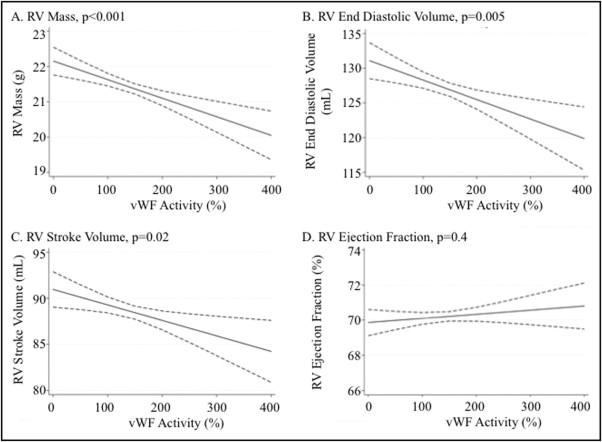
Elevation in plasma activity of von Willebrand factor (vWF) reflects endothelial dysfunction and predicts death in pulmonary arterial hypertension. Higher vWF activity is also associated with a lower right ventricular (RV) ejection fraction in pulmonary arterial hypertension. Little is known about the relation between vWF and RV structure and function in adults without cardiovascular disease. The present investigation included 1,976 participants with magnetic resonance imaging assessment of RV structure and function and measurement of vWF activity from the Multi-Ethnic Study of Atherosclerosis. Multivariable linear regression was used to estimate the associations between vWF activity and measures of RV structure and function after adjusting for demographics, anthropometrics, smoking, diabetes mellitus, hypertension, and the corresponding left ventricular parameter. The average vWF activity was 140.7 ± 57.2%. Elevated vWF activity was independently associated with lower RV mass, RV end-diastolic volume, and RV stroke volume in models with and without adjustment for the corresponding left ventricular parameter (all p values <0.05). There was no association observed between vWF activity and the RV ejection fraction. In conclusion, higher vWF activity is associated with lower RV mass, RV end-diastolic volume, and RV stroke volume. These associations are independent of common cardiovascular risk factors and left ventricular morphologic changes.
Von Willebrand factor (vWF) is principally released by endothelial cells and mediates the initiation and progression of thrombus formation via platelet aggregation at a site of vascular injury. vWF reflects endothelial dysfunction, which can both influence and be affected by left ventricular (LV) dysfunction. Elevated vWF predicts poor prognosis in several diseases, including heart failure, hypertension, and coronary artery disease. Previous work by our group has suggested an independent association between vWF and mortality in patients with pulmonary arterial hypertension. We have also shown that elevated vWF activity is associated with a lower right ventricular (RV) ejection fraction (RVEF) in patients with pulmonary arterial hypertension. As a marker of endothelial dysfunction, vWF may reflect pulmonary vascular disease severity. However, the relation between vWF and RV structure and function has not been studied in adults free of cardiovascular disease. A better understanding of the relation of vWF with RV structure and function in adults without pulmonary hypertension may help clarify the cardiac role of vWF in disease. We examined the relation of vWF and measures of RV structure and function in a multiethnic cohort of adults free of clinical cardiovascular disease. We hypothesized that elevated vWF activity would be associated with greater RV mass, larger RV end-diastolic volume (RVEDV), and decreased RVEF.
Methods
The Multi-Ethnic Study of Atherosclerosis (MESA) is a multicenter, prospective cohort study designed to investigate the prevalence, correlates, and progression of subclinical cardiovascular disease in whites, African Americans, Hispanics, and Chinese Americans. From 2000 to 2002, MESA recruited 6,814 men and women aged 45 to 84 years from 6 United States communities: Forsyth County, North Carolina; Northern Manhattan and the Bronx, New York; Baltimore City and Baltimore County, Maryland; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles, California. Exclusion criteria were clinical cardiovascular disease (physician diagnosed heart attack, stroke, transient ischemic attack, heart failure, angina, current atrial fibrillation, any cardiovascular procedure), weight >136 kg (300 lb), pregnancy, or impediment to long-term participation. The institutional review boards of all participating institutions and the National Heart, Lung, and Blood Institute approved the protocols of MESA and all studies described herein. The MESA-Right Ventricle Study, which includes the present investigation, is an ancillary study focused on RV morphology in MESA participants eligible for magnetic resonance imaging at the baseline examination.
The cardiac magnetic resonance imaging protocol has been previously described, and methods for interpretation of LV and RV parameters have been previously reported. Cardiac magnetic resonance imaging examinations were transmitted to the reading center at Johns Hopkins University in Baltimore, Maryland, and image analysis was performed by 2 independent analysts using QMASS software (Medis Medical Imaging, Leiden, The Netherlands). Images were magnified to 250%, contrast and brightness were set to 55, and window width and level were set with the QMASS auto function.
