Video-Assisted Thoracic Surgery as a Diagnostic Tool
Anthony P. C. Yim
Alan D. L. Sihoe
F. Pons
Many advances have been made in the field of video-assisted thoracic surgery (VATS) since the last edition of this book. The use of VATS as a diagnostic tool for pleural diseases, solitary pulmonary nodules, and interstitial lung diseases has now been well accepted in mainstream thoracic surgery. Its role as an adjunct in lung cancer staging and in selected cases of chest trauma is becoming increasingly appreciated. However, alongside this technologic advance in surgery, we have also witnessed the rapid development of various imaging modalities for diagnosing a variety of chest diseases. The use of low-dose helical computed tomography (CT) of the thorax for lung cancer screening poses a challenge to the clinicians to best select patients for a surgical biopsy. Positron emission tomography (PET) has already made an impact on tumor staging and patient selection for resection. Newer diagnostic modalities like monoclonal antibody scans, somatostatin receptor scans, and antisense imaging techniques are likely to enhance the physician’s diagnostic ability further. Therefore, although surgical histology remains a cornerstone for diagnostic confirmation, readers are reminded that clinical management algorithms may need to be continually updated in the face of such rapid evolution in surgical, radiologic, and medical technology. The role of VATS in such algorithms similarly needs constant review and revision.
The objective of this chapter is to give an overview of the current applications of VATS in the diagnosis of chest disease and to define its role in modern thoracic investigative algorithms.
Background
The human body contains two noncommunicating pleural spaces. In contrast, elephants are born with physiologic pleural symphysis and essentially no pleural space at all. Other mammals, such as horses and buffalos, have extensive communications between the right and left thoracic spaces, effectively giving them a single pleural cavity. It is fortuitous that the anatomy in humans allows for single-lung collapse using selective one-lung anesthesia, affording ample room in the pleural cavity for instrument maneuvering during surgery, as emphasized by Kirsch.40 Because carbon dioxide insufflation is generally unnecessary for lung collapse, valved ports and dedicated endoscopic instruments are not mandatory. We are therefore blessed in having an ideal cavity for minimal-access thoracic surgery.
Many detailed reviews on the history and development of thoracoscopy have already been written, such as that by Braimbridge,7 and we shall not duplicate them in detail here. It is perhaps sufficient to note that thoracoscopy itself is an established technique, used for more than a century for adhesiolysis (to complement collapse therapy in tuberculosis management) and for simple pleural biopsy. Although the birth of thoracoscopy is generally credited to Hans Christian Jacobeus, a Swedish internist of the early twentieth century, recent evidence, as recorded by Hoksch and colleagues,33 suggests that this technique may have existed even half a century earlier. Much of the early use of thoracoscopy was for the diagnosis of intrathoracic diseases. However, it was the introduction of high-resolution video-endoscopic systems in the 1980s and of modern techniques of selective single-lung ventilation that revolutionized thoracic surgery. The fusion of these newer elements greatly enhanced the application of the old technique of thoracoscopy in the management of chest disease, evolving into VATS as we know it today. The role of VATS as a diagnostic tool for chest diseases is now well established in modern clinical practice.
Basic Technique
For general VATS diagnostic procedures, we prefer general anesthesia with selective one-lung ventilation using a double-lumen endotracheal tube. A single-lumen endotracheal tube with a bronchial blocker is an acceptable alternative, particularly for a patient with a small trachea. In young children for whom no suitably sized double-lumen tube is available, we use a single-lumen tube with the tip placed into the contralateral mainstem bronchus.
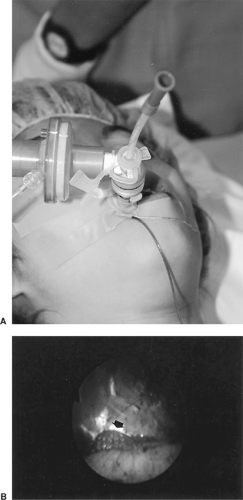
We have recently begun employing a novel method of highly selective lobar lung collapse for VATS in selected adult patients with compromised respiratory function. A similar technique using balloon catheter blockade of a targeted lobar bronchus was described by Takahashi and associates74 for children and later by Morikawa and colleagues55 for adults. Our method uses a fiberoptic bronchoscope to guide placement of a standard nasogastric feeding tube to the bronchial orifice of the target lobe (Fig. 19-1). The tube is left open to air or connected intermittently to low suction to expedite lobar collapse.
