Compared with anterior cerebral circulation ischemia, our knowledge regarding ischemia of the posterior cerebral circulation is more rudimentary. With improved technology that allows imaging of the brain and vascular lesions causing vertebrobasilar ischemia (VBI), this gap has closed and many misconceptions have been challenged.
Based on data from a well-characterized group of patients with signs and symptoms of posterior circulation ischemia (n = 407), the causes of VBI have been defined (1). Embolism is the dominant mechanism, accounting for approximately 40% of cases. Emboli may arise from the heart (usually thrombus), aorta (usually atheroma), or proximal vessel thrombus (predominantly the vertebral artery). Large artery disease, predominantly involving the vertebral artery, is the second most common mechanism accounting for approximately 32% of cases, with ischemia being produced on a hemodynamic basis or by occlusion of important penetrating or circumferential branches arising from the diseased vessel. The remaining cases are caused by a variety of conditions such as dissection, fibromuscular dysplasia, migraine, and rare arteriopathies that often involve the vertebral artery. These data highlight the importance of vertebral artery disease in causing posterior cerebral circulation ischemia, a phenomenon that has previously been underappreciated in clinical practice.
Atherosclerosis is the dominant pathology seen in the vertebral artery and has a predilection for the origin and proximal section of the extracranial (i.e., termed the V1 segment) and the intracranial portion of the vessel. The focus of this chapter will be on the interventional management of patients with proximal extracranial vertebral artery (ECVA) disease. Management of intracranial artery disease is discussed in Chapters 13A and 13B. Although it has generally been considered that ECVA disease has a more benign outcome compared to intracranial vertebral artery disease, significant occlusive disease of the proximal vertebral artery was present in 20% of patients who presented with VBI at a tertiary referral center and was felt to represent the primary cause of ischemia in 9% of patients (2).
ANATOMY
The vertebral artery typically arises from the superoposterior aspect of the first part of the subclavian artery and is usually the first branch of this vessel. In approximately 5% of patients, the left vertebral artery arises directly from the aortic arch, between the origin of the left common carotid and left subclavian arteries (Fig. 12.1).
Other rare anomalies have been described including origin directly from the aortic arch distal to the left subclavian artery, origin distal to the thyrocervical branch of the subclavian artery, origin of the right vertebral from the right common carotid artery, and duplication of the vertebral artery that may occur at any level of the artery (3).
The vertebral artery is arbitrarily divided into four anatomic parts (Fig. 12.2)
- V1—The portion extending from the origin to the point at which it enters the transverse foramina of either the fifth or sixth cervical vertebra.
- V2—The course within the intervertebral foramina until exiting at the level of the atlas (i.e., C2).
- V3—The extracranial segment between the transverse process of the C2 and the base of the skull, as it enters the foramen magnum.
- V4—The final intracranial portion that begins as it pierces the dura and arachnoid mater at the base of the skull and ends as it meets its opposite vertebral artery to form the midline basilar artery at the level of the medullopontine junction.
The intracranial part gives off major anterior and posterior spinal arteries to the medulla and spinal cord, minute penetrating vessels to the medulla, and the largest branch, the posterior inferior cerebellar artery (PICA), to a portion of the dorsal medulla and cerebellum. One of the vertebral arteries is often larger (i.e., left more frequently than right) and provides most of the blood supply to the posterior circulation (i.e., dominant artery). Stenosis of the dominant artery is more likely to cause symptoms.
CLINICAL PRESENTATION OF EXTRACRANIAL VERTEBRAL ARTERY DISEASE
Extracranial vertebral artery (ECVA) disease causing hemodynamic compromise typically produces dizziness accompanied by other signs of hind-brain ischemia (e.g., diplopia, hemiparesis, bilateral leg weakness, numbness) consistent with global ischemia of the posterior circulation (4,5). The nonspecific nature of a number of these symptoms, particularly in an elderly population, has contributed to the failure to associate vertebral artery disease and VBI.
Embolization from proximal vertebral atherosclerosis produces a variety of syndromes based on the site of distal embolization. The typical sites of embolization include the PICA, superior cerebellar artery (SCA), and posterior cerebral artery. Obstruction of circumferential arteries (e.g., PICA, SCA) results in typical lateral syndromes that affect cerebellar function, sensation, and lateral cranial nerves. In contrast, the clinical presentation following obstruction of midline perforator branches is highly variable. In general, midline syndromes tend to affect the pyramidal system, consciousness, and midline cranial nerves.
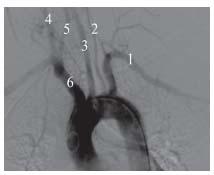
Figure 12.1 • Left vertebral artery arising directly from the aortic arch. 1. Left subclavian; 2. Left vertebral; 3. Left common carotid; 4. Right common carotid; 5. Right vertebral; 6. Innominate.
