ECG Patterns of Ventricular Arrhythmias
In this chapter, we describe the ECG characteristics of ventricular arrhythmias. Their mechanisms have been explained in Chapter 10.
12.1. Premature Ventricular Complexes
12.1.1. Ventricular Extrasystoles (VE): Fixed Coupling Interval
This mechanism is explained in Chapter 10. We will now look at how it appears in the ECG.
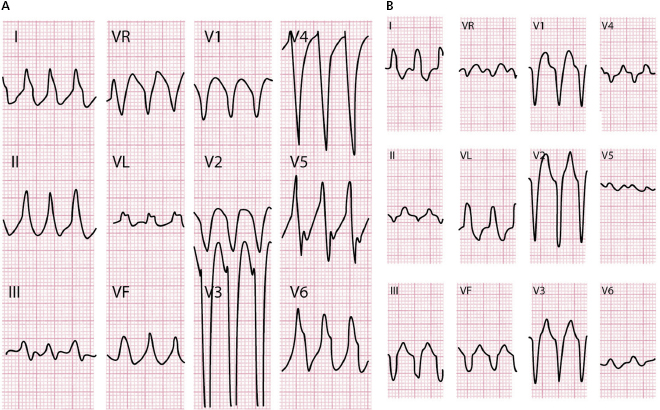
- The morphology depends on the site of origin. If VEs start in the right ventricle (RV), the morphology resembles that of LBBB, and if they start in the left ventricle (LV), R wave may be present in V1 as in the case of RBBB. Often, the morphology does not resemble branch block (e.g. all positive or negative in the HP). [A]
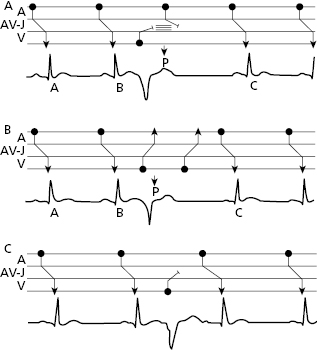
- In healthy individuals, QRS does not present notches and repolarization is opposite to QRS and asymmetrical. When there is associated pathology, notches are frequent, especially in the plateau of QRS. Figure 12.1 shows the three types of conduction of ventricular extrasystoles (VE) in the atria: (A) VE remains cancelled in the AV junction, with the next sinus impulse also blocked, and a complete compensatory pause originates (BC = 2AB); (B) the VE is conducted to the atria and depolarizes the sinus node, changing its cadence (incomplete compensatory pause [BC < 2AB]; and (C) VE remains blocked in the AV union, but the next P may be conducted, generally with a longer PR due to the concealed conduction phenomenon (interpolated VE) (Chapter 10).
12.1.2. Lown Classification of VE from Low to High Degrees of Severity
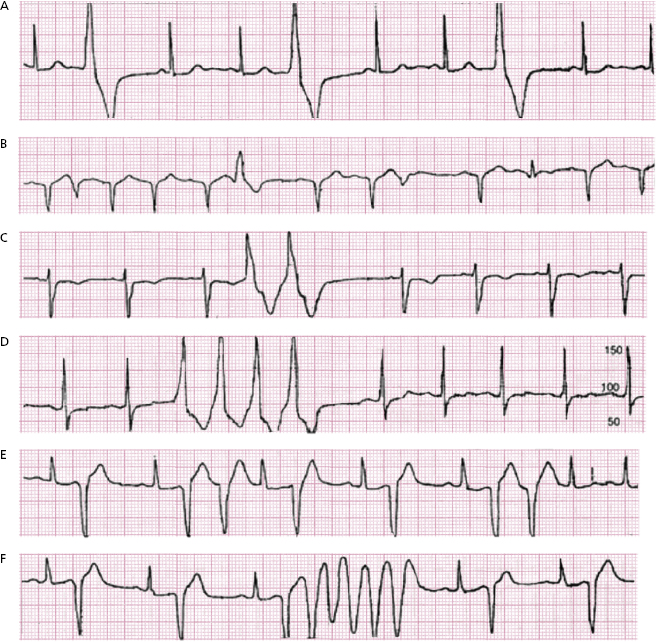
Lown and Wolf (1971) classified five types of VE: (1) isolated; (2) frequent (>30 per hour); (3) polymorphic; (4) repeating forms: (a) pairs and (b) runs; and (5) with R/T phenomenon (Fig. 12.2). [B]
In practical terms, the risk for the patient is mostly related to the clinical context in which it appears. The most serious cases occur during the course of acute ischemia and in patients with a low ejection fraction (<30%). In these patients a VT/VF may be produced, especially when Lown classification is high. The R/T phenomenon is especially dangerous in acute ischemia.
