Chapter 107
Vertebral Artery Disease
Mark D. Morasch
Atherosclerosis and other vasculopathies involving the vertebrobasilar system are known to cause symptoms of posterior circulation ischemia. Approximately 25% of ischemic strokes occur in the vertebrobasilar territory. The vertebrobasilar system supplies blood to the brainstem, cerebellum, and occipital lobes via paired vertebral arteries. Brainstem ischemia, most often the result of atherosclerotic disease involving the vertebrobasilar arteries, remains poorly understood, and misdiagnosis is common. In contradistinction to the clear focal symptoms of anterior circulation ischemia, the symptoms associated with brainstem ischemia can be multiple, varied, and vague. Furthermore, a number of medical conditions may mimic vertebrobasilar ischemia, thus confounding the selection of patients in need of posterior circulation intervention (see Chapter 97). Consequently, clinicians appear to be reluctant to aggressively pursue diagnosis or recommend treatment for many of the surgically correctable lesions that may be responsible for these syndromes.
Vertebrobasilar ischemia is less common than internal carotid artery disease, yet it must be diagnosed appropriately because it is a treatable vasculopathy. Significantly, 50% of patients will initially be evaluated for stroke and 26% for transient ischemic symptoms rapidly followed by stroke.1 For patients who experience vertebrobasilar transient ischemic attacks, disease in the vertebral arteries portends a 22% to 35% risk of stroke over a 5-year period.2–4 The mortality associated with a posterior circulation stroke is 20% to 30%, higher than that for an anterior circulation event.5–7
Pathogenesis
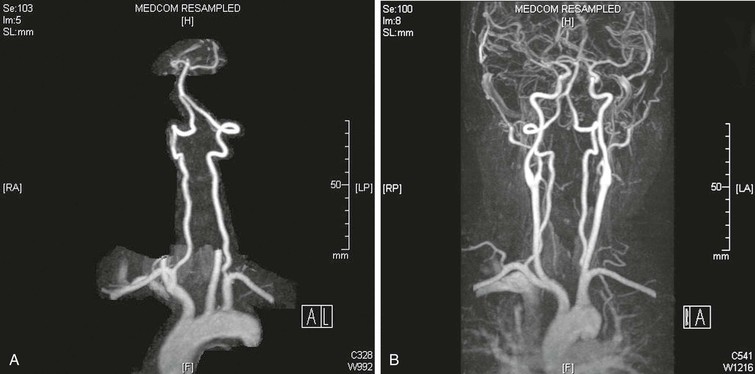
One reason the pathophysiology of vertebrobasilar ischemia is less well understood than that of carotid/anterior hemispheric ischemia is that the peculiar anatomy of the vertebral artery makes it less accessible to surgical reconstruction and postmortem examination. The surgical anatomy of the paired vertebral arteries has traditionally been divided into four segments: V1, the origin of the vertebral artery arising from the subclavian artery to the point at which it enters the C6 transverse process; V2, the segment of the artery buried deep within intertransversarium muscle and the cervical transverse processes of C6 to C2; V3, the extracranial segment between the transverse process of C2 and the base of the skull before it enters the foramen magnum; and V4, the intracranial portion beginning at the atlanto-occipital membrane and terminating as the two vertebral arteries converge to form the basilar artery (Fig. 107-1).
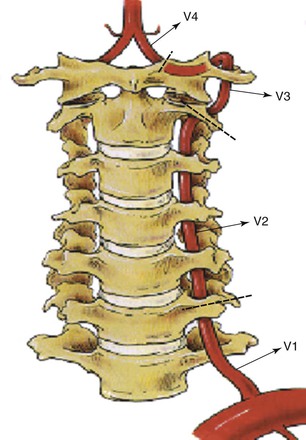
Figure 107-1 The four segments of the vertebral (V) artery. (From Berguer R: Surgical management of the vertebral artery. In Moore WS, editor: Surgery for cerebrovascular disease, New York, NY, 1986, Churchill Livingstone.)