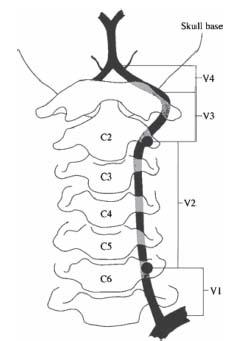
Figure 12.2 • Schematic of the four parts of the vertebral artery. (From Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM. 2003;96(1):27–54, by permission of Oxford University Press.)
PATIENT SELECTION
Considerable controversy surrounds the indications for endovascular intervention for occlusive disease of the ECVA. The reasons for this have been well described and are multiple (6). Relatively inexpensive, noninvasive testing with ultrasonography has been unreliable in this location. CT and MR angiography also have significant limitations, often resulting in the need for routine invasive angiography to help make a reliable anatomic diagnosis of disease. In contrast to the treatment of carotid bifurcation disease, there is an absence of an effective and safe surgical therapy for the treatment of proximal ECVA disease. These factors have contributed to a knowledge gap, with respect to vertebral artery disease and the potential for revascularization to alter the natural history of the disease.
Endovascular approaches to proximal ECVA disease have transformed approaches to therapy. In contrast to surgical revascularization, where surgical accessibility is particularly demanding and likely contributes to the very high morbidity and mortality rates for these procedures (i.e., approximately 20%) (7), endovascular access is straightforward, and the techniques of angioplasty and stenting are readily applied to the treatment of proximal ECVA stenoses. Although endovascular ECVA revascularization has been practiced at multiple centers for over two decades, the techniques continue to evolve, and currently available data are still derived from relatively small registries. Therefore, appropriate decisions regarding patient management remain hampered by a lack of data.
Despite these limitations, it is generally accepted that intervention is indicated in patients with symptomatic vertebral artery stenosis who fail or are intolerant of medical therapy. Intervention in patients with symptomatic disease without a trial of medical therapy is also probably justified, in view of the outcomes reported from observational studies. Decisions regarding intervention in asymptomatic patients are more uncertain. A thorough review of the clinical history and angiographic findings by a neurologist, together with the interventionist, is recommended. Factors that will influence the decision include the severity of the stenosis, the angiographic appearance of the stenosis (i.e., friability, presence of ulceration), the adequacy of collateral flow, and the age of the patient. A severe, ulcerated stenosis without good collateral flow, in a relatively young, asymptomatic patient may be approached after appropriate discussion with the patient.
ENDOVASCULAR INTERVENTION FOR ECVA DISEASE
Arterial Access
The choice of an appropriate arterial access site is crucial to performing safe and successful angiography, and intervention of the vertebral artery (4). Access is typically obtained using the retrograde common femoral artery (CFA) approach. Ipsilateral brachial artery access is considered in individuals with bilateral, severe, iliac artery stenosis or distal aortic occlusions. Brachial access may also be indicated in patients with severe tortuosity or stenosis of the proximal subclavian artery, Type III aortic arch anatomy, or an acute angulation of the origin and proximal segment of the vertebral artery. If brachial or radial artery access is used, 3000 to 5000 U of unfractionated heparin should be injected through the sidearm of the sheath immediately following sheath insertion to minimize the risk of thrombosis, and liberal use of intra-arterial vasodilators such as nitroglycerin (in 100 μg boluses), verapamil (100 to 200 μg boluses), or nitroprusside (100 to 200 μg boluses) is recommended to prevent spasm.
DIAGNOSTIC ANGIOGRAPHY
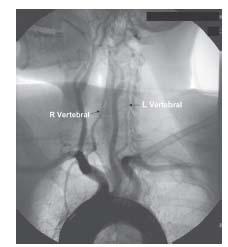
Arch Aortogram
Where possible, an arch aortogram should be performed prior to attempts at selective cannulation of the vertebral arteries (4). Arch aortography is typically performed in the LAO 30° to 45° projection, using an injection rate of 20 cc/sec for a total of 40 cc and a PSI limit of 1000. This allows an assessment of the complexity of the aortic arch, the origin of the great vessels from the arch, and some information about the origin of the vertebral arteries (Fig. 12.3).
Typical arch anatomy with separate origin of the brachiocephalic, left carotid, and left subclavian arteries is seen in more than 70% of cases. A shared origin of the brachiocephalic trunk and left common carotid artery is seen in 15% of cases, while a bovine arch (i.e., origin of the left common carotid artery from the brachiocephalic trunk) is seen in 8% to 10% of cases (Fig. 12.4).
Selective Vertebral Artery Angiography
When using femoral access, the initial goal of vertebral artery angiography is engagement of the innominate or left subclavian artery angiography. One should start with a catheter appropriate to the aortic arch type, rather than repeatedly scraping the arch with an inappropriate catheter that increases the risk of stroke and other procedural complications. In most patients, both the innominate and left subclavian arteries may be cannulated with a Bernstein, JB1, or Judkins® Right (JR4) catheter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