Endocardial and epicardial borders of the right ventricle were manually traced on short-axis cine images at end-systole and end-diastole. Correct placement of RV contours relied on the evaluation of cine images to determine the demarcation between the right atrium and the right ventricle. Contours were modified at basal cardiac slices by careful identification of the tricuspid valve to exclude the right atrium and to avoid overestimation of the volumes. The outflow tract was included in the RV volume. Papillary muscle and trabeculae were included in the RV volumes and excluded from RV mass, as is commonly done for LV mass. RV end-systolic volume and RVEDV were calculated using Simpson’s rule by summation of areas on each slice multiplied by the sum of slice thickness and image gap. RV mass was determined at end-diastole as the difference between epicardial and endocardial volumes of the RV free wall multiplied by the specific gravity of the heart (1.05 g/mL). RV stroke volume (RVSV) was calculated by subtracting RV end-systolic volume from RVEDV. RVEF was calculated by dividing RVSV by RVEDV. The intrareader intraclass correlation coefficient for RV mass was 0.94 (229 scans), for RVEDV was 0.99 (230 scans), and for RVEF was 0.89 (230 scans). The blinded interreader intraclass correlation coefficients on 240 scans for RV mass, RVEDV, and RVEF were 0.89, 0.96, and 0.80, respectively.
Fasting blood samples were drawn, processed, and stored using standardized procedures. The MESA parent study originally measured baseline vWF in 1,000 participants, of whom 733 also had RV data from cardiac magnetic resonance imaging. We selected 1,290 additional participants with sufficient plasma and available RV data for measurement of vWF. vWF activity was measured in the Laboratory for Clinical Biochemistry Research at University of Vermont in Burlington. vWF activity was measured by the Liatest (latex immunoturbidometric) assay on the STA analyzer (Diagnostica Stago, Parsippany, New Jersey). In this assay, the degree of agglutination (measured by light absorption) between vWF in the sample and vWF monoclonal antibody in the assay is directly proportional to vWF activity. The intra-assay and interclass coefficients of variation were 3.7% and 4.5%, respectively.
Race and ethnicity were self-reported during the baseline MESA examination according to 2000 United States census criteria. Height was measured to the nearest 0.1 cm with the subject in stocking feet, and weight was measured to the nearest pound with the subject in light clothing using a balanced scale. Hypertension was accounted for with systolic blood pressure and current use of antihypertensive medication. Presence of diabetes mellitus was based on self-reported physician diagnosis, use of medication for hyperglycemia, or fasting glucose value ≥126 mg/dl, measured by rate reflectance spectrophotometry (Johnson & Johnson Clinical Diagnostics, Inc., Rochester, New York). Fasting glucose of 100 to 125 mg/dl was considered impaired fasting glucose. Smoking was classified as current, past, or never. Spirometric and computed tomographic lung density measures of percentage emphysema were available for a subset of participants. Flow-mediated dilation (FMD) as a marker of systemic endothelial dysfunction has been previously described. The brachial artery was occluded by a sphygmomanometer at a pressure of 50 mm Hg above systolic blood pressure for 5 minutes. Maximal brachial artery dilation over the last 2 minutes of this occlusion was recorded. Percentage FMD (%FMD) was the maximum brachial artery diameter minus the baseline diameter divided by the baseline diameter expressed as a percentage. The MESA Typical Week Physical Activity Survey has been previously described and includes intentional exercise as the sum of METs from activities that were consciously done for exercise. Intentional exercise was most strongly associated with LV structure and function.
We used linear regression to characterize the relation between vWF and RV parameters. Covariables were chosen on the basis of known associations with ventricular size, heart disease, and co-morbidities. In limited models, we adjusted for age, gender, race/ethnicity, height, weight, and study site. Adjustment for height and weight avoided the assumptions made in indexing the RV measures to certain parameters of body size (e.g., body surface area), while achieving the same end of accounting for differences in body size between participants. In fully adjusted models, we included smoking, hypertension, diabetes mellitus, cholesterol, impaired glucose tolerance, systolic blood pressure, treatment for hypertension, and C-reactive protein. We then adjusted the RV mass analysis by LV mass, the RVEDV analysis by LV end-diastolic volume, and the RVEF analysis by the LV ejection fraction to evaluate for independence from LV abnormalities (e.g., increased LV mass causing pulmonary venous hypertension leading to increased RV mass) and to better account for differences in body size. Because RVSV and LV stroke volume are interdependent, we adjusted for LV mass in this case. In separate analyses, we adjusted for intentional exercise, lung function (forced expiratory volume in 1 second, forced vital capacity, and percentage emphysema on chest computed tomography) (n = 1,826) and %FMD (n = 1,620). Generalized additive models were used to assess possible nonlinearity in the associations between vWF and RV parameters. Statistical significance was defined as p <0.05. Analyses were performed using Stata version 11.0 (StataCorp LP, College Station, Texas). We anticipated 99% power to detect a difference of 0.3 standard deviations in RV mass, volumes, and ejection fraction from the top quintile to the bottom quintile of vWF in the full sample.