Ischemia affecting the temporo-occipital areas of the cerebral hemispheres or segments of the brainstem and cerebellum characteristically produces bilateral symptoms. The classic symptoms of vertebrobasilar ischemia are dizziness, vertigo, drop attacks, diplopia, perioral numbness, alternating paresthesia, tinnitus, dysphasia, dysarthria, and ataxia. When patients have two or more of these symptoms, the likelihood of vertebrobasilar ischemia is high (Box 107-1). Posterior circulation strokes occur most commonly in relation to large-artery occlusive diseases (Table 107-1). The vertebral artery is the most common large vessel to be involved with an occlusive lesion that leads to stroke (Table 107-2).
Table 107-1
Mechanisms of Posterior Circulation Stroke or Transient Ischemic Attack in 407 Patients
| Mechanism | Number (%) |
| Large-artery occlusive disease | 132 (32) |
| Embolism—cardiac source | 99 (24) |
| Embolism—arterial source | 74 (18) |
| Penetrating artery disease | 58 (14) |
| Vasospasm/migraine | 10 (2) |
| Other causes | 34 (8) |
Adapted from Caplan LR, et al: New England Medical Center Posterior Circulation registry. Ann Neurol 56:389, 2004.
Table 107-2
Frequency of Symptomatic Vascular Occlusive Lesions in 417 Patients
| Lesion | Number |
| Innominate artery | 2 |
| Subclavian artery | 5 |
| Extracranial vertebral artery | 131 |
| Intracranial vertebral artery | 132 |
| Basilar artery | 109 |
| Posterior cerebral artery | 38 |
Adapted from Caplan LR, et al: New England Medical Center Posterior Circulation registry. Ann Neurol 56:389, 2004.
The most common disease affecting the vertebral artery is atherosclerosis. Less common pathologic processes include trauma, fibromuscular dysplasia, Takayasu’s disease, osteophyte compression, dissections, aneurysms, and other arteritides.
Ischemic Mechanisms
In general, the ischemic mechanisms can be broken down into those that are hemodynamic and those that are embolic. The low-flow hemodynamic mechanism of ischemia is better recognized and more frequent than the embolic one.
Low Flow
Patients with low-flow hemodynamic ischemia have transient symptoms in the territory of the basilar artery because they lack appropriate inflow from the vertebral artery and have inadequate compensation from the carotid territory. Hemodynamic symptoms occur as a result of transient end-organ (brainstem, cerebellum, occipital lobes) hypoperfusion and can be precipitated by postural changes or a transient reduction in cardiac output. Ischemia from hemodynamic mechanisms rarely results in infarction. Rather, symptoms are short lived, repetitive, and more of a nuisance than a danger. Some patients may be prone to traumatic injuries from loss of balance. For hemodynamic symptoms to occur in direct relation to the vertebrobasilar arteries, significant occlusive disease must be present in both of the paired vertebral vessels or in the basilar artery. In addition, compensatory contribution from the carotid circulation via the circle of Willis must be incomplete. Alternatively, hemodynamic ischemic symptoms may result from proximal subclavian artery occlusion and the syndrome of subclavian/vertebral artery steal.
Embolic
Embolic causes of vertebrobasilar ischemia may not be as well recognized. Symptoms may be due to microembolization from the heart or aortic arch or, more frequently, from vessels directly leading to the basilar artery. Arterial-to-arterial emboli can arise from atherosclerotic lesions, from intimal defects caused by extrinsic compression or repetitive trauma, and rarely, from fibromuscular dysplasia, aneurysms, or dissections. Although fewer patients suffer from embolic phenomena than from hemodynamic mechanisms, actual infarctions in the vertebrobasilar distribution are most often the result of embolic events. When compared with the hemodynamic mechanisms of ischemia, emboli are much more likely to cause fatal events or dangerous or debilitating infarcts. It is estimated that up to a third of vertebrobasilar ischemic episodes are caused by distal embolization from plaque or mural lesions of the subclavian, vertebral, or basilar arteries (or any combination of these vessels).8 These patients may have transient ischemic attacks or strokes in the territory supplied by the basilar artery. The importance of the embolic mechanism as a cause of vertebrobasilar symptoms has been emphasized in clinical and anatomicopathologic studies. This information has been derived from autopsy studies and magnetic resonance imaging (MRI), which have identified small infarcts in the brainstem and cerebellum and shown their source, via arteriography, to be lesions in the subclavian or vertebral arteries. As opposed to patients with hemodynamic symptomatology, multiple and multifocal infarcts in the brainstem, cerebellum, and occasionally, the posterior cerebral artery territory often develop in patients with embolic ischemia.9,10
Patient Selection for Vertebral Artery Reconstruction
Anatomic Considerations
The minimal anatomic requirement to justify vertebral artery reconstruction for hemodynamic symptoms would be stenosis greater than 60% diameter in both vertebral arteries if both are patent and complete or the same degree of stenosis in the dominant vertebral artery if the opposite vertebral artery is hypoplastic, ends in a posteroinferior cerebellar artery, or is occluded. A single, normal vertebral artery is sufficient to adequately perfuse the basilar artery, regardless of the patency status of the contralateral vertebral artery. Unlike carotid artery disease, the mere presence of vertebral artery stenoses in an asymptomatic patient is rarely an indication for reconstruction because these patients are well compensated from the other vertebral or from the carotid circulation through the posterior communicating vessels.
Etiologic Considerations
Low Flow
For patients with hemodynamic symptoms, it is essential to rule out systemic causes of ischemia before advising evaluation of the vertebrobasilar arteries as the source of symptoms. In the later years of life, vertebral artery stenosis is a frequent arteriographic finding, and dizziness is a common complaint. The presence of both cannot necessarily be assumed to have a cause-effect relationship. The indication for intervention in patients with hemodynamic symptoms depends on the ability to demonstrate insufficient blood flow to the basilar artery. Other common systemic causes of hemodynamic ischemia, aside from vascular occlusion, include orthostatic hypotension, poorly regulated antihypertensive therapy, arrhythmias, heart failure, malfunction of pacemakers, and anemia.
Embolic
In contrast to individuals with low-flow states among patients with posterior circulation ischemia secondary to microembolism and appropriate lesions in a vertebral or subclavian artery, the potential source of the embolus needs to be eliminated regardless of the status of the contralateral vertebral artery. Patients with symptomatic vertebrobasilar ischemia secondary to emboli are candidates for surgical correction of the lesion irrespective of the condition of the contralateral vertebral artery. However, surgical intervention is not indicated in asymptomatic patients who harbor suspicious radiographic findings.
Global Ischemia
Another indication for vertebral artery reconstruction pertains to patients who have extensive extracranial disease with one or both internal carotid arteries occluded and global manifestations of cerebrovascular ischemia. In these patients the carotid arteries may be occluded or involved with severe siphon stenosis, thus making direct revascularization via the internal carotid arteries impossible or inadvisable, and reconstruction of the vertebral artery may offer the best option for reestablishment of adequate cerebral blood flow. In patients with global ischemia, the vertebral arteries are important pathways for cerebral revascularization when they are critically stenosed or occluded. Demonstration of normal-sized posterior communicating arteries increases the likelihood of successfully correcting global ischemic symptoms by vertebral artery reconstruction. Once the diagnosis of vertebrobasilar ischemia (or global ischemia requiring vertebral revascularization) has been confirmed and significant pathology identified radiographically, endovascular or surgical correction may be considered.
Differential Diagnosis
Identifying patients who can benefit from vertebral artery reconstruction begins with an accurate assessment of the symptom complex, followed by efforts to exclude other causes of the symptoms (Box 107-2). These other medical conditions include inappropriate use of antihypertensive medications, cardiac arrhythmias, anemia, brain tumors, and benign vertiginous states. A thorough investigation consists of ruling out (1) inner ear pathology, (2) cardiac arrhythmias, (3) internal carotid artery stenosis/occlusion, and (4) inappropriate use of medications (Box 107-3).
Evaluation of patients with posterior circulation ischemia should include assessment of the precise circumstances associated with the development of symptoms. Symptoms often appear on standing in older individuals with poor sympathetic control of their venous tone, which causes excessive pooling of blood in the veins of the leg. This is particularly common in patients with diabetes who have diminished sympathetic venoconstrictor reflexes. A 20-mm Hg drop in systolic pressure on rapid standing is a criterion for a diagnosis of orthostatic hypotension causing low flow in the vertebrobasilar system. In these cases the drop in pressure triggers the symptoms of posterior circulation ischemia.
Any systemic mechanism that decreases the mean pressure of the basilar artery may be responsible for hemodynamic symptomatology, and affected individuals may or may not have concomitant vertebral artery stenosis or occlusion. Because certain prescription medications can mimic vertebrobasilar ischemia, patient medications require thorough review. In fact, excessive use of antihypertensive medications is the most common etiology of posterior circulation symptoms and can also cause hemodynamic posterior circulation ischemia by decreasing perfusion pressure and inducing severe orthostatic hypotension.
A cardiac source is the second-most common cause of brainstem ischemia, especially in older adults, and thorough evaluation should include 24-hour Holter monitoring for arrhythmias and echocardiography to assess heart valve function. Arrhythmias are another common cause of symptoms as a result of decreased cardiac output. Patients with ischemia secondary to arrhythmias often report the association of palpitations with the appearance of symptoms. In addition, transesophageal echocardiography may be useful in patients with a suspected embolic mechanism of ischemia to rule out a cardiac source.
In some patients, the cause of the drop in mean arterial pressure can be corrected simply by readjusting their antihypertensive regimen, by the administration of antiarrhythmic drugs, or by inserting a cardiac pacemaker. In patients with orthostatic hypotension, the problem may not respond to medical treatment, and only reconstruction of a diseased or occluded vertebral artery will render the patient asymptomatic in the presence of persistent oscillations in blood pressure.
Investigation must also be undertaken to exclude inner ear pathology, including rare cerebellopontine-angle tumors. In addition, neurologic evaluation to rule out benign vertiginous states should be considered.
Because patients are often initially seen with a combination of anterior and posterior hemispheric symptoms, investigation of the great vessels and the carotid circulation is usually warranted. An important aspect of the history is identifying triggering events such as positional or postural changes. This is followed by a thorough physical examination, which includes palpation, auscultation, pulse examination, and comparative arm blood pressures (recumbent and standing).
Physical examination can alert the physician to the possibility of subclavian steal in patients with differences in brachial blood pressure greater than 25 mm Hg or with diminished or absent pulses in one arm. The diagnosis of reversal of vertebral artery flow can be made accurately by noninvasive indirect methods and demonstrated directly by duplex imaging of the reversal of flow in the vertebral artery (see Chapter 16 and Chapter 98).
Patients may relate their symptoms to turning or extending their head. These dynamic symptoms usually appear when turning the head to one side. Symptoms are caused by extrinsic compression of the vertebral artery, usually the dominant or the only one, by arthritic bone spurs.11 To differentiate this mechanism from dizziness or vertigo secondary to labyrinthine disorders that appear with head or body rotation, the patient should attempt to reproduce the symptoms by first turning the head slowly and then repeating the maneuver briskly, as when shaking the head from side to side. In labyrinthine disease, the sudden inertial changes caused by the latter (brisk) maneuver result in immediate symptoms and nystagmus. Conversely, with extrinsic vertebral artery compression, a short delay occurs before imbalance develops.
Diagnostic Tests
Once a suspicion of vertebrobasilar ischemia has been entertained, only a few diagnostic tests are available to clearly ascertain the vertebral anatomy.
