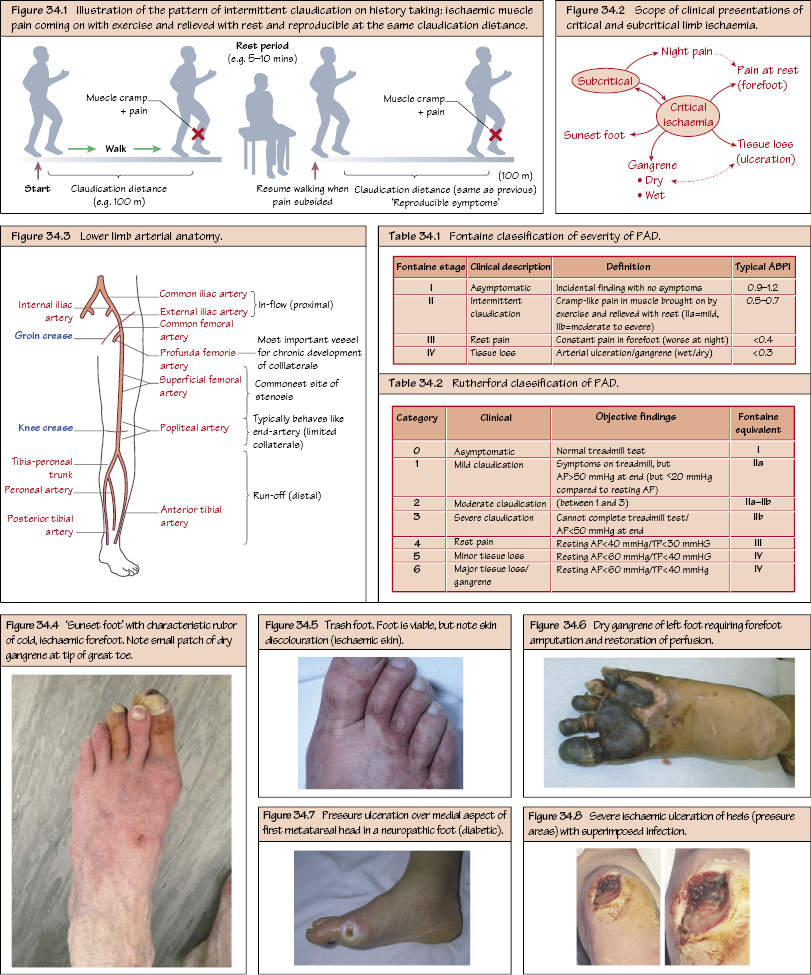
Peripheral Vascular Disease I: Overview Peripheral vascular disease (PVD) is arterial disease that may lead to limb ischaemia. The normal resting oxygen demand in the lower limb is 130–150 mL/min. In symptomatic PVD, there is an imbalance between limb perfusion supply and demand. During exercise the increased metabolic demand by muscle cannot be met, leading to anaerobic metabolism and by-product formation (e.g. lactate) causing ‘cramp-like’ pain. In critical disease, even the resting oxygen demand cannot be met and tissue necrosis ensues. Perfusion pressures are severely reduced (<50 mmHg tibial pressure [<30 mmHg toe pressure]). PVD affects ∼10% of the general population and predominantly affects smokers and/or people with diabetes with a male preponderance. It is also an independent surrogate marker for both coronary and carotid artery disease (i.e. systemic atherosclerosis). These are the same as for atherosclerosis (see Chapter 9) and include smoking, diabetes, hypercholesterolaemia, advancing age, hypertension and hyperhomocystinaemia.
Pathophysiology
Aetiology
Epidemiology
Risk Factors
Clinical Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


