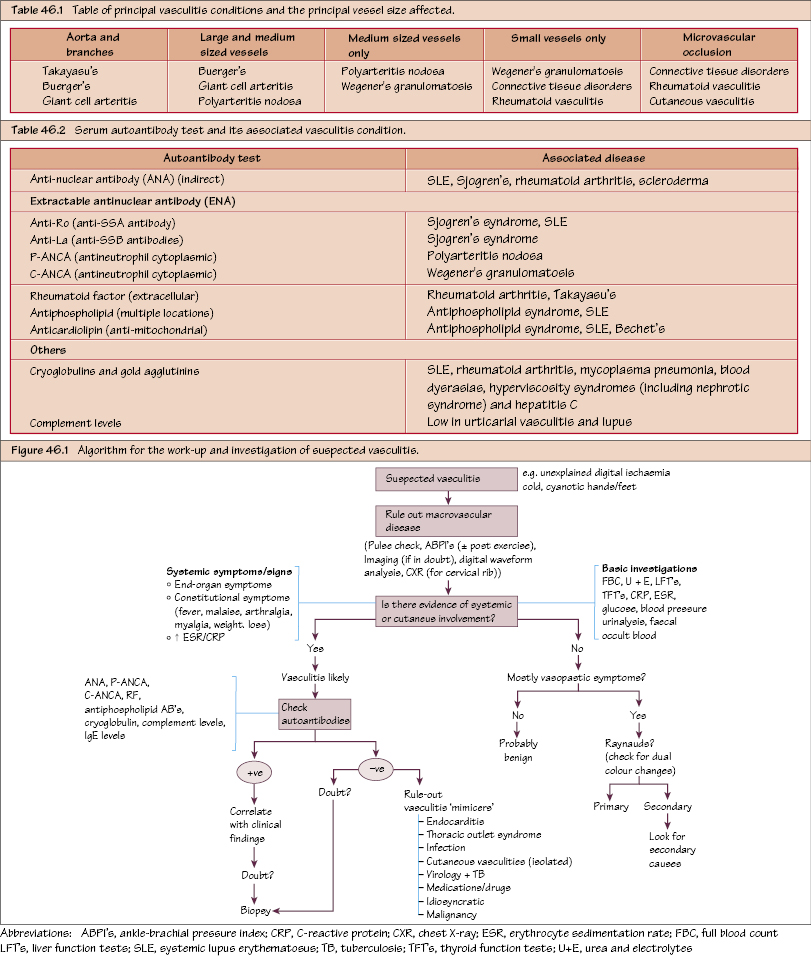
Vasculitis I: Overview Vasculitis is a spectrum of disorders characterised by acute and chronic inflammatory changes in the vessel wall. While the management of vasculitis is rarely surgical, many patients may present to a vascular service for an opinion on managing the ischaemic component. There are numerous disorders, most of whose aetiology is unknown. Long-term complications may include vessel fibrosis, stenosis and occlusion (often microvascular occlusion) with tissue ischaemia ± end-organ injury. The condition may be confined to the skin (cutaneous vasculitis) or may be systemic. Systemic vasculitis is characterised by: In addition there is further classification according to the size and therefore type (elastic versus muscular) of vessel predominantly affected (see Figure 46.1).
Broad Classification
Clinical Picture and Examination
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