Duplex Ultrasonography
Although duplex ultrasound is an excellent tool for detecting lesions in the carotid artery, it has significant limitations when used to detect vertebral artery pathology. Direct visualization of the second portion of the vessel is difficult because of its intraosseous course through the transverse processes of C2 to C6. The usefulness of duplex ultrasound lies in its ability to confirm reversal of flow within the vertebral arteries and detect changes in flow velocity consistent with a proximal stenosis.12 In addition, ultrasound imaging can diagnose great-vessel pathology and confirm subclavian steal.
Computed Tomography and Magnetic Resonance Imaging
MRI is another modality that provides a safe, noninvasive, detailed evaluation of both the extracranial and intracranial vasculature, as well as structures within the posterior fossa. Contrast-enhanced magnetic resonance angiography (MRA) with three-dimensional reconstruction and maximum image intensity techniques provides full imaging of the vessels, including the supra-aortic trunks and the carotid and vertebral arteries (Fig. 107-2).
Arteriography
Despite the technologic advances in MRI and CT evaluation, selective subclavian and vertebral angiography remains the “gold standard” for preoperative evaluation of patients with vertebrobasilar ischemia. Some surgeons still consider angiography mandatory before endovascular intervention or surgical reconstruction. The most common site of disease, the vertebral artery origin, may not be well imaged with ultrasound or magnetic resonance angiography and, in fact, can often be displayed only with oblique projections that are not part of the standard aortic arch evaluation. Patients with suspected vertebral artery compression should undergo dynamic angiography, which incorporates provocative positioning. Finally, delayed imaging should be performed to demonstrate reconstitution of the extracranial vertebral arteries through cervical collaterals.
Arteriographic investigation of vertebral artery pathology necessitates systematic positions and projections to evaluate the vertebrobasilar system from its origin to the top of the basilar artery. Arteriographic evaluation begins with an arch view, which determines the presence or absence of a vertebral artery on each side. Angiography shows whether one vertebral artery is dominant (generally the left) and can clearly define aberrant vessel anatomy. The most common anomalous origin involves the left vertebral artery, which can originate from the aortic arch in 6% of patients. A much rarer variant involves the right vertebral artery, which can be seen to arise from the innominate or right common carotid artery (Fig. 107-3). This anatomy usually occurs in patients with an aberrant retroesophageal right subclavian artery. Arch views must be obtained in at least two projections: right and left posterior oblique views. Usually, these two projections will sufficiently display the first segment (V1) of the vessel from its subclavian origin up to the transverse process of C6.

Figure 107-3 Arch injection in a 33-year-old woman with vertebrobasilar ischemia. A, The right vertebral artery and the right external carotid artery arise from a long common right carotid trunk (arrow). The right internal carotid artery is congenitally absent. The right subclavian arises as the last branch of the aorta. B, The right vertebral artery, which has an anomalous origin, enters the spine at a high level (C4) and is severely compressed (arrow) at this level with head rotation.
Disease Distribution
V1 Segment
The most common atherosclerotic lesion of the vertebral artery is stenosis of its origin. The prevalence of such lesions is approximately 20% to 40% in patients with cerebrovascular disease.8 This lesion may be missed in standard arch views because of superimposition of the subclavian artery over the first segment of the vertebral artery. Additional oblique projections may be needed to “throw off” the subclavian artery to obtain a clear view of the origin of the vertebral artery (Fig. 107-4). The presence of a poststenotic dilatation in the first centimeter of the vertebral artery suggests that there may be a significant stenosis at its origin hidden by an overlying subclavian artery. Redundancy and kinks are common, but only very severe kinks associated with poststenotic dilatations can be responsible for hemodynamic symptoms.
