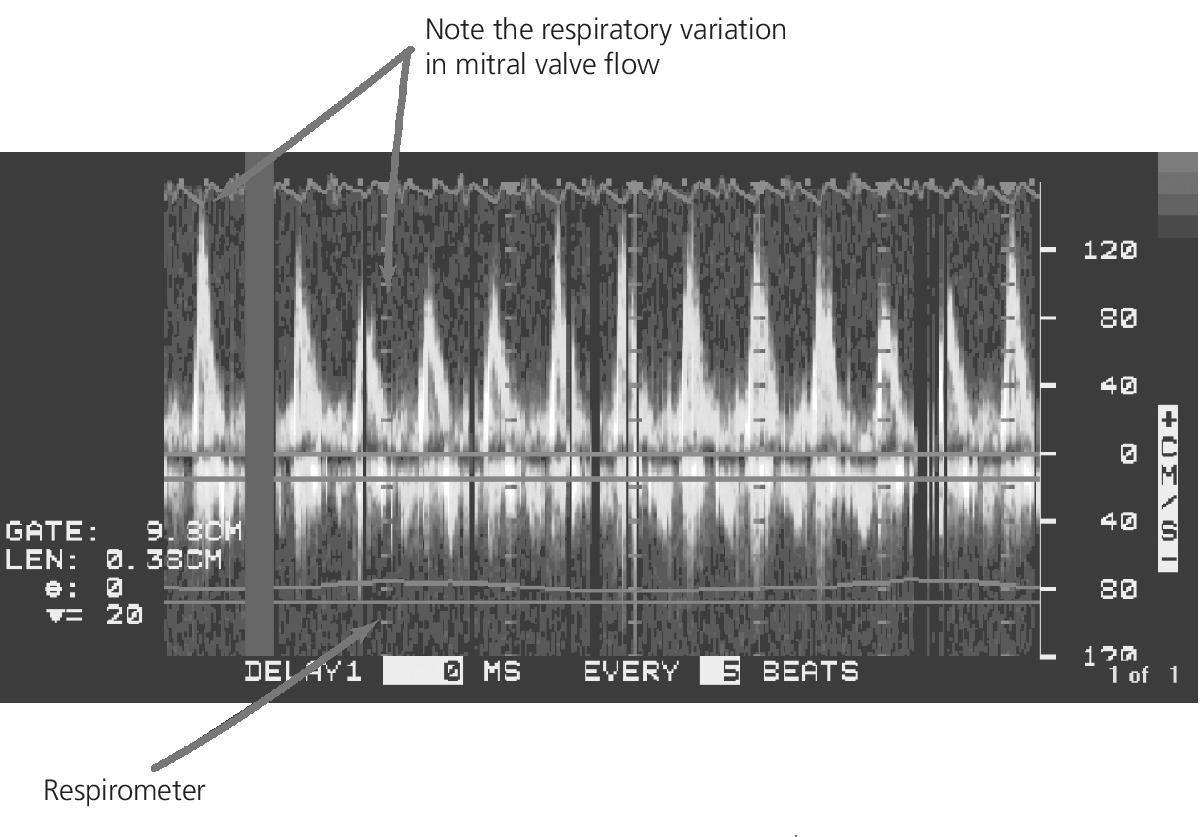
CHAPTER 19 Siva B. Mohan and George A. Stouffer The pericardium is a fibroserous sac consisting of two parts: (a) a strong external layer composed of tough fibrous tissue, called the fibrous pericardium; and (b) an internal double‐layered sac (visceral and parietal pericardium) composed of a transparent membrane called the serous pericardium. The parietal pericardium is fused to the internal surface of the fibrous pericardium. The visceral pericardium is reflected onto the heart, where it forms the epicardium, the external layer of the heart wall. The potential space between the parietal and visceral layers of the serous pericardium is called the pericardial cavity. It normally contains a thin film of serous fluid that enables the heart to move and beat in a frictionless environment. The pericardium stabilizes the heart within the thoracic cavity by virtue of its ligamentous attachments, and also prevents extreme dilatation in the setting of a sudden rise of intracardiac volume. The normal pericardial space contains 15–40 mL of pericardial fluid. A myriad of conditions produce pathologic accumulation of fluid in the pericardial cavity. Fluid that accumulates in the pericardial space can be serous, sero‐sanguineous, hemorrhagic, chylous, or a combination of the above. Once a critical threshold of pericardial fluid is reached, the pericardial pressure rises in a nonlinear fashion, resulting in hemodynamic compromise or cardiac tamponade (Figure 19.1). Figure 19.1 Schematic of the phases of cardiac tamponade. Source: Courtesy of Cardiovillage.com. The primary hemodynamic pathophysiologic process in the development of tamponade is increased pericardial pressure that impairs diastolic filling [1–6]. Normal pericardial pressure is zero; any increase can have hemodynamic consequences. One way of looking at tamponade is that the effusion competes with the cardiac chambers to occupy the limited volume within and surrounded by the pericardium. Another way to think of tamponade is as a rubber band around the cardiac chambers, exerting a constrictive force and preventing adequate expansion. Resultant elevations in intracardiac diastolic pressures impair systemic and pulmonary venous return, leading to venous congestion and reduced cardiac output (Figure 19.2). As pericardial pressures increase, a variety of compensatory mechanisms are elicited, including sympathetic nervous system activation, which leads to tachycardia, increased ejection fraction, peripheral vasoconstriction, and sodium and fluid retention. Figure 19.2 Cardiac tamponade. The pericardium is a relatively noncompliant structure and thus the relationship between pericardial pressure and volume is nonlinear. Pericardial pressure rises exponentially as pericardial fluid volume increases after a certain threshold is reached. Factors that influence the development of hemodynamic compromise in the setting of a pericardial effusion include the rate at which the fluid accumulates, the amount of pericardial fluid, the compliance of the pericardium, the size of the pericardial space, and ventricular compliance. The pericardium expands only minimally in the acute setting, but can greatly increase in size over prolonged periods of time. Thus, patients with a slowly developing effusion may be asymptomatic even with a large‐volume effusion. In contrast, if the rate of accumulation is rapid, even a small volume of effusion may trigger hemodynamic compromise (e.g., in the setting of cardiac trauma). The inherent compliance of the pericardium also plays a role in determining the hemodynamic significance of an effusion. Several disease processes may render the pericardium more stiff or noncompliant, allowing for a smaller effusion to cause cardiac tamponade. Left and right ventricular hypertrophy renders the heart most resistant