Hypertrophic cardiomyopathy (HC) has become a contemporary and treatable genetic heart disease, now with disease-related mortality reduced to as low as 0.5% per year, based largely on more effective risk stratification and the use of the implantable cardioverter-defibrillator for primary prevention of sudden death. This paradigm change in the natural history of HC has caused us to reconsider the overall mortality risk in this disease. We interrogated the databases of 2 HC referral centers, Minneapolis Heart Institute and Tufts Medical Center. Of 1,902 consecutive patients evaluated between 1992 and 2013, 1,653 patients (87%) have survived to the end of follow-up and 249 patients (13%) have died. Most deaths (178 of 249; 72%) were unrelated to HC, commonly because of cancer and predominantly in older patients. Non-HC mortality was significantly more common in adults presenting ≥60 years and least common in the youngest patients aged <30 years (p <0.001). Notably, deaths from non-HC causes substantially exceeded HC-related causes by 2.6-fold (p <0.001). In conclusion, only about 25% of patients with HC ultimately died of their disease, including predominantly those who were <30 years of age. These data allow patients with HC to develop a more realistic and reassured perception of their disease.
Long regarded as a grim and unrelenting disease with generally poor prognosis and inadequate treatment options, hypertrophic cardiomyopathy (HC) has now become a contemporary treatable disease with reasonable expectation for extended or normal longevity in many patients. HC-related mortality has decreased significantly due principally to penetration of implantable cardioverter-defibrillators into disease management for prevention of sudden death (SD). Patients with HC are, of course, still subjected to all-cause and noncardiac mortality because of a variety of other organ system diseases.
To determine the causes of mortality in a contemporary HC population, which may require redefinition in the rapidly evolving treatment environment for this complex genetic heart disease, we studied natural history and outcome of 1,902 consecutive patients. These patients were evaluated between 1992 and 2013 (27% obstructive at rest with outflow gradient, ≥30 mm Hg) at 2 HC referral institutions: Minneapolis Heart Institute Foundation and Tufts Medical Center (Boston) with complete follow-up over 6.6 ± 5.3 years.
Of 1,902 patients, 1653 patients (87%) survived to the end of follow-up, whereas 249 patients (13%) have died ( Figure 1 ). Most deaths (n = 178 of 249; 72%) were due to causes unrelated to HC, predominantly in patients aged ≥60 years: cancer (n = 37), other noncardiac (n = 16), coronary artery disease (n = 15), postoperative, including surgical myectomy (n = 9), advanced age associated with multiple cardiovascular and other organ system involvement, and co-morbidities largely independent of HC (n = 71; including nursing home deaths in patients aged >90 years [n = 20]; lost to follow-up [n = 10]).
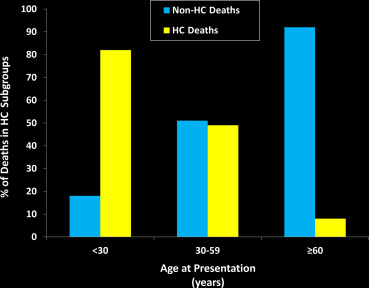
The other 71 of the 249 deaths (28%) were due to causes directly related to HC: SD (n = 31); heart failure (n = 17); embolic stroke (n = 8); postoperative (n = 7); and transplant complications (n = 8). Notably, deaths due to non-HC causes substantially exceeded HC-related causes by 2.6-fold (p <0.001; Table 1 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