The patient is turned to a full lateral decubitus position and the table flexed to widen the rib spaces on the operation side, as the senior author emphasized in 1995.85 The positions of the surgeon and assistant depend on the site of the pathology as suggested by preoperative imaging. The surgeon stands facing the site of the pathology with the camera-holding assistant on the same side. The television monitor is positioned so that the surgeon, the site of pathology, and the monitor are aligned to allow the surgeon to look straight ahead when operating. Five- or 10-mm thoracoscopes are used with a 0- or 30-degree lens and a three-chip CCD video camera. Prewarming the thoracoscope with a sterile hot-water bath effectively prevents fogging of the lens (which can result from temperature differences when it is first inserted into the chest).
Intercostal port placement is described by Landreneau and colleagues.42 This baseball-diamond pattern allows for the comfortable “triangulation” of the instruments, enabling them to target the lesion site from either side. For general exploration, the first (camera) port is often made in the midaxillary to anterior axillary line at the seventh or eighth intercostal space. This first port is always made bluntly, and digital exploration is performed to detect and release adhesions around the port site before camera insertion. Generally, a 10-mm camera is used for adults and a 5-mm camera for children. The remaining two instrument ports are made under video guidance.
The authors prefer the use of standard conventional instruments, such as sponge-holding forceps, for nontraumatic lung manipulation. Rotation or tilting of the operating table can facilitate visualization by allowing the lung to drop away from the area to be examined. Pulmonary biopsies are taken using standard endoscopic staplers. An alternative technique is the enucleative precision cautery resection first described by Perelman and later advocated by Cooper and colleagues.15
One recent development in this regard is the technology of saline-enhanced thermal sealing, which employs a continuous flow of electrically conductive saline between the tissue and the diathermy electrode to translate the electrical energy of the diathermy into thermal energy in the tissue. This has been reported by one of us and associates.99 This achieves hemostasis and pneumostasis in the tissue, but the peak temperatures involved are significantly less than with direct conventional diathermy, resulting in less char formation, smoke generation, and lateral thermal damage to the adjacent tissue (hence reducing the potential for blood vessel perforation). The technology has been incorporated into a floating-ball device to allow nodulectomy by a modified Perelman technique (Fig. 19-2A). The technology has also been used in a bipolar sealing forceps, which functions similarly to an endoscopic stapling device for wedge resections (Fig. 19-2B), with the advantage of minimizing the consumable costs of reloadable cartridges for the stapler. Randomized studies comparing this technology with conventional staples are under way.
At the end of the procedure, the authors normally leave in a single chest tube (20–24 Fr) overnight. Some authors, such as Russo and colleagues,66 advocate even sooner removal of the chest tube.
There is a trend toward the use of ever smaller thoracoscopes for simpler procedures to minimize access trauma further. Thoracoscopes and instruments of 2-mm diameter (i.e., needlescopic instruments) have been used for thoracodorsal sympathectomies for many years at the authors’ institution, and their use in thoracic diagnostic procedures is being explored, as noted by the senior author and coinvestigators.97,98 Lazopoulos and colleagues43 demonstrated 100% diagnostic accuracy with 0% mortality and morbidity in using 2-mm mini-VATS for intrathoracic diagnosis in 54 patients. Such needlescopic VATS procedures cause less pain and offer even better cosmesis than classic VATS. The authors use a simple underwater seal technique to detect air leaks on-table after our needlescopic VATS procedures, obviating the need for routine chest tube insertions,
as described by the senior author and his colleagues.100 However, the 2-mm fiberoptic lens generally offers an inferior video image compared with that of a 3-mm Hopkins rod lens. Some surgeons also report poorer control and “feel” through the 2-mm endoscopic instruments because of their flexibility. Hence, more experience on the part of the surgeon is demanded.
as described by the senior author and his colleagues.100 However, the 2-mm fiberoptic lens generally offers an inferior video image compared with that of a 3-mm Hopkins rod lens. Some surgeons also report poorer control and “feel” through the 2-mm endoscopic instruments because of their flexibility. Hence, more experience on the part of the surgeon is demanded.
