Corrected QT (QTc) interval prolongation has been shown to be an independent predictor of mortality in many clinical settings and is a common finding in hospitalized patients. The causes and outcomes of patients with extreme QTc interval prolongation during a hospital admission are poorly described. The aim of this study was to prospectively identify patients with automated readings of QTc intervals >550 ms at 1 academic tertiary hospital. One hundred seventy-two patients with dramatic QTc interval prolongation (574 ± 53 ms) were identified (mean age 67.6 ± 15.1 years, 48% women). Most patients had underlying heart disease (60%), predominantly ischemic cardiomyopathy (43%). At lease 1 credible and presumed reversible cause associated with QTc interval prolongation was identified in 98% of patients. The most common culprits were QTc interval–prolonging medications, which were deemed most responsible in 48% of patients, with 25% of these patients taking ≥2 offending drugs. Two patients were diagnosed with congenital long-QT syndrome. Patients with electrocardiograms available before and after hospital admission demonstrated significantly lower preadmission and postdischarge QTc intervals compared with the QTc intervals recorded in the hospital. In conclusion, in-hospital mortality was high in the study population (29%), with only 4% of patients experiencing arrhythmic deaths, all of which were attributed to secondary causes.
Prolongation of the corrected QT (QTc) interval is a common occurrence in the hospital, but the causes and outcomes of patients with extreme QTc interval prolongation during hospital admissions are poorly described, and the proportion of these patients who have underlying congenital long-QT syndrome (cLQTS) is unknown. We describe the clinical problem of hospital-recorded QTc interval prolongation in terms of the patient population affected, including the prevalence of cLQTS, other potential contributing causes, outcomes, and the progression of electrocardiographic changes over time.
Methods
Patients were drawn from a single academic tertiary center (University Hospital, London Health Sciences Centre, London, Ontario, Canada). The hospital has a catchment area of 1 million residents. Hospitals in close proximity share 1 electronic medical records platform, and thus hospital-based services for the catchment population can reliably be captured. The protocol was approved by the Health Sciences Research Ethics Board of the University of Western Ontario.
Electrocardiograms (ECGs) were recorded at any time during a hospital admission. Electronically interpreted ECGs were identified when the automated algorithm’s interpretation of the digitally acquired MUSE (GE Healthcare, Waukesha, Wisconsin) ECG included a QTc interval >550 ms. These ECGs were then overread by an electrophysiologist working in the inherited heart rhythm clinic (RY, ADK, GJK). ECGs and accompanying patients were excluded if (1) the repeat measurement resulted in a QTc interval <500 ms, (2) the QRS width was >120 ms, (3) the heart rate was >100 or <30 beats/min, (4) rhythm was atrial fibrillation or atrial flutter, and (5) patients or surrogate decision makers were unable or unwilling to give informed consent. The QT interval was measured from the onset of the QRS complex to the end of the T wave, as defined by the intersection of the tangent drawn at the maximum downslope of the T wave with the isoelectric T-P line. The mean QT interval of 3 consecutive QT interval measurements at a stable RR interval was used. The QT interval measurements were corrected for heart rate using Bazett’s correction formula (QTc = QT/√RR). Previous ECGs were sought for all patients, with the most recent ECG used as a reference if acquired at a distinct time point from the acute hospitalization leading to the index ECG.
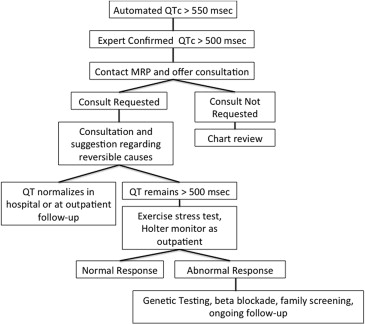
The most responsible physician of the patient with an automated QTc interval >550 ms, and a verified QTc interval >500 ms, received a notification of the extreme value and was offered an arrhythmia service consultation to review the patient ( Figure 1 ). If the most responsible physicians requested consultations, patients underwent review either in the hospital or as outpatients, at which time reversible causes of QTc interval prolongation were identified and treated whenever possible, including drug review at www.qtdrugs.org . A full medical and genetic history, including 3-generation pedigree, were obtained. Further testing, including Holter monitoring, exercise testing, or genetic testing, was performed at the discretion of the consulting electrophysiologist. The patients were then classified initially by the presumed most responsible cause for QTc interval prolongation on the basis of the most responsible physicians’ classifications and a subsequent independent chart review by the authors (BM, ZL). Categories of responsible causes included drugs, ischemia (acute presentation attributed to unstable coronary artery disease), electrolyte imbalance (serum calcium <2.1 mmol/L, serum potassium <3.0 mmol/L, and serum magnesium < 0.7 mmol/L), acute intracranial processes, hypothermia (core temperature <36°C), and cLQTS.
Statistical analysis was performed using SPSS version 16.0 (SPSS Inc., Chicago, Illinois). A p value <0.05 was considered to indicate statistical significance. Univariate testing was performed using the chi-square or Student’s t test.
