Ventricular Preexcitation
8.1. Concepts and Types
- Ventricular preexcitation occurs when the electrical stimulus reaches the ventricles before the normal activation through the specific conduction system (SCS). In fact, this phenomenon is not really a preexcitation, but rather early ventricular excitation. [A]
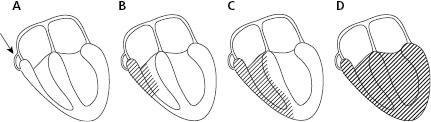
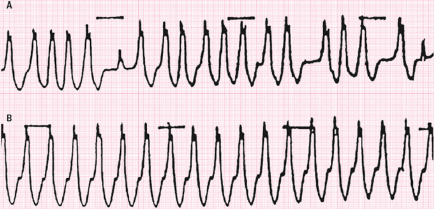
- Early ventricular excitation, mistakenly known as preexcitation, was described by Wolff, Parkinson, and White in young persons presenting paroxysmal arrhythmias, and is known as Wolff–Parkinson–White (WPW) syndrome. Early excitation occurs because of the existence of short muscular bundles with accelerated conduction (accessory pathway), known as Kent bundles, that connect the atria to the ventricles. These bundles may involve conduction that is anterograde, retrograde, or both. The degree of anomalous activation is variable (Fig. 8.1).
- Rarely, early excitation takes place through long bundles that connect the right atrium with the fascicles or muscular mass of the right ventricle and present anterograde decremental conduction only. This is known as atypical preexcitation and includes the phenomenon previously known as Mahaim preexcitation.
- Also the preexcitation may be due to the existence of an atrial-hisian bundle, which carries the stimulus from the atrium to the ventricle faster, or may be due simply to accelerated AV conduction. This is known as short PR-type preexcitation, or Lown–Gannon–Levine syndrome.
- The presence of preexcitation, especially WPW syndrome, favors the appearance of potentially dangerous supraventricular arrhythmias (see later).
8.2. WPW-Type Preexcitation
8.2.1. Electrocardiographic Characteristics (Fig. 8.2) [B]
(A) Short PR Interval
This is due to early ventricular excitation through an accessory pathway, that occurs before the normal excitation arrives through the SCS.
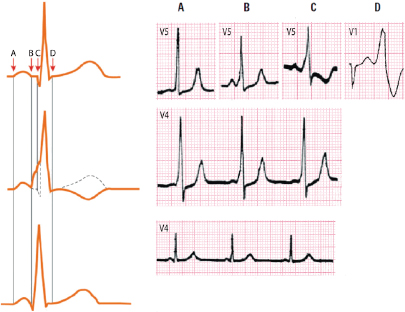
(B) QRS Morphology
The QRS is usually wide (≥0.11 s) and its morphology depends on the location of the accessory pathway. However, in all the cases as the location in the ventricular muscle of the accessory pathway takes place in an area with few Purkinje fibers, some initial slurrings in the QRS complex, known as delta wave, are present. Later, the stimulus arrives through the normal pathway, and the ventricles are activated through two fronts, configuring a true fusion complex that presents a greater or lesser degree of preexcitation depending on the quantity of preexcited ventricular mass (Fig. 8.1).
Figure 8.2 shows various degrees of WPW-type preexcitation (above right). See how from A to C an increasing degree of delta wave. D is a case of atrial fibrillation with a second complex presenting the maximum degree of preexcitation. In the middle part of the figure, four successive complexes are seen in a case of moderate preexcitation. With a clear short PR and an exclusive short PR-type preexcitation below. On the upper left, normal ventricular activation is shown. In the middle, WPW preexcitation shows short PR and a delta wave with an earlier QRS complex seen in points, but with the same final QRS resembling that found in normal patients. This is because ventricular activation is a fusion complex between the first preexcited part and the second part activated by a normal pathway.
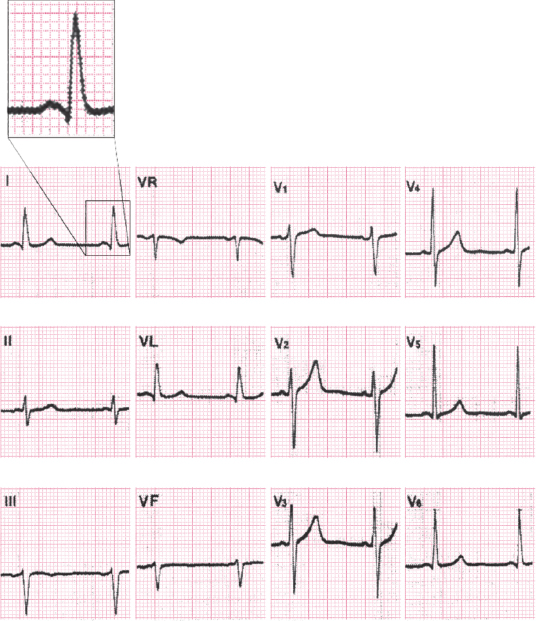
8.2.2. Types of WPW-type Preexcitation [C]
WPW-type preexcitation may be classified into four types according to the accessory pathway location. Figure 8.3 shows this organization and the repercussions of the anomalous pathway location on ECG morphology. We must always remember that in WPW preexcitation ventricular activation is shared by the accessory pathway and the normal pathway (Figs 8.1–8.3). Figures 8.4 and 8.5 show examples of the four types of preexcitation with evident delta waves.