 Figure 19-2. Endoscopic instruments incorporating the saline-enhanced thermal sealing technology. A: Floating-ball device. B: Bipolar sealing forceps (TissueLink Medical Inc., Dover, NH). |
A related but totally different technique is pleuroscopy (sometimes referred to as “medical pleuroscopy”), which can be performed using a sterile fiberoptic bronchoscope. The bronchoscope is usually inserted under local anesthesia through a chest drain tract into the pleural cavity or through a small chest incision. The scope can be placed through a truncated chest tube, which can then guide the tip of the endoscope to the area of interest, as suggested by one of us.94 The application of this technique is very limited, and we would reserve this procedure for the occasional frail or debilitated patient who cannot tolerate general anesthesia but for whom an accurate tissue diagnosis (usually a pleural biopsy) is nonetheless required.
Use of Video-Assisted Thoracoscopic Surgery as a Diagnostic Modality
Pleural Disease
Effusion
The normal human pleural space is a closed potential space containing only a minimal volume of fluid (usually less than 5 mL) similar in composition to tissue fluid. This pleural fluid normally allows the lung to glide smoothly on the chest wall during respiration. Under certain abnormal circumstances, the amount of this fluid can increase, giving rise to a pleural effusion (Table 19-1).
Table 19-1 Some Common Indications for Diagnostic VATS | ||
|---|---|---|
|
Conventional methods of diagnosing the pathology underlying an abnormal pleural effusion include imaging, thoracocentesis, and percutaneous pleural biopsy. However, each of these has its specific drawbacks and limitations. Imaging (including chest radiography, ultrasonography, and CT) is useful in detecting and localizing the effusion but cannot diagnose the underlying etiology. Imaging can, however, guide thoracocentesis or insertion of drainage catheters. Thoracocentesis provides biochemical, microbiological, and cytologic information regarding the effusion. A precise histologic diagnosis is rarely indicated for a transudative effusion as determined by Light’s criteria44; on the other hand, an exudative effusion calls for further investigation to exclude malignancy and tuberculosis, among others. This can be performed blindly as a bedside percutaneous procedure or with radiologic guidance for targeting loculated effusions. It has been estimated by Collins and Sahn14 that up to 75% of diseases presenting with pleural effusion can be diagnosed by analyzing the fluid tapped by thoracocentesis. It has been suggested that a positive diagnosis is more likely with diseases such as empyema thoracis, chylothoraces, and hemothoraces, which do not require a precise cytologic diagnosis. However, for diseases that require cytology for diagnosis, such as malignant pleural disease, the yield is much lower. Menzies and Charbonneau51 reported positive cytologic diagnosis rates from thoracocentesis of 45% to 80%, with rates for malignant mesothelioma as low as 20%.
Percutaneous pleural biopsy is typically performed using an Abrams needle. Using this technique to detect malignant disease, Rao61 and Canto10 and their colleagues reported positive diagnosis rates of only 38% to 67%. Tomlinson and Sahn,75 using the Abrams needle, reported only 54% to 75% positive diagnosis rates for tuberculosis. These relatively low sensitivity rates are not surprising given that many pleural lesions may be located on the mediastinal, diaphragmatic, or visceral pleural surfaces, which are inaccessible to the percutaneous approach.
The problem, therefore, is that at least 15% to 25% of pleural effusions may remain undiagnosed using the aforementioned nonsurgical techniques. Boutin and coworkers6 reported that 215 in a series of 1,000 pleural effusions remained undiagnosed using only the former techniques. Repeating thoracocentesis for those 215 patients with indeterminate effusions only marginally increased the yield. However, in the same 215 patients, thoracoscopy gave 96% diagnostic accuracy, suggesting that thoracoscopy and VATS may indeed be the ideal investigative tools for such situations.
VATS not only means that bigger, more representative biopsies can be undertaken but also allows for all of the pleural surfaces (including the mediastinal, diaphragmatic, and visceral pleura) to be fully visualized and accessible for biopsy. A large volume of literature has already been published during the past 15 to 20 years confirming that VATS consistently achieves positive diagnosis rates for indeterminate pleural effusions in 95% to 100% of cases. A 1991 meta-analysis by Menzies and Charbonneau51 of 1,500 cases of indeterminate pleural effusions worldwide confirmed that VATS provided 90% diagnostic accuracy with only 3% morbidity. The diagnostic effectiveness of VATS in pleural disease is perhaps even greater than that of an exploration by thoracotomy, given the superior ability of VATS to visualize the entire lateral chest wall.