Results
There were 6,814 men and women enrolled in MESA ( Figure 1 ). Of them, 5,098 underwent cardiac magnetic resonance imaging, and 5,004 (98%) had interpretable examinations for the left ventricle. We selected 4,634 scans and attempted reads in 4,484 scans before reaching our goal of 4,204 participants with successful RV interpretations (94% of 4,484 attempted). vWF was available for 2,011 of these participants. Thirty-five participants were excluded for missing covariates, leaving 1,976 in the study sample. Table 1 shows characteristics of the study sample compared to those excluded. The mean age was 60.2 years, and 47.2% were men. Compared to MESA participants not included in the analysis, the study sample was slightly younger, with a slightly lower prevalence of hypertension and diabetes. The mean RV mass in the sample was 21.4 ± 4.4 g, the mean RVEDV was 127.2 ± 31.5 ml, and the mean RVSV was 88.7 ± 20.9 ml. The mean RVEF was 70.2 ± 6.6%. All analyses were adjusted for height and weight (accounting for differences in body size), so that indexing to certain measures (e.g., body surface area) was not necessary and was not performed.

| Variable | Study Sample | Excluded |
|---|---|---|
| (n = 1,976) | (n = 4,838) | |
| Age (years) | 60.2 ± 9.9 | 62.9 ± 10.3 |
| Men | 47.2% | 47.1% |
| Race/ethnicity | ||
| White | 43.3% | 36.5% |
| Chinese | 10.9% | 12.1% |
| African American | 25.6% | 28.6% |
| Hispanic | 20.1% | 22.7% |
| Educational attainment | ||
| No high school degree | 14.5% | 19.5% |
| High school degree | 16.2% | 19.0% |
| Some college | 16.6% | 16.2% |
| Bachelor’s degree | 19.7% | 16.2% |
| Higher than bachelor’s degree | 22.0% | 16.4% |
| Height (cm) | 167.0 ± 10.1 | 166.1 ± 10.0 |
| Weight (kg) | 77.8 ± 16.6 | 79.0 ± 17.6 |
| Body mass index (kg/m 2 ) | 27.8 ± 5.0 | 28.6 ± 5.7 |
| Cigarette smoking status | ||
| Never | 52.1% | 49.6% |
| Former | 35.2% | 37.2% |
| Current | 12.7% | 13.2% |
| Hypertension | 40.6% | 46.6% |
| Systolic blood pressure (mm Hg) | 123.6 ± 20.2 | 127.8 ± 21.9 |
| Diastolic blood pressure (mm Hg) | 71.7 ± 10.1 | 72.0 ± 10.3 |
| Diabetes mellitus | 10.4% | 14.9% |
| vWF activity (%) | 140.7 ± 57.2 | 145.2 ± 57.5 ⁎ |
⁎ Three hundred nine subjects with measured vWF were not included in the study sample because of missing magnetic resonance imaging or covariates.
vWF was independently associated with RV mass ( Table 2 , Figure 2 ). Higher vWF was associated with lower RV mass. This relation was not meaningfully altered by adjustment for cardiovascular risk factors or LV mass. Adjustment for intentional exercise, %FMD (n = 1,620; as a proxy for systemic endothelial function), or lung function (forced expiratory volume in 1 second, forced vital capacity, and radiographic percentage emphysema) (n = 1,826) did not alter the relation between vWF and RV mass in participants with these measures ( Table 3 ).
| RV Parameter | Per 50% Increase in vWF Activity | ||
|---|---|---|---|
| Coefficient | (95% Confidence Interval) | p Value | |
| Mass (g), limited model | −0.2 | (−0.4 to −0.1) | <0.001 |
| Mass (g), adjusted model | −0.2 | (−0.4 to −0.1) | <0.001 |
| Mass (g), adjusted model + LV mass | −0.2 | (−0.4 to −0.1) | <0.001 |
| End-diastolic volume (ml), limited model | −1.2 | (−2.1 to −0.4) | 0.005 |
| End-diastolic volume (ml), adjusted model | −1.2 | (−2.1 to −0.4) | 0.005 |
| End-diastolic volume (ml), adjusted model + LV end-diastolic volume | −0.7 | (−1.3 to −0.1) | 0.03 |
| Stroke volume (ml), limited model | −0.8 | (−1.4 to −0.1) | 0.02 |
| Stroke volume (ml), adjusted model | −0.7 | (−1.4 to −0.1) | 0.02 |
| Stroke volume (ml), adjusted model + LV mass | −0.6 | (−1.2 to 0.0) | 0.04 |
| Ejection fraction (%), limited model | 0.1 | (−0.1 to 0.3) | 0.4 |
| Ejection fraction (%), adjusted model | 0.1 | (−0.1 to 0.4) | 0.4 |
| Ejection fraction (%), adjusted model + LV ejection fraction | 0.1 | (−0.1 to 0.3) | 0.4 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


