECG. There are exceptions as follows. (i) Two to five per cent of myocardial infarctions (MIs) have a normal presentation ECG but the usual MI-related complications (including death). The diagnosis of MI must use the clinical features as well as the ECG – heavy (‘crushing’), severe (‘the worst ever’) retrosternal pain, with sweating, nausea and vomiting. Patients with such symptoms should be observed for ≥ 12 h before reaching a benign diagnosis. (ii) Some high-risk ACS present with a normal ECG, and only later does the ECG becomes abnormal, hence again the need for observation and further ECGs. (iii) Some severe non-cardiac disease presents as chest pain with a normal ECG, e.g. pulmonary emboli (sinus tachycardia is often present) and aortic dissection (ECG often normal). Do not rule out dangerous conditions on the basis of a normal ECG – always factor in the clinical features.
- ST elevation or Q waves not known to be old (early relative risk ± 17× increased).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