Results
One hundred seventy-two patients (mean age 67.6 ± 15.1 years, 48% women) with QTc intervals >550 ms from April 2010 to August 2011 were identified and selected for complete chart and follow-up review. The mean QTc interval on the identifying ECG was 574 ± 53 ms ( Table 1 ). Most patients (60%) had underlying heart disease, predominantly ischemic cardiomyopathy. Credible presumed reversible causes associated with QTc interval prolongation were identified in 98% of patients ( Table 2 , Figure 2 ), with 41% and 8% having 2 and 3 identifiable causes, respectively ( Table 3 ). The most common cause was QTc interval–prolonging medication and was deemed most responsible in 48% of patients, with 25% of these patients taking ≥2 offending drugs ( Table 4 ). Antidepressant and antiarrhythmic medications were the most common culprits ( Table 5 ). In addition, 35 patients were taking loop diuretics.
| Age (years) | 67.6 ±15.1 (20-102) |
| Female | 83 (48%) |
| Underlying Heart Disease | 103 (60%) |
| Ischemic Cardiomyopathy | 74 (43%) |
| Valvular | 12 (7%) |
| Dilated Cardiomyopathy | 10 (6%) |
| Congenital | 3 (2%) |
| Hypertrophic Cardiomyopathy | 1 ( 1%) |
| Cardiomyopathy NYD | 12 (7%) |
| QTc (msec) | 574 ± 53 |
| Left Ventricular Ejection Fraction (N = 103) | 46.3 ± 14 (15-65) |
| Hypertension | 95 (55%) |
| Diabetes Mellitus | 36 (21%) |
| Diabetes requiring insulin | 13 (8%) |
| Chronic Renal Insufficiency | 24 (14%) |
| Hemodialysis | 6 (3%) |
| Chronic Obstructive Lung Disease | 15 (9%) |
| QT prolonging medication | 83 (48%) |
| Acute intracranial process | 11 (6%) |
| Coronary Ischemia | 38 (22%) |
| Electrolyte Abnormalities | 37 (22%) |
| Congenital Long QT Syndrome | 2 (1%) |
| Unknown | 2 (1%) |
| QT prolonging medication | 118 (69%) |
| Acute intracranial process | 16 (9%) |
| Coronary Ischemia | 58 (34%) |
| Electrolyte Abnormalities | 82 (48%) |
| Hypothermia | 1 (1%) |
| Bradycardia | 1 (1%) |
| 2 causes | 71 (41%) |
| 3 causes | 14 (8%) |
| 1 QT prolonging medication | 88 (75%) |
| > 1 QT prolonging medication | 30 (25%) |
| Anti-depressants | 53 |
| Anti-psychotics | 16 |
| Anti-arrhythmics | 41 |
| Antibiotics | 14 |
| Antidopaminergics | 11 |
| Serotonin Antagonists (5HT3) | 11 |
| Other | 15 |
| Anti-depressants | 53 |
| Selective serotonin reuptake inhibitors | 32 |
| Serotonin-norepinephrine reuptake inhibitors | 4 |
| Serotonin antagonist and reuptake inhibitors | 10 |
| Tricyclic antidepressants | 7 |
| Anti-psychotics | 16 |
| Typical antipsychotics | 5 |
| Atypical antipsychotics | 11 |
| Anti-arrhythmics | 41 |
| Amiodarone | 36 |
| Sotalol | 4 |
| Dronedarone | 1 |
| Antibiotics | 14 |
| Sulpha | 1 |
| Fluoroquinolones | 11 |
| Macrolides | 2 |
| Antifungal (imidazole) | 2 |
| Antiviral | 1 |
| Anti-dopaminergic | 11 |
| Serotonin antagonists (5HT3) | 11 |
| Anticonvulsants | 2 |
| Cholinesterase inhibitors | 1 |
| Alpha blockers | 1 |
| Diuretics (indapamide) | 1 |
| Anti-histamines | 3 |
| Anti-muscarinics | 4 |
Thirty-one patients (18%) were seen in consultation by the electrophysiology service while in the hospital (15 of 172 [9%]), as outpatients in the inherited heart rhythm clinic (14 of 172 [8%]), or at a general electrophysiologist outpatient practice (2 of 172 [1.2%]). Four patients underwent genetic testing through a commercial laboratory, either PGx Health (New Haven, Connecticut) or GeneDx (Gaithersburg, Maryland), as previously described. Of the 31 patients assessed, 2 had long-QT syndrome risk scores >3.5, 1 of whom had a pathogenic mutation.
The single patient with genotype-positive long-QT syndrome was a 67-year-old man who was found to have a frameshift mutation in exon 10 of the KCNH2 gene (p.Asn819ThrfsX49), which results in a premature stop codon and a truncated protein product. He initially presented to the emergency department with noncardiac chest pain and was receiving ciprofloxacin for presumed community-acquired pneumonia. He had no history of syncope or seizure and no family history of sudden cardiac death. The other patient with a long-QT syndrome risk score >3.5 was a 59-year-old woman who presented after resuscitation from cardiac arrest presumed secondary to long-QT syndrome.
Eighty-four patients had ECGs available before hospital admission in addition to the index ECG identified during hospital admission. QTc intervals during hospital admission were increased from baseline, with a mean increase of 133 ± 11 ms (p <0.0001). Fifty-four patients had ECGs in follow-up in addition to the index hospital-acquired ECG. QTc intervals at follow-up were shorter, with a mean decrease of 115 ± 16 ms (p <0.0001). Forty-four patients (81%) had QTc intervals <500 ms at follow-up. Of the 37 patients who had ECGs before hospital admission and during follow-up after hospital admission, QTc intervals after hospital admission were significantly increased (mean increase 37 ± 19 ms, p = 0.0003; Figures 3 and 4 ).