12.1.3. Ventricular Parasystole: Variable Coupling Interval
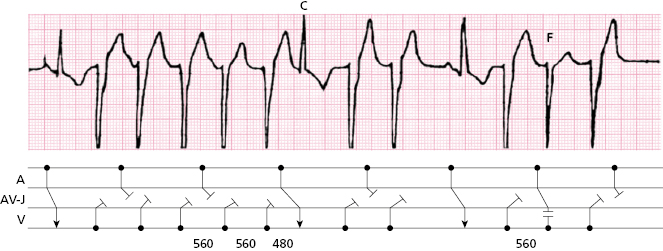
They are very infrequent, and only in rare cases are presented in the form of runs, usually slow, of VT. [C]
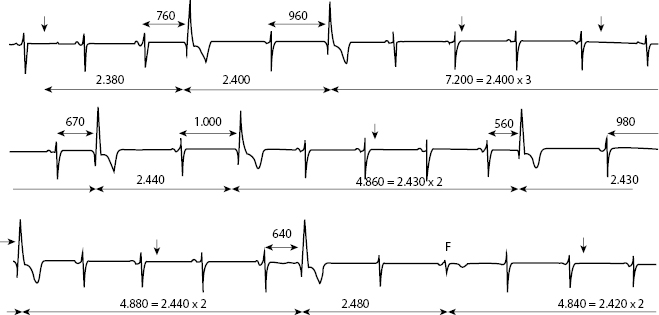
Figure 12.3 provides an example of ventricular parasystole: variable coupling intervals (from 560 to 1000 ms), multiples ectopic spaces, and the presence (third row) of fusion complexes (F) when the cadence of sinus and ectopic focus coincide.
12.2. Ventricular Tachycardia
The mechanisms are explained in Chapter 10. They may be sustained or appear in runs.
12.2.1. Classification
Monomorphic [D]
We refer mainly to classical VT (QRS ≥ 120 ms). It may be idiopathic, usually of a focal origin (↑ automaticity or microreentry), or appear in patients with heart disease (may be focal or due to a macroreentry (scar or branch-to branch) (Fig. 10.6).
Rarely, VT originates in the upper part of one fascicle with narrow QRS (<120 ms) and morphologies resembling intraventricular conduction disturbances, and, exceptionally, VT may be of parasystolic origin. These forms of VT are not discussed in this book (see Bayés de Luna, 2011 and 2012a).
Polymorphic
The most frequent types are torsades de pointes VT. There are also other types such as bidirectional VT, catecholaminergic VT, etc (see Bayés de Luna, 2011–2012).
12.2.2. Idiopathic Monomorphic Ventricular Tachycardia
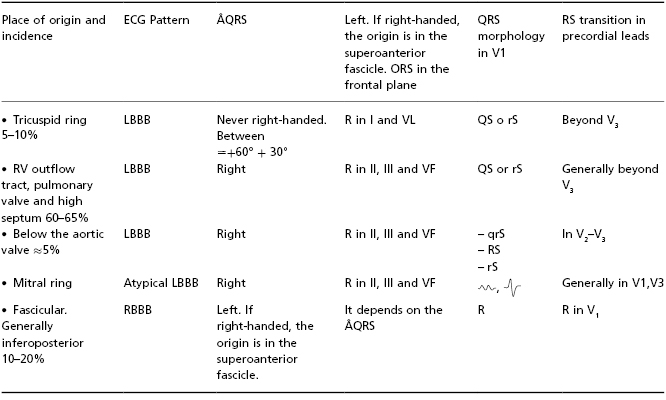
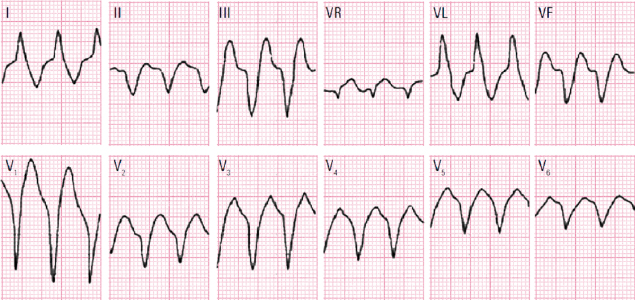
Idiopathic monomorphic ventricular VT may originate in both ventricles (Table 12.1), explaining the morphology resembling LBBB (generally starting in VD) or RBBB (always starting in VI). [E]
Table 12.1 ECG characteristics, place of origin and incidence of different types of idiopathic monomorphic VT
If it originates in the inferoposterior fascicle of the LV, it is sensitive to verapamil and due to microreentry; if it is sensitive to adenosine it is due to triggered activity; and if it is sensitive to propranolol it is due to increased automaticity.
It may present in the form of sustained VT or in runs. Table 12.1 shows the most important ECG characteristics of different types of idiopathic VT, according to the place of origin, and Figures 12.4 and 12.5 are two examples of idiopatic VF with right and left BBB morphology.

12.2.3. Classical Monomorphic VT in Patients with Heart Disease
Sustained monomorphic VT is a relatively common arrhythmia that occurs especially in ischemic heart disease (acute and chronic phase), inherited heart diseases and when heart failure is present. In some cases VT may trigger VF and sudden death.
The VT in these cases may be triggered by different factors alone or in combination (increased automaticity, HDR, rotors, macroreentrant circuits) (see Chapter 10).
12.2.3.1. ECG Diagnosis (Figs 12.6 to 12.12)


(See also Bayés de Luna, 2012a.)
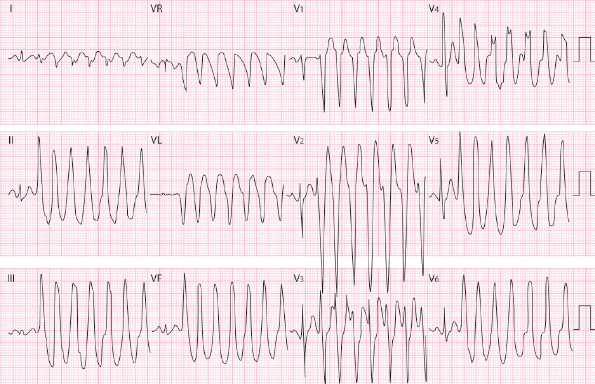
By definition, QRS in classical VT is wide (≥120 ms), its morphology varies, and it is usually different from typical bundle branch block. The type most similar to BBB is the branch-to-branch VT. In fact, this type of VT is very difficult to distinguish from a supraventricular tachycardia with LBBB aberrancy (Fig. 12.9). In other cases when VT resembles LBBB, there is usually an rS morphology in V1 with wide r >1 mm (Fig. 12.9).
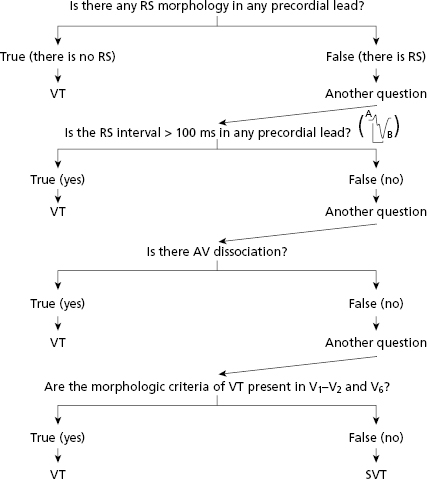
The diagnosis must be made after ruling out aberrant supraventricular tachycardia. This may be carried out following the sequential algorithm of Brugada et al. (1991), based on some morphological criteria (steps 1, 2 and 4 of the algorithm) and in the presence of AV dissociation. The other criteria explained below are also helpful.
- Morphological criteria: Table 12.2 shows the classical morphologies that indicate aberrancy or ectopy in tachycardia with wide QRS including the criteria used in the Brugada algorithm (step 4) and those of Pava et al. (2010) (favors ectopy a peak time of R in lead II > 50 ms), and Vereckei et al. (2008) (favors ectopy the presence in VR of slow recording of first 40 ms of R or Q with slurrings). [F]
- Presence of AV dissociation (Fig. 12.7). This is a crucial diagnostic criterion. Step 3 of Brugada algorithm.
- The sequential algorithm by Brugada, based partially on some of the mentioned criteria, is useful to make the differential diagnosis between VT with wide QRS and high Se and SP, as explained in Figure 12.6. The first step is to look for the presence of RS morphology in precordial leads. If none are found, VT is indicated (Fig. 12.10). Second, if RS is present in the precordial leads, the duration of the R/S interval is measured (Fig. 12.6). If greater than 100 ms, VT is indicated. If less than 100 ms, the third step is taken: looking for AV dissociation (Fig. 12.9). If not found, we move to the fourth step, which involves morphological criteria as shown in Table 12.2 and below. [G]
Figures 12.7 to 12.9 show three clear examples of VT based on morphologic criteria and Brugada’s algorithm (Figs 12.7 and 12.9, first criteria and 12.8, second and third criteria).