The senior author and associates86 previously demonstrated that more than half of all indeterminate pleural effusions may be related to an underlying malignant disease. This relatively high incidence highlights the importance of thorough investigation of all such effusions. With the proven efficacy and low morbidity of VATS, there is a strong case for early aggressive investigation of such effusions surgically should nonsurgical techniques prove inconclusive. The use of VATS enables the surgeon to diagnose less common causes of indeterminate pleural effusions without difficulty. These include the location and repair of sources of persistent chylothorax and the close pleuroperitoneal fistulas associated with peritoneal dialysis, as reported by the senior author (A.P.Y.C.) and colleagues.101
For the diagnosis of pleural effusions of unknown origin, the basic three-port VATS technique described earlier is used. Representative parietal pleural biopsies can be undertaken with endoscopic biopsy forceps inserted through the instrument ports. Should dedicated biopsy forceps not be available, an acceptable alternative method is to circumscribe the suspected pleural lesion with a generous margin and then to peel off the disc of pleura, containing it with forceps. If it can immediately be determined that the effusion was due to malignant disease, one can elect to apply chemical pleurodesis by talc insufflation. Talc insufflation, as noted by the senior author and associates,95 can be given by blowing in talc through a wide-bore suction catheter placed into the pleural space using a 50-mL bladder syringe.
For the experienced VATS surgeon, the use of two ports (one for the camera, one for biopsy forceps) or even one port can be sufficient to obtain adequate pleural biopsy specimens should there be no major adhesions. For the one-port technique, the biopsy forceps can be inserted alongside the video thoracoscope through the same port to reach the target lesion. An alternative is the use of an operating telescope with an offset eyepiece plus a central working channel for the insertion of the biopsy forceps. In patients coming to an operation with a chest drain already in situ, the drain site wound can be used as the single port, avoiding extra incisions.
Pleural Space Infections
The natural history of a parapneumonic effusion follows a well-described sequence, classically progressing through exudative, fibrinopurulent, and then organized phases. The management of pleural space infections and parapneumonic effusions is consequently very dependent on timing, with early parapneumonic effusions responding well to drainage alone, whereas full-blown lung entrapment would require extensive decortication procedures, as described by the senior author.91
The major role of VATS in such clinical situations is therapeutic: breaking down loculations in the fibrinopurulent phase allows for adequate drainage of a unified cavity. VATS may have a minor secondary role as a diagnostic adjunct in these cases, yielding a greater mass of pleural fluid, pleural exudative tissue, pleural cortical peel, and even lung tissue for microbiological study than is produced by other nonsurgical investigations.
In developing countries, VATS may still play an important diagnostic role in patients with suspected pulmonary tuberculosis, as discussed by the senior author.95 Mycobacteria are notoriously difficult to culture; positive diagnosis often requires sizable specimens for microbiological study. VATS can prove useful in obtaining generous quantities of tissue for tuberculosis
microscopy and culture. Such biopsies can be performed in a dedicated diagnostic VATS procedure or, more commonly, as part of a therapeutic VATS decortication procedure for an established empyema.
microscopy and culture. Such biopsies can be performed in a dedicated diagnostic VATS procedure or, more commonly, as part of a therapeutic VATS decortication procedure for an established empyema.
For cases of pleural space infections, the same basic three-port technique as described previously is used. For empyema thoracis, the authors prefer to site ports close enough together that fingers passed through any two ports can touch inside the chest. Using this bidigital technique, dense adhesions and loculations can be broken down around the ports, allowing greater room for exploration by the video thoracoscope. This is the same VATS technique employed in reoperated chests, as described by one of us and colleagues.96 For diagnostic purposes, aspirated pleural fluid and exudative peel from the parietal or visceral pleural surfaces are submitted for microbiological and pathologic studies. In areas where tuberculosis is still endemic, microbiological studies to exclude acid-fast bacilli are also mandatory.
Mesothelioma
Malignant mesothelioma can be notoriously difficult to diagnose. In its early stages, it may not be detectable even on CT scanning. Even if pleural thickening is seen on CT, it is often situated on the mediastinal, diaphragmatic, or costophrenic angle parietal pleura, which are not amenable for percutaneous needle biopsy. Any such biopsy would still be a blind procedure, yielding only small quantities of tissue, which may be insufficient for the histopathologist to make the difficult distinction between a malignant mesothelioma and metastatic adenocarcinoma. In cases where a fluid effusion is present, the diagnostic yield of fluid cytology from a diagnostic tap can be as low as 4% to 20%.