to elevated pericardial pressures. The hemodynamic effects of increased pericardial pressure occur on a spectrum and cardiac tamponade can be divided into three phases [5,7]. As the pericardial fluid accumulates, the pericardial pressure rises. Increasing pericardial pressure leads to increasing right atrial (RA) pressure. At this point, clinical signs of tamponade may be absent as the right heart, including right ventricular (RV) stroke volume, but not the left heart is compromised (phase 1). As pericardial fluid continues to accumulate and pericardial pressure rises, pulmonary capillary wedge pressure (PCWP) begins to rise and external compression of both left and right ventricles is present (phase 2). End‐diastolic pressures (EDP) throughout the cardiac chambers are elevated and within 5 mm Hg of each other, including RA, RVEDP, pulmonary artery, PCWP, and LVEDP. At this stage, classic signs and symptoms of cardiac tamponade are usually seen. In this phase, compensatory tachycardia maintains cardiac output in the presence of diminished stroke volume. Eventually, if pericardial pressures continue to rise and approximate RA and RV diastolic pressures, cardiac output falls, and cardiac tamponade progresses to shock with impaired tissue perfusion (phase 3). See Table 19.1. In patients with tamponade, a relatively larger amount of atrial filling occurs following ventricular contraction, since as blood is ejected to the great vessels during ventricular systole, ventricular volume transiently falls, enabling atrial expansion and filling. RA pressure drops immediately following ventricular contraction as atrial volume increases; this large swing in RA pressure gradient in the setting of cardiac tamponade elicits an exaggerated RA X descent. The X descent may be exaggerated during inspiration since a decrease in pericardial pressure leads to augmentation of blood flow to the RV during inspiration (Figure 19.2). Conversely, the Y descent corresponds to passive ventricular filling and is blunted. Following removal of pericardial fluid with a resulting reduction in pericardial pressure, the Y descent in the RA tracing will become more apparent (Figure 19.4). Table 19.1 Findings on catheterization. Figure 19.3 RA pressure tracing in a patient with tamponade. Note the increased RA pressures, preserved respiratory variation, and blunted Y descent. Figure 19.4 Simultaneous right atrial and pericardial pressure tracings in a patient with tamponade before and after the removal of 400 mL of pericardial fluid. Figure 19.5 Aortic pressure tracing in a patient with tamponade showing pulsus paradoxus. Source: Courtesy of Cardiovillage.com. Several clinical scenarios can mask the clinical diagnosis of tamponade. In the setting of hypovolemia and suspected tamponade, the typical hemodynamic findings may be masked. Low‐pressure effusions equilibrate only with right‐sided diastolic pressures and at first only during inspiration. A fluid bolus may elicit classic findings. Severe left ventricular dysfunction may also mask tamponade. In this setting, LV diastolic pressures are higher than RV diastolic pressures and the diagnosis of cardiac tamponade should be dependent on demonstrating elevated pericardial pressures equal to RA pressures. Regional cardiac tamponade can occur when some, but not all, cardiac chambers are compressed by loculated effusions. Typical hemodynamic abnormalities maybe found only in the compressed chambers or zones. In some cases, loculation may also produce classic tamponade, presumably by “stretching” the pericardium. Tremendous efforts are expended in determining whether a patient is “in tamponade” and, thus, qualifies for emergent therapy. It is important to note that increased pericardial pressure is a clinical spectrum rather than an all‐or‐none phenomenon. The important questions are “What is the approximate pericardial pressure?” and “What effect is the pericardial fluid having on cardiac output, arterial blood pressure, and intracardiac pressures?” The determination of the need for pericardiocentesis must weigh the risk of the procedure versus these questions and other important considerations, including the rate of accumulation and the potential diagnostic value of obtaining pericardial fluid. The European Society of Cardiology Working Group on Myocardial and Pericardial Diseases has proposed a stepwise scoring system to be used in patients with suspect tamponade. A score ≥6 warrants immediate pericardiocentesis in the absence of contraindications [9]. The physical examination can provide clues to cardiac tamponade. Sinus tachycardia and hypotension with narrow pulse pressure are hallmarks. The clinician must remain aware that blood pressure may remain normal or even elevated until cardiovascular collapse is imminent. Pulsus paradoxus, as already described, is an “exaggerated” drop in systolic blood pressure during normal inspiration (not forced inspiration). This is a common finding in moderate to severe tamponade. To measure pulsus paradoxus, the sphygmomanometer should be inflated to suprasystolic pressure, deflating until Korotkoff sounds are initially heard in expiration only. Then, the cuff should be deflated until Korotkoff sounds are heard throughout the respiratory cycle. The difference of these two pressures is the “paradox” (normal pulsus paradox is <10–12 mm Hg). This finding is neither specific nor sensitive and may be seen in other conditions, including constrictive pericarditis, severe obstructive pulmonary disease, restrictive cardiomyopathy, pulmonary embolus, obesity, and right ventricular infarction (Figure 19.6). Figure 19.6 Aortic pressure tracings from four patients with pulsus paradoxus. Only the patient in (d) had tamponade. Note that the recording in (c) is made at a speed slower than normal to show several respiratory cycles. Jugular venous distension is usually present with a preserved X descent. In tamponade, venous waves in the neck are not outward pulsations, but rather X descents are apparent as a collapse from a high standing pressure level. The Y descent is typically not seen. Kussmaul’s sign, which was originally described as an increase in the jugular venous pressure with inspiration but is now commonly used to describe the lack of a decrease in JVP with inspiration, is not classically seen in tamponade without a component of constrictive disease (i.e., effusive–constrictive disease) [10]. Beck’s Triad, described in 1935, is a cluster of findings in cardiac tamponade characterized by hypotension, muffled heart sounds, and jugular venous distension. Pericardial friction rub may be heard in the setting of pericarditis. The echocardiogram is a useful tool in the diagnosis of cardiac tamponade; however, it is important to note that cardiac tamponade is a clinical diagnosis. The echocardiogram is a relatively quick, noninvasive test, which may aid the clinician in delineating the size, morphology, hemodynamic impact, and location of the effusion. Important findings on echocardiography include the following: Figure 19.7 Doppler recording of LV inflow with a superimposed respirometer in a patient with tamponade. Note the decrease in mitral valve flow during inspiration.
Cardiac tamponade
Hemodynamic pathophysiology
Hemodynamic findings
Elevated diastolic pressures and equalization of end‐diastolic pressures
X descent is preserved, but Y descent is small or absent on RA pressure tracing
Pericardial pressure is elevated
RV pressure does not fall in early diastole (i.e., there is no dip and plateau configuration)
Pulsus paradoxus 
Physical exam findings
Hemodynamics of cardiac tamponade as measured with echocardiography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