- Other important criteria
- Capture and fusion complexes. The presence of these complexes confirms the presence of VT (Fig. 12.11).
- Atrial activity occurring before the first complex of wide QRS tachycardia confirms that this type of VT is supraventricular (Fig. 12.12).
- Presence of AV dissociation (Fig. 12.7). This is a crucial diagnostic criterion. Step 3 of Brugada algorithm.
Table 12.2 Aberrancy versus ectopy in tachycardia with wide QRS
In favor of ectopy:
|
In favor of aberrancy:
|
12.2.3.2. Summary of Differential Diagnosis of Wide QRS Tachycardia
The criteria explained before (Brugada sequential algorithm and others) are useful for performing the correct diagnosis between aberrancy and ectopy in cases of wide QRS tachycardia with high SP and Se.
The most difficult cases are the branch-to-branch TV, because usually the QRS morphology is very similar to LBBB (see Fig. 12.10).
On the other hand, both the antidromic tachycardia due to the Kent bundle and to atriofascicular fibers may be difficult to differentiate from sustained VT. However, the antidromic tachycardia due to the Kent bundle compared with the one due to atriofascicular fibers, present in the precordial leads transition to R wave before V4 (see Section 8.2.4 in Chapter 8). The Brugada algorithm is not useful for performing differential diagnosis between junctional reentrant antidromic tachycardia and VT. We may use the criteria of Steurer (1994). According to these, the following criteria favor VT: (1) Negative QRS from V4 to V6; (2) QR pattern in one lead from V2 to VL; and (3) ÂQRS located between −60 to +150°.
12.3. Polymorphic Ventricular Tachycardia (Fig. 12.13) [H]
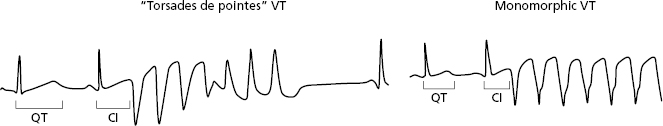
The most important type of polymorphic VT is ‘torsades de pointes VT’. This tachycardia is characterized by a change in polarity of the QRS (Dessertene, 1966), which is more visible in certain leads, and a long QT interval. Figure 12.13 shows a run of torsades de pointes VT in a patient with long QT syndrome.
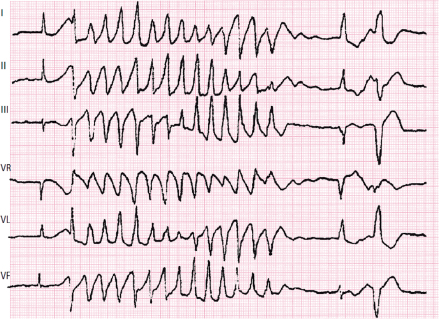
The differentiating characteristics between classical VT, monomorphic VT, and torsades de pointes VT are shown in Figure 12.14.
For more information on other types of polymorphic VT see Bayés de Luna, 2011 and 2012a).
12.4. Accelerated Idioventricular Rhythm (Fig. 12.15)
Ventricular rhythm with wide QRS that does not surpass 100 bpm indicates accelerated idioventricular rhythm (AIR), because true ventricular tachycardia only exist when the rate is above this threshold. [I]

In the presence of AIR, fusion complexes occur, presenting a morphology between ventricular rhythm and sinus rhythm that can have a similar rate. Based on the quantity of ventricular mass activated by ventricular or sinus rhythm, different degrees of complexes of intermediary morphologies (Fig. 12.15) (fusion complexes) exist. The morphology goes from capture complexes (the entire complex is sinus, see Fig. 12.7), to different intermediate patterns between the sinus complex and the ventricular extrasystole (VE) that depolarize the entire ventricular mass. The fusion complexes depolarize more or less the quantity of the ventricular myocardium, and according to that will be more or less within a degree of similarity with the basal rhythm (Fig. 12.13).
12.5. Ventricular Flutter (Fig. 12.16)
Ventricular flutter is a fast (≈300 bpm) and regular ventricular arrhythmia. The QRS complexes do not have an isoelectric line between them and repolarization is not observed. [J]
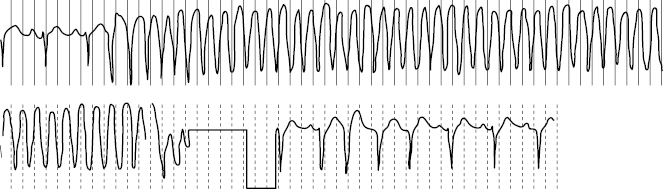
The differential diagnosis with fast VT is difficult to perform, although the repolarization signs are not seen in ventricular flutter. In addition, it may be confused with 1 × 1 atrial flutter with aberrancy (Bayés de Luna, 2012a).
Ventricular flutter usually triggers VF/SD unless it appears in the intensive care setting (Fig. 12.16).
12.6. Ventricular Fibrillation (Figs 12.17 and 12.18)
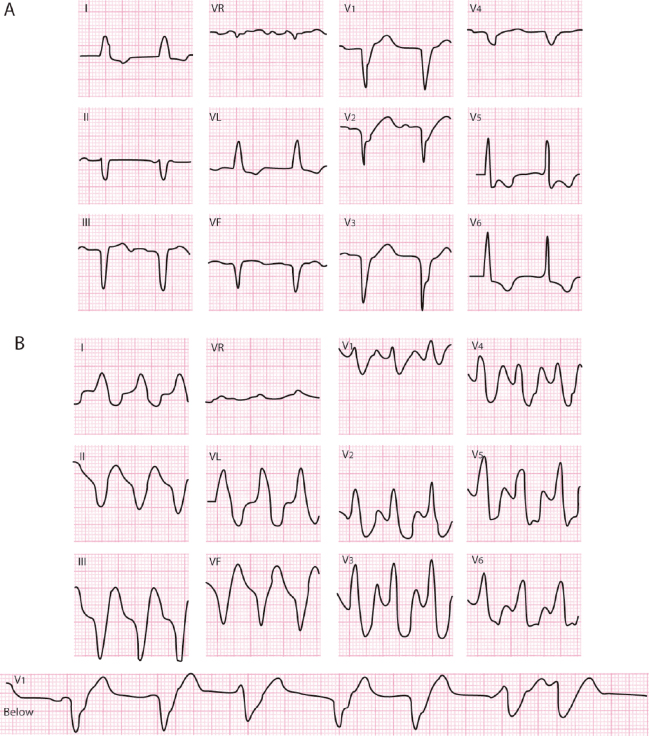
Ventricular fibrillation is a fast, irregular arrhythmia with a rate greater than 300–400 per minute that may be originated by (a) multiple reentries; (b) spiral wave (rotor), or c) HDR (see Chapter 10). It does not generate mechanical activity and leads to cardiac arrest and death, with the exception of rare self-limiting cases or situations where the patient is resuscitated with cardioversion or previously with an implantable cardioverter–defibrillator (ICD). [K]

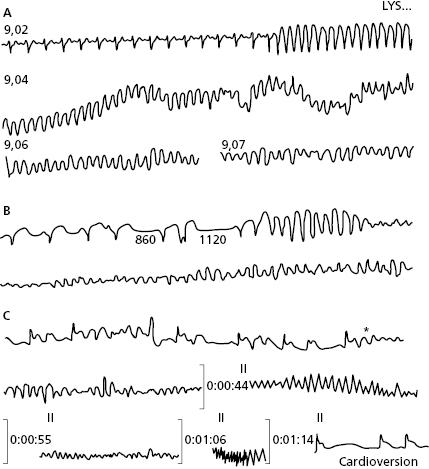
The ECG shows (Fig. 12.17) a fast and irregular rhythm, with QRS varying in morphology and height and without visible repolarization. When voltage is low, recuperating the basal rhythm is proportionally more difficult.
Ventricular fibrillation may be preceded by sustained VT, generally in patients with chronic ischemic heart disease (Holter recorder) (Fig. 12.18A). On other occasions (Fig. 12.18B) ventricular fibrillation is primary and occurs during the course of myocardial infarction and, less frequently, in ambulatory patients (Bayés de Luna et al., 1985). Ventricular fibrillation is triggered by VE (*) (Fig. 12.18C) and on very rare occasions is self-limiting. If may be resolved with cardioversion (Fig. 12.16C) if it appears in the intensive care unit or in ambulatory patients with an implanted ICD (see Bayés de Luna, 2011 and 2012a).
Self-assessment
A. Describe the ECG of ventricular extrasystole.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 especially if in V6
especially if in V6 
 (Vereckei et al., 2008)
(Vereckei et al., 2008)

 if in V6
if in V6 