VATS is able to access all parts of the pleura, yielding generous biopsy specimens with high diagnostic yield. In 1979, Boutin and colleagues5 reported that thoracoscopy could yield a 94% positive diagnosis rate in cases of mesothelioma, compared with only 40% with percutaneous biopsies. In 1991, Sgro and coworkers68 achieved an 85.7% positive diagnosis rate. Grossebner and colleagues32 used VATS to confirm malignant mesothelioma in 23 of 25 patients suspected clinically of having the disease.
Diffuse Interstitial Lung Disease
The appearance of diffuse pulmonary infiltrates on radiologic imaging presents a diagnostic challenge for most clinicians, given the great variety of possible etiologies with a similar radiologic appearance.
Sputum analysis and bronchoalveolar lavage can yield positive cytologic and microbiological results. However, in more than half of all cases, the diagnosis remains elusive, as noted by Gaensler and Carrington.28 Percutaneous biopsy techniques are of limited value in this group of patients owing to the small size of the specimens generally obtained. In particular, some pathologies (such as pulmonary lymphoma) require special staining and cellular architectural analysis for identification and cannot be diagnosed from the small biopsy specimens these techniques provide.
Traditionally, the diagnostic procedure of choice was the open-lung biopsy. This can be performed through a limited thoracotomy without video assistance. Several studies have reported a positive diagnosis rate of more than 90% for diffuse lung infiltrative disease with open-lung biopsy. Nonetheless, before the advent of VATS, the morbidity and pain of a thoracotomy often deterred clinicians from performing lung biopsies until late in the course of the disease.
In modern practice, VATS has gradually replaced open-lung biopsy in most cases by virtue of its lower morbidity, leading to reduced postoperative morbidity and pain to the patient. It has also been shown in many studies that the size and quality of the biopsy from VATS is not inferior to that obtained by the open procedure. Rena and associates,63 for example, achieved 100% diagnostic accuracy using VATS for 58 patients with diffuse interstitial lung disease, with only two complications (both prolonged air leaks) and only one conversion to minithoracotomy because of pleural symphysis. Caccavale and Lewis’s9 review of 61 patients undergoing VATS biopsy for diffuse lung infiltrates achieved a 100% diagnostic rate at a cost of only two complications (both prolonged air leaks).
Numerous studies during the past decade have also compared VATS favorably with open-lung biopsy for the diagnosis of diffuse pulmonary infiltrates in terms of relative patient morbidity. Ferguson22 reported that VATS involved significantly shorter hospital stays when used for diagnosis of diffuse lung disease compared with open biopsy. Bensard and coauthors4 conducted a retrospective study comparing 21 patients undergoing open-lung biopsy with 22 undergoing VATS biopsy. Diagnostic accuracy was essentially the same in both groups, but the VATS patients enjoyed a lower complication rate (2 of 22 versus 4 of 21), shorter mean duration of chest drainage (1.4 days versus 3.2 days), and shorter hospital stay (2.6 days versus 5.7 days). Ferson and associates23 also demonstrated that, compared with open-lung biopsy, VATS lung biopsy offered significantly shorter hospital stays and fewer complications. A 1995 study by Kadokura and colleagues38 also concluded that VATS offered similar if not better results as compared with open-lung biopsy, with comparable complication rates, and that VATS was thus a satisfactory alternative. In 1998, Ravini and colleagues62 retrospectively compared 65 patients who underwent VATS biopsy for diffuse lung disease with 68 who underwent open-lung biopsy. Specimen adequacy and diagnostic accuracy were equivalent in both groups, but the VATS patients enjoyed significantly less blood loss, reduced postoperative analgesic requirements, and shorter postoperative stays. A prospective randomized trial by Ayed and Raghunathan3 compared 32 patients having VATS biopsy for diffuse lung disease to 29 patients undergoing open biopsy. The diagnostic yield in the two groups was comparable, but the VATS procedure gave significantly shorter operating times, reduced postoperative analgesic requirement, and reduced duration of hospital stay. There was also a trend for VATS patients to have a lower complication rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree