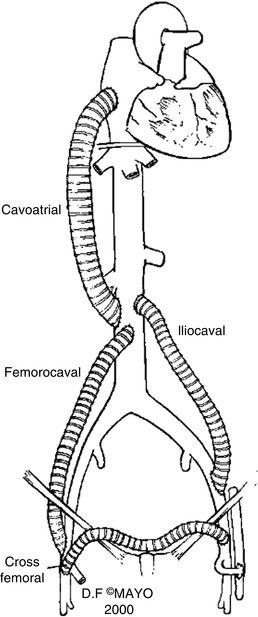
Fig. 16.1
This 68-year-old man presented with gradual onset of massive bilateral lower extremity edema several years after a course of radiation therapy to the abdomen for an ampullary carcinoma. Duplex ultrasound showed no evidence of reflux; however, venogram and IVUS demonstrated a clear stenosis of the IVC. This was treated with angioplasty and stenting and there was near-complete resolution of the leg edema. IVUS images through the stenotic portion of the IVC and the more normal distal IVC are shown in the insets
Patients with a known history of iliofemoral DVT represent a uniquely high-risk group for iliac or caval obstruction. Previous longitudinal studies have demonstrated that only 20–30 % of iliac vein thrombi completely recanalize with anticoagulation alone, while the remaining veins develop persistent obstruction with variable collateral formation [4, 5]. Thus, pelvic imaging should be obtained in patients with a history of DVT and/or thrombophilic disorders and coexisting CVI. Although frequently clinically silent, the importance of primary, non-thrombotic iliac vein obstruction (May-Thurner syndrome or iliac vein compression syndrome) can play an important role in the pathogenesis of iliac vein obstruction. As reported by Meissner et al., among approximately 1,000 limbs that were treated for iliocaval obstruction, approximately 40 % had non-thrombotic occlusion [6].
16.3 Diagnostic Imaging
The absence of a “gold standard” imaging modality represents an obstacle in the systematic study of patients with iliac vein obstruction. There are now multiple imaging studies that are complementary, however, and together can provide a clear view of the underlying pathophysiology. With judicious application of these available tests, the savvy practitioner can amass enough information to reliably diagnose and treat nearly all patients with deep venous reflux.
The evaluation of both valvular incompetence and obstruction almost always begins with duplex ultrasonography (US). Unfortunately, duplex US is unreliable for assessment of the iliac veins, especially in obese patients. Duplex US is, however, the starting point for a comprehensive evaluation and will yield the first clues that there may be an issue above the level of the inguinal ligament. Loss of respiratory variation in the femoral tracing or poor signal augmentation with distal limb compression during duplex US examination of the femoral vein may be indicative of venous outflow obstruction. Data from a large retrospective study by Lin et al. that included 2,963 limbs scanned with duplex US documented abnormal monophasic waveforms in the common femoral veins in 124 patients [7]. Just under 50 % of these patients with abnormal waveforms had evidence of prior DVT or iliac vein stenosis on computerized tomography (CT) scan. Based on this and other similar studies, it is reasonable to pursue central imaging in all CVI patients with abnormal Doppler waveforms in the common femoral vein. But while specific criteria for duplex detection of central venous stenosis have been described, the most significant finding is usually what the duplex does not show. That is, if there are severe symptoms of chronic venous insufficiency, but minimal infrainguinal reflux or occlusion, a more proximal cause must be suspected.
Ascending venography provides greater detail than simple duplex US, detects extensive iliac vein stenosis, and images collateral flow. It is an essential study when surgical intervention is planned [6]. The Achilles heel of venography is that it often does not provide adequate visualization of focal obstructions with a post-thrombotic or non-thrombotic cause [9]. For instance, a post-thrombotic iliac vein may still appear to have flow with multiple small recanalized channels while still representing a major physiologic obstruction (Fig. 16.2a). In addition, anterior-posterior (AP) compression, as might be present in a May-Thurner syndrome, will be completely missed by a standard venogram in an AP projection. CT and magnetic resonance venography (MRV) appear to be more sensitive for detection of spatially complex and focal lesions (Fig. 16.3). Unfortunately, significant technical expertise in MRV or CT is required to produce consistently reliable images and may not be widely available in all locales. Significant obstructions are also not uncommon in asymptomatic patients [10]. IVUS is increasingly viewed as the superior imaging modality in estimating the extent of iliac vein stenosis since it allows real-time visualization of the details and morphology of intraluminal obstruction [11, 12]. In addition, IVUS allows definitive identification of focal lesions and can be used as a guide during angioplasty and stenting. When performed in conjunction with direct pressure measurement, many practitioners feel that it is the most sensitive and specific method of identifying hemodynamically significant stenoses in the iliocaval system. While IVUS is an invasive procedure, high-quality images are easily obtained, and interpretation is straightforward. Figure 16.2 demonstrates a situation in which a post-thrombotic iliac vein appeared patent on venogram but was near occluded as demonstrated by IVUS. In this case, the post-thrombotic vein was treated successfully with angioplasty and stenting, resulting in near-complete resolution of the symptoms. In current practice, while purists may debate which imaging modality is the gold standard, the simple fact is that a combination of venogram and IVUS will identify nearly all significant obstructive lesions.
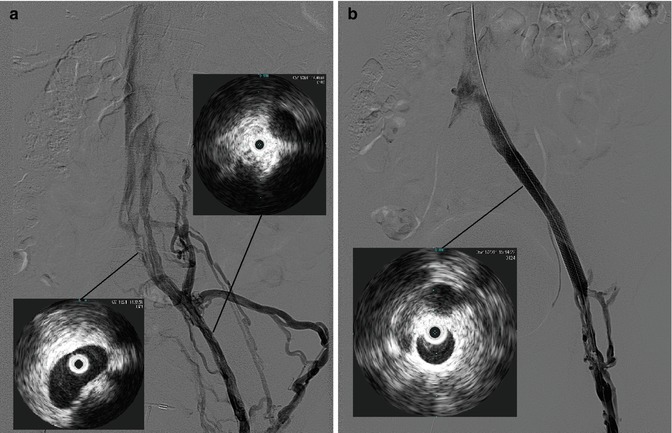

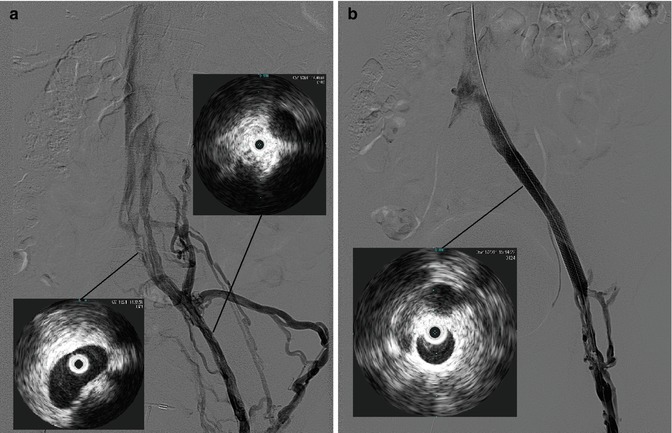
Fig. 16.2
This 44-year-old woman presented with a history of approximately 20 years of left leg edema, beginning with a DVT during pregnancy. Duplex findings were notable only for GSV incompetence; however, after an ablation of the great saphenous vein, she developed worsening symptoms with chronic, severe pain and worsening edema. Venogram shows what appears to be a patent left iliac system, but with extensive collaterals (a), and IVUS shows near occlusion of the common and external iliac veins (inset). After angioplasty and stenting, there is free flow through the iliac veins with minimal collateral flow (b) and IVUS shows a patent, re-expanded lumen (inset)

Fig. 16.3
A 65-year-old man presented with severe, recurrent varicosities of the left leg extending up to the inguinal area and buttocks. Given some suspicion of proximal obstruction, an MRV was ordered which showed only mild compression of the left common iliac vein by the left common iliac artery. This was deemed not to be physiologically significant and was not treated
The only real concern is that IVUS might be oversensitive to physiologic compression and the degree of stenosis which merits intervention is a matter of discussion and debate. The point at which stenosis should be considered hemodynamically significant in the venous system remains controversial, but stenosis of greater than 50 % is probably considered the minimum indication for intervention [6, 8]. In practice however, the decision to intervene is based on multiple factors including the degree of stenosis, the clinical presentation, and the perceived odds of success. One might be hard pressed to recommend intervention on an older patient with mild lower leg edema and a 70 % compression of the iliac vein by the overlying iliac artery. In contrast, a 70 % stenosis of the iliac vein may well-merit treatment in a post-thrombotic 35-year-old with symptomatic thigh and lower leg edema accompanied by venous claudication.
16.4 Venous Angioplasty and Stenting
Currently available treatment modalities for the management of iliac vein obstruction are large vein bypass and percutaneous stenting. In the past, the only available option for patients with iliac vein or IVC obstruction was surgical bypass. These procedures are, however, maximally invasive and technically challenging and have been associated with poor long-term results in all but the most experienced hands. Over the last decade, the success associated with percutaneous angioplasty and stenting for venous obstruction on an outpatient basis has largely relegated surgical procedures to a handful of the most intractable cases which have failed multiple attempts with an endovascular approach.
Data from several studies has demonstrated that venous stenting is associated with low morbidity and strikingly high long-term patency rates. In a case series including 982 lower extremities, Neglen et al. reported cumulative patency rates of 86 and 100 % at 5 years in patients treated for post-thrombotic and non-thrombotic iliac vein occlusion, respectively [13, 14]. The same authors reported complete pain relief in 64 % of patients, resolution of leg swelling in 34 %, and ulcer healing in 58 % of treated patients, despite the presence of untreated infrainguinal reflux in many limbs [13, 14]. Hartung et al. demonstrated that stenting of iliac obstruction was associated with significant improvement of the venous clinical severity scores (VCSS). In their study, which included 44 patients followed for an average of 27 months, VCSS were 8.5 and 2.0 before and after the procedure, respectively [15]. These excellent patency rates, and documented symptomatic improvement with a minimally invasive procedure, have revolutionized the management of deep venous obstruction. A typical case of iliac venous obstruction due to May-Thurner syndrome which was treated with venous angioplasty and stenting is presented in Fig. 16.4.
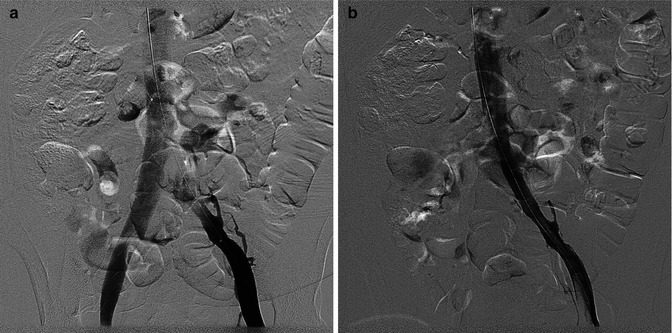
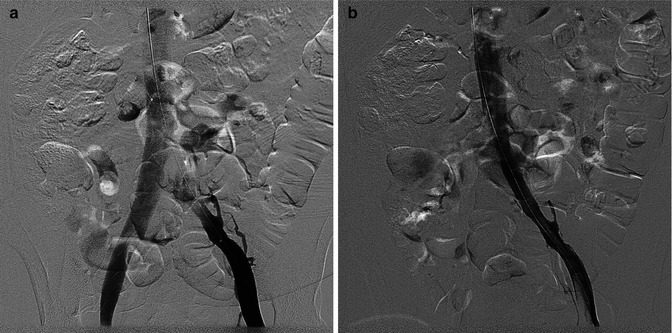
Fig. 16.4
A classic presentation of May-Thurner syndrome is illustrated by this 35-year-old woman with sudden onset of massive left leg swelling. After thrombolysis of an occluded iliac vein, there is a residual iliac stenosis (a), which was addressed successfully with angioplasty and stenting (b). The leg returned to a normal diameter within 48 h
Even very extensive iliocaval obstructions can be addressed effectively with endovascular approaches. As recently documented by Neglen and Raju, long-standing caval obstructions due to an IVC filter can be successfully and durably addressed with angioplasty and stenting [16]. Figure 16.5 illustrates a case of extensive iliac and IVC obstruction in the presence of an IVC filter which was not retrievable. This patient presented with recurrent right leg stasis ulceration that was refractory to conservative management with compression and wound care. In this case, the occluded iliac segment and IVC were recanalized and stented with almost immediate symptomatic improvement and eventual ulcer healing.
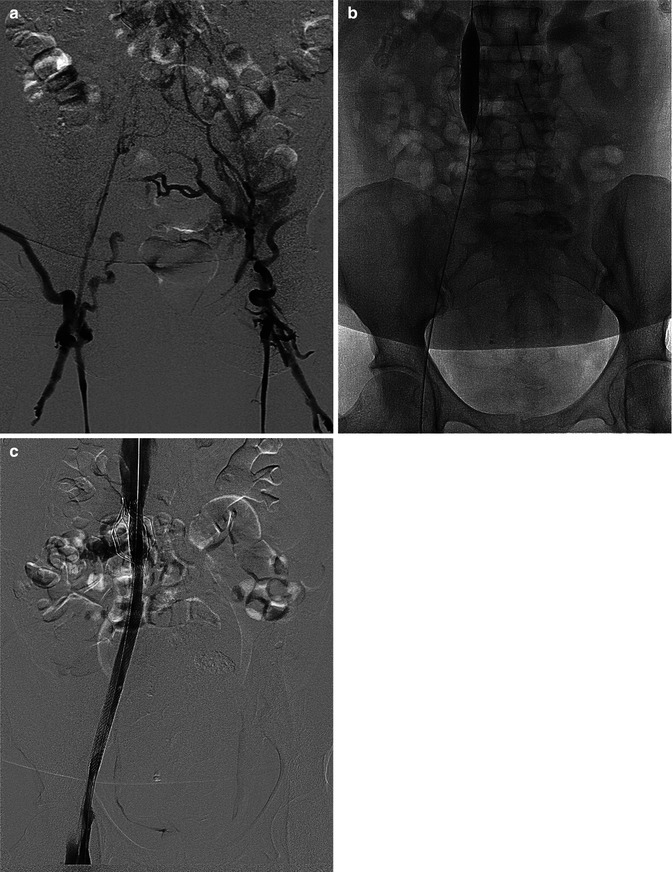
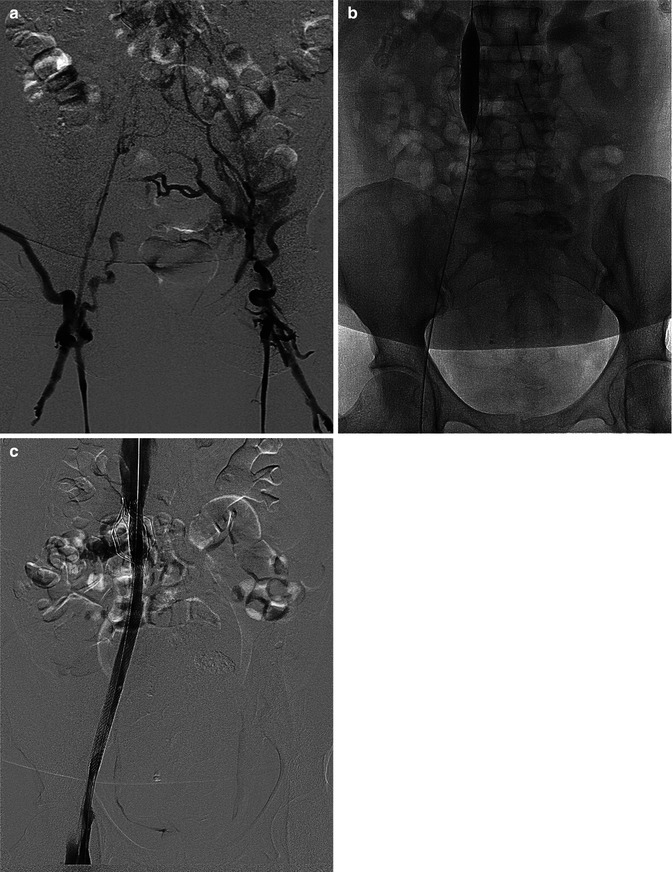
Fig. 16.5
This 55-year-old woman had a history of multiple bilateral DVTs as well as prior placement of an IVC filter and presented with recurrent right leg stasis ulcers. Complete iliocaval occlusion is demonstrated by venogram (a); however, the right iliac veins were easily crossed with a wire and the entire segment, including the occluded filter, was balloon dilated and stented (b). Completion venogram shows brisk flow across the treated segment (c)
The technical approach to venous angioplasty and stenting begins with percutaneous access of the popliteal, femoral, or greater saphenous vein. Our preference is to access the femoral vein in the mid-thigh under ultrasound guidance, since the patient can be positioned supine while still allowing visualization of the entire iliac and proximal femoral drainage. A venogram is obtained which will often diagnose obvious long-segment occlusions and document collateral flow. If the venogram is relatively normal or equivocal, the IVUS catheter is passed up over a wire and the entire iliocaval system is interrogated. If there is an occlusion, we attempt to cross the lesion with a guidewire/catheter combination and then obtain imaging proximal to the occlusion, as well as IVUS of the affected segment. Pullback pressures across a stenosis or occlusion may be obtained; however, venous pressure differentials may be quite small and difficult to interpret and are not typically a major part of our decision-making process.
If the stenosis or occlusion is deemed to be clinically significant, the next step is serial pre-dilation to near the normal expected diameter of the vein segment. Balloon dilation alone will almost never be sufficient for venous obstructions of the lower extremities, and a self-expanding stent, sized to a diameter 10–20 % greater than the expected vein diameter, is nearly always placed. The Wallstent® (Boston Scientific, Natick, MA) and SmartStent (Cordis, Bridgewater, NJ) are the most frequently used devices in this setting. After post-dilation, a completion venogram and IVUS are obtained. In our practice, patients requiring long-term warfarin are restarted on enoxaparin and warfarin immediately post-procedure, while those not on long-term systemic anticoagulation are begun on aspirin and Plavix. Presence of a stent in the iliac system alone does not necessarily mandate long-term anticoagulation with warfarin.
16.5 Venous Bypass
For a patient with the most severe and intractable symptoms of CVI, a documented central venous occlusion, and multiple failed attempts at endovascular recanalization, one of the traditional venous bypass procedures might still be considered. The first and most famous large vein bypass procedure, described by Dr. Palma (“Palma procedure”), uses contralateral great saphenous vein as a bypass conduit [17]. This procedure is designed to bypass a chronically obstructed iliac vein by mobilizing the contralateral greater saphenous vein and turning it over onto the ipsilateral femoral vein (Fig. 16.6). The largest available series, with data from an analysis of 412 procedures, demonstrated clinical improvement in 63–89 % of patients and long-term patency rates of up to 80 % [6]. A particularly optimistic review from the Mayo Clinic documented patency rates for the Palma procedure as high as 83 %, at 4 years [18]. Unfortunately, clinical success hinges on long-term patency of a fairly small conduit with relatively low flow, and the procedure is technically challenging, so real-world results may not be as advertised. Nevertheless, the morbidity of the procedure is limited, and it may be worthwhile in a small subset of patients.
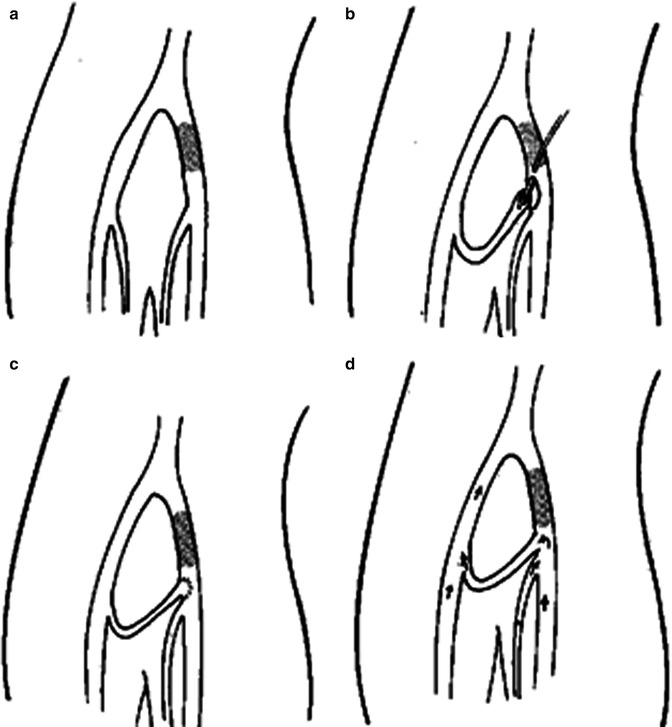
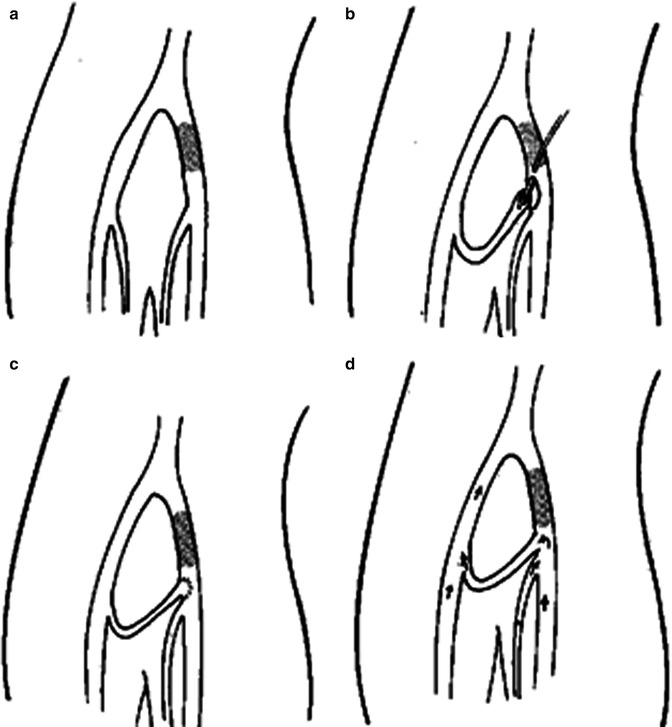
Fig. 16.6
The Palma procedure is designed to address unilateral iliac occlusion (a) by mobilization and anastomosis of the contralateral great saphenous vein to the ipsilateral common femoral vein (b, c). Drainage of the affected leg then flows through the saphenous vein and the contralateral iliac system (d) [30]
The Palma procedure is not, however, appropriate for patients with bilateral iliac occlusions or patients with complex iliocaval stenosis or occlusion. In such cases, an in-line bypass with polytetrafluoroethylene (PTFE) may be considered. In-line bypass (femorocaval, iliocaval, or even ilioatrial) may be indicated in patients with bilateral iliac occlusions, isolated caval occlusion, or very extensive iliocaval obstructions who also have relatively non-diseased venous segments proximally and distally to provide adequate inflow and outflow for the graft. In-line bypass may also be considered in cases of unilateral iliac obstruction where autologous conduit for a suprapubic graft (Palma procedure) is not available. Some typical graft configurations are seen in Fig. 16.7 [18]. One-year primary patency rates associated with in-line venous bypass have been reported to be as high as 93 % [6]. However, somewhat lower patency rates are documented in a series from the Mayo Clinic, the best realistically achievable results (Fig. 16.8) [18].