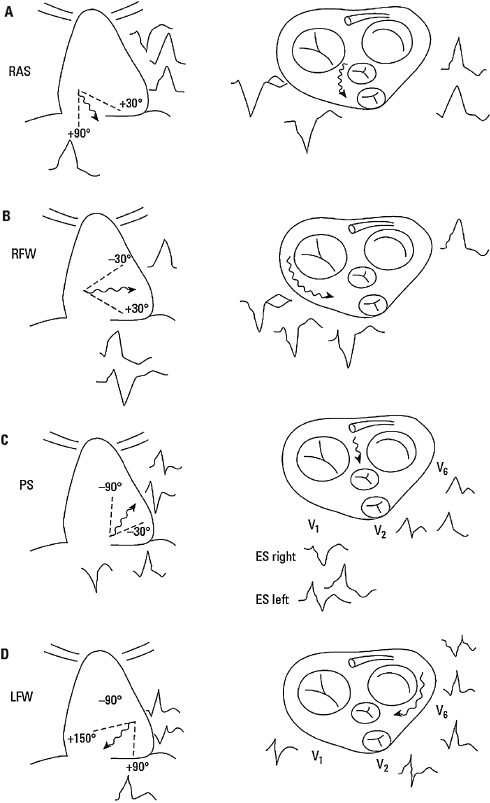
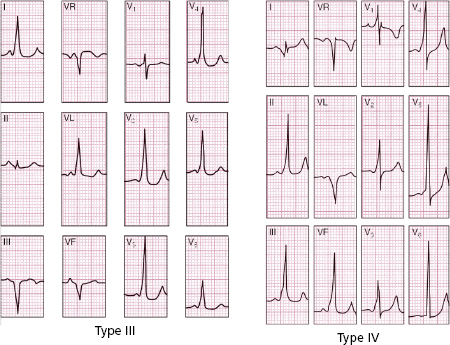
Many algorithms have been described based on the location of the delta wave in certain leads. These algorithms can be used to locate the accessory pathway quite precisely (Bayés de Luna, 2012a). However, the predicted location must always be confirmed before performing ablation of the pathway.
Sometimes preexcitation is intermittent and occasionally may appear progressively (concertina effect). Figure 8.6 shows a case of sudden intermittent preexcitation and Figure 8.7 shows how preexcitation disappears progressively (concertina effect).

8.2.3. Confirming or Ruling Out Preexcitation
- The injection of adenosine, a selective blocker of the AV node, can confirm (if the ECG pattern appears clearly), or rule out (if the ECG pattern does not modify) the preexcitation. [D]
- The presence of q in V6 practically rules out preexcitation.
8.2.4. WPW-Type Preexcitation and Arrhythmias
WPW preexcitation may be related to certain types of arrhythmia.
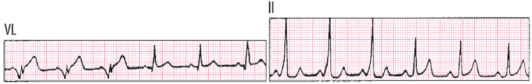
A. Reentrant Paroxysmal Tachycardias of the AV Junction with an Accessory Pathway [E]
(JRT-AP; also named AVRT, see Chapter 11.)
- The accessory bundle may participate in the reentrant circuit of a paroxysmal tachycardia of the AV junction, with retrograde conduction through the accessory pathway and anterograde conduction through the SCS. The atria are activated through the accessory pathway after anterograde activation of the ventricles through the normal pathway, and thus P’ is located after a narrow QRS. This differentiates these tachycardias from those in which the re-entrant circuit is found exclusively in the AV junction (JRT-E) (see Chapter 10).
- Figure 8.8 shows in the first two complexes (A) the activation through the accessory pathway (
 ) and later (B), after an atrial extrasystole (P’), the activation blocked in the accessory pathway and carried anterograde in through the AV junction of the SCS with a narrow QRS (1), originating a re-entrant tachycardia with retrograde atrial activation through the accessory pathway (P’ located after QRS) (P’R > RP’). The subsequent QRS complexes are also narrow (3) (orthodromic tachycardia) (see Chapter 11).
) and later (B), after an atrial extrasystole (P’), the activation blocked in the accessory pathway and carried anterograde in through the AV junction of the SCS with a narrow QRS (1), originating a re-entrant tachycardia with retrograde atrial activation through the accessory pathway (P’ located after QRS) (P’R > RP’). The subsequent QRS complexes are also narrow (3) (orthodromic tachycardia) (see Chapter 11).
- In rare cases of reentrant tachycardia, the anterograde conduction to the ventricles is made through one accessory pathway (Kent bundle or a long anomalous pathway in atypical preexcitation with retrograde conduction (see Fig. 8.3). This is known as antidromic tachycardia.
- ECGs can generally be used to identify these two types of antidromic tachycardias that present a similar morphology to that of LBBB (QS in V1 and R in V6). Antidromic tachycardia through the Kent bundle presents a LBBB-like morphology with transition to R in precordial leads before V4 and the antidromic tachycardia through a long atriofascicular pathway of atypical preexcitation presents a LBBB-like morphology with a transition to R in precordial leads in V4 or later (see Bayés de Luna, 2011 and 2012a). For the differential diagnosis of antidromic tachycardia with ventricular tachycardia. See Section 12.2.3.2 in Chapter 12 (Steurer et al., 1994).
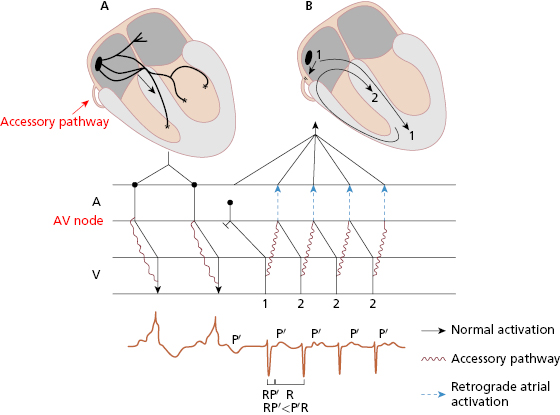
B. WPW Preexcitation and Atrial Fibrillation or Flutter
- Patients with WPW more frequently present episodes of atrial fibrillation (AF) or flutter (AFL). Usually this is explained because a ventricular extrasystole (VE) carried quickly and retrogradely through the accessory pathway encounters atria that are vulnerable because they are outside the refractory period, which is generally shorter, and may trigger AF or AFL.
- Occasionally, a supraventricular paroxysmal tachycardia may also trigger AF or AFL for a similar reason.
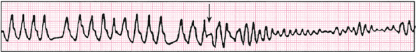
- The differential diagnosis between AF of WPW syndrome and ventricular tachycardia is relatively easy, even though QRS is wide in both scenarios. The diagnostic criteria are exposed in the legend of Figure 8.9. However, the differential diagnosis is more difficult when AFL, rather than AF, is present (Fig. 8.10). [F]
- Occasionally, a supraventricular paroxysmal tachycardia may also trigger AF or AFL for a similar reason.
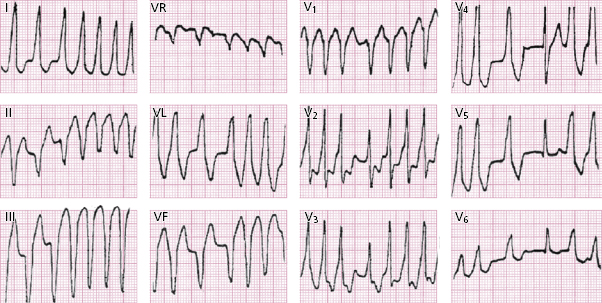
C. Atrial Fibrillation in WPW Syndrome and Sudden Death
- Sudden death (SD) in WPW may appear in the presence of very fast AF when the RR is very short, allowing the supraventricular stimulus to fall into the vulnerable stage in the ventricles (Fig. 8.11). This usually does not occur if preexcitation disappears at high heart rate during a stress test, and if the refractory period of the accessory pathway is long. [G]
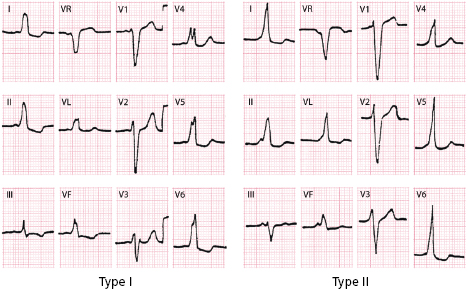
8.2.5. Differential Diagnosis in WPW-Type Preexcitation
- WPW types I and II = LBBB. [H]
- WPW type III = inferior infarction, right ventricular enlargement (VE), and RBBB.
- WPW type IV = lateral infarction, right VE, and RBBB.
The key in every case is to measure the PR interval and to detect any delta waves.
8.3. Atypical Preexcitation
- The accessory bundle is long, with slow conduction and goes from the right atrium to the right ventricle (atriofascicular or atrioventricular bundle). [I]
- The ECG is often almost normal, or with only small degrees of preexcitation in the form of small initial slurrings of R wave in I and V6, and often with rS in lead III that mimick partial LBBB (accessory pathway in RV).
- It may originate tachycardias with wide QRS usually of LBBB type, because the anterograde conduction is made through one long right accessory bundle (see Figure 8.2.4.A and Bayés de Luna 2011, and 2012a).
8.4. Short PR-Type Preexcitation
- In this case early excitation is produced by an accelerated AV conduction, or by the existence of an atrial hisian bundle that avoids slow conduction through the AV node. [J]
- Figure 8.2 (bottom) shows a case of short PR-type preexcitation in which the end of QRS complex occurs earlier because the entire activation, which starts early, occurs through the SCS.
- Figure 8.12 shows a typical example of short PR-type preexcitation. It is important to remember that these patients are also at risk for potentially serious arrhythmias, especially in cases of rapid AF.
Self-assessment
A. What is ventricular preexcitation and how many types exist?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