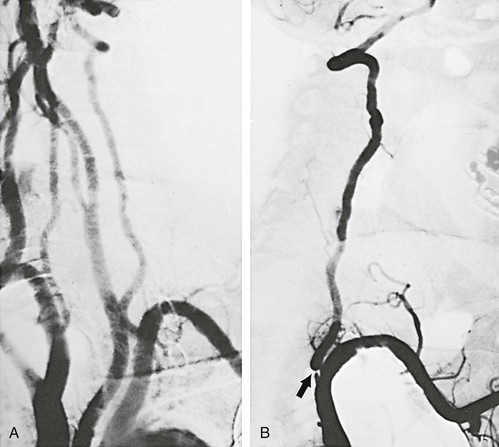
Figure 107-4 A, Arch arteriogram on anteroposterior projection. B, Severe stenosis (arrow) of a dominant left vertebral artery seen only after additional oblique rotation of the patient (right). (From Berguer R: Role of vertebral artery surgery after carotid endarterectomy. In Bergan JJ, et al, editors: Reoperative arterial surgery, Orlando, Fla, 1986, Grune & Stratton, pp 555-564.)
V2 Segment
Visualization of the second segment (V2) of the vertebral artery, from C6 to the top of the transverse process of C2, is accomplished in the oblique arch views in conjunction with selective subclavian injections. A point should be made to attempt to angiographically identify the point of entry of the vertebral arteries into the transverse processes of the spine. Whether a patient has an abnormally low entry at the level of C7 instead of C6 should be noted. This finding is associated with a short V1 segment of the artery. In this circumstance, the short extraosseous length can create challenges for reconstruction at the V1 level. In addition, extrinsic compression by musculotendinous structures is common in vertebral arteries with an abnormally high level of entry into the spine, usually C4 or C5 (see Fig. 107-2). Such compression is due to the sharp angulation resulting from the abnormal level of entry. The level of entry into the spine is best determined on unsubtracted views.
The most common pathology of the V2 segment is extrinsic compression of the vertebral artery by osteophytes,11 but compression can also be caused by the edges of the transverse foramina (Fig. 107-5) or the intervertebral joints. Positional changes or rotation or extension of the neck usually triggers compression of the vertebral artery in this segment. Arteriography is required to demonstrate extrinsic dynamic compression of the vertebral artery. This is performed either with the patient sitting up, by means of bilateral brachial injections, or if the transfemoral approach is used, with the patient supine in the Trendelenburg position with the head resting against a block. The reason to position the patient either sitting up or in a 25-degree Trendelenburg position is to mimic the effects of the weight of the head on the spine. With the patient standing, the weight of the head acting on the cervical spine changes its curvature and decreases the distance between C1 and C7. This longitudinal compression of the spine often enhances the extrinsic compression effects caused by osteophytic spurs. In these positions, intended to exert axial compression on the cervical vertebrae, the angiographer should obtain the specific rotation or extension of the head that provokes the symptoms. When the patient is rendered symptomatic, arteriographic injection should demonstrate the extrinsic compression that developed with the head rotation or extension.13 The vertebral artery may be normal in one projection and occluded by extrinsic compression in the other (Fig. 107-6). The agent of compression may be bone (an osteophyte) or tendon (longus colli).
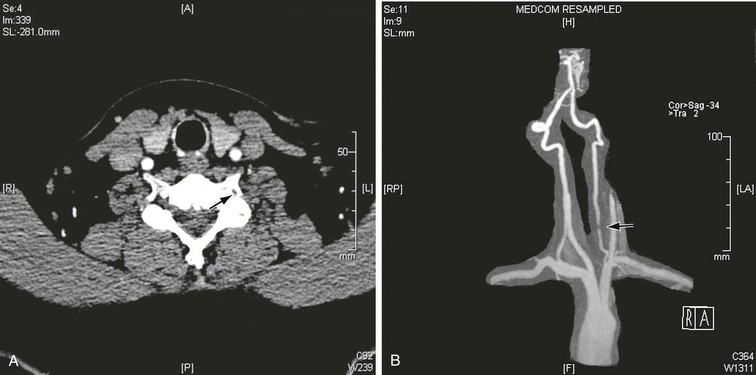
Figure 107-5 CT (A) and MRA (B) images demonstrating large osteophytes occluding the vertebral artery at C5.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